Abstract
We have reported that the platelet intracellular calcium (Ca) mobilization after stimulation by serotonin (5-HT) is specifically enhanced in bipolar disorder among various psychiatric disorders, compared with that in normal control. To explore the mechanisms of enhanced Ca response to 5-HT in the platelets, we first examined the relation between the 5HT-elicited Ca mobilization and 5-HT2A receptor density using the platelets from 13 normal subjects. From this study, we found no significant correlation between two measures. Then, we investigated the effects of staurosporine, a protein kinase C (PKC) inhibitor, on Ca response to 5-HT in platelets from patients with major depressive disorder (unipolar), bipolar disorder, and normal controls. While 5-HT-induced Ca mobilization, in the presence of 100 nM staurosporine, was significantly attenuated in normal controls and patients with major depressive disorder, the inhibitory effect of staurosporine was not observed in bipolar disorder. These results suggest that the failure in inhibiting the platelet intracellular Ca response to 5-HT in bipolar disorder may be related to increased activity of PKC rather than increased 5-HT2A receptor number. Moreover, the trend of the Ca response towards staurosporine may become a specific biological marker for unipolar–bipolar dichotomy.
Similar content being viewed by others
INTRODUCTION
We have reported that serotonin (5-HT)-induced intracellular calcium (Ca) mobilization in platelet is enhanced in drug-naive patients with some types of affective disorders (Kusumi et al, 1991b,1994; Suzuki et al, 2001). Other researchers (Mikuni et al, 1992; Eckert et al, 1993; Okamoto et al, 1994; Tomiyoshi et al, 1999) have obtained similar findings. The enhancement in Ca response to 5-HT continues after remission, which indicates that this response may be a trait-dependent rather than a state-dependent marker (Kusumi et al, 1994; Tomiyoshi et al, 1999). Furthermore, we reported in a naturalistic follow-up study that patients with enhanced Ca mobilization exhibited good response to mood stabilizers such as lithium or valproate (Kusumi et al, 2000). Thus, exploring the mechanism of this enhancement might contribute to our understanding of the underlying pathophysiology of affective disorders.
The 5-HT-induced intracellular Ca mobilization in human platelets was mediated by 5-HT2A receptors (Kagaya et al, 1990; Kusumi et al, 1991a). Stimulation of 5-HT2A receptors in human platelets increases phosphoinositide hydrolysis through Gq type G protein, producing inositol triphosphate, which mobilizes intracellular Ca from internal storage sites (Rittenhouse-Simmons, 1979; Affolter et al, 1984; de Chaffoy de Courcelles et al, 1985). As previously suggested in depressed patients in several studies (Arora and Meltzer, 1989; Pandey et al, 1990; Hrdina et al, 1995; Sheline et al, 1995), one possible explanation for enhanced Ca mobilization stimulated by 5-HT is that increased density of 5-HT2A receptor binding sites in platelets causes larger Ca response to 5-HT. Enhanced Ca mobilization can be also explained by the altered 5-HT2A-receptor function caused by enhanced transduction of stimuli through a postreceptor mechanism, that is, coupling between the receptor and G protein, or regulation of a second- or third-messenger pathway involving protein kinase. Recently, enhanced protein kinase C (PKC) activities in platelet or brain in affective disorders has been observed by some investigators (Friedman et al, 1993; Wang and Friedman, 1996; Pandey et al, 1998; Wang et al, 1999).
In this pilot study, for the purpose of elucidating a relation between the density of 5-HT2A receptors and the degree of intracellular Ca response after 5HT stimulation, we measured these two markers simultaneously in the same blood sample from normal subjects. Furthermore, we examined the effects of staurosporine, a PKC inhibitor, on 5-HT-induced Ca increase in the platelets from not only healthy subjects but also patients with major depressive disorder and bipolar disorder, in order to confirm the involvement of PKC in the enhanced Ca response to 5-HT.
MATERIALS AND METHODS
Materials
Serotonin (5-hydroxytryptamine) creatinine sulfate was purchased from Sigma Chemical Co. (St Louis, MO). [3H]ketanserin (66.4 Ci/mmol) from Dupont New England Nuclear (Boston, MA). Fura-2/acetoxymethyl ester (fura-2/AM) from Dojindo Lab. (Kumamoto, Japan). Staurosporine was kindly donated by Asahi-kasei Co. (Shizuoka, Japan).
Subjects
For the simultaneous measurement of 5-HT2A receptor binding and 5-HT-induced Ca mobilization, subjects were 13 healthy male volunteers, whose mean age (±SEM) was 35.5±7.2 years. For the effects of several doses of staurosporine on Ca response to 5-HT, eight healthy subjects (four men, four women, 30.0±1.8 years) participated in the study. In all, 11 patients with major depressive disorder (six men, five women, 37.4±4.4 years), 10 patients with bipolar disorder (five men, five women, 37.3±3.8 years), and 11 sex- and age-matched normal controls (six men, five women, 38.0±2.5 years) participated in the comparison study. Written informed consent was obtained from all participants prior to blood sampling, which was approved by the Institutional Review Board in Hokkaido University School of Medicine. Patients were all drug-naive outpatients. A total of 10 subjects including two patients in manic episode and eight patients in depressive episode at the time of sampling were diagnosed using DSM-IV criteria as bipolar disorders. Patients who met the DSM-IV criteria for major depressive episode but had never experienced manic or hypomanic episodes were diagnosed as having unipolar major depressive disorder. All normal volunteers did not have any histories of psychiatric illness, family histories, and subsyndromal symptoms at the time of sampling. For at least 4 weeks before blood sampling all subjects had not received drugs such as aspirin that might interfere with platelet aggregation. They were free of physical illness including hypertension at the time of sampling.
Blood Sampling
Blood samples were taken from the antecubital vein and were anticoagulated by the addition of acid citrate dextrose (93 mM sodium citrate, 213 mM citric acid, 111 mM glucose; 1 vol/9 vol of blood).
5-HT2A Receptor Binding Assay
A volume of 63 ml of venous blood taken from a subject was divided into 9 ml for the measurement of intracellular Ca concentration and 54 ml for receptor binding assay. Both experiments were performed simultaneously and started immediately after blood sampling. Isolated platelets were homogenized with a Polytron (setting 6.0) in hypotonic buffer (Tris-Na2 EDTA 5 mM, pH 7.5). Platelet membranes were collected and centrifuged for 20 min at 30 000 g at 4°C. The pellets were washed twice in 50 mM (pH 7.7) Tris-HCl buffer by successive centrifugations for 10 min at 30 000 g at 4°C. The final washed platelet membranes were suspended in the same buffer in a concentration corresponding to 1×109 original platelets/ml.
Incubation mixtures were composed of 0.3 ml platelet membrane preparation, 0.05 ml of incubation buffer (50 mM Tris-HCl, pH 7.7 for total binding), or cold-displacing drug (10 μM methysergide, to define nonspecific binding), 0.05 ml [3H]ketanserin. The incubation was run for 15 min at 37°C. The reaction was terminated by rapid filtration over Whatman GF/B filters presoaked by 0.1% polyethylenimine, which were rinsed twice with ice-cold 50 mM Tris-HCl buffer (pH 7.7 at 25°C) using a 24-well cell harvester (Brandel, USA).
For saturation experiments, six concentrations of [3H]ketanserin (0.1–3.2 nM) were used. The dissociation constant (KD) and density (Bmax) of 5-HT2A receptors were estimated using the nonlinear regression program EBDA/LIGAND.
Measurement of 5-HT-Induced Intracellular Ca Mobilization
The isolation of platelets and the measurement of intracellular Ca concentration were performed as described previously (Kusumi et al, 1991a,1991b,1994). Briefly, platelet-rich plasma (PRP) was prepared by centrifugation at 200 g for 10 min at room temperature. After 15 min incubation with 4 μM fura-2/AM, platelets were isolated from the PRP by further centrifugation at 650 g for 15 min. The resulting platelet pellet was suspended at 1×108 cells/ml in Krebs–Ringer HEPES buffer (145 mM NaCl, 5 mM KCl, 1 mM MgSO4, 0.5 mM Na2HPO4, 6 mM glucose, 10 mM HEPES, 1 mM CaCl2, pH 7.4). The samples were prewarmed in a cuvette at 37°C for 4 min with staurosporine that was dissolved in Krebs–Ringer HEPES buffer or an equivalent volume of Krebs–Ringer HEPES buffer as control, and then 10 μM 5-HT was added to the incubation medium. Fluorescence was measured on a Hitachi F-2000 fluorometer with excitation at 340 and 380 nm, and with emission at 510 nm. Intracellular Ca concentrations were calculated from the ratio of fluorescence intensities at two excitation wavelengths in the platelet samples according to the method of Grynkiewicz et al (1985). We examined the maximum Ca response (Ca increase=initial peak (nM)−resting level (nM)) after stimulation by 5-HT. The intraassay coefficient of variation (CV) was 4.7% and the interassay CV 11.2% as described in the previous report (Kusumi et al, 1991a).
Statistical Analysis
Values are expressed as means±SEM. Pearson's correlations were used to assess the inter-relations between intraplatelet Ca response and the Bmax or KD of 5-HT2A receptors. The effect of several doses of staurosporine on Ca increase was examined using a one-factor repeated measures of ANOVA followed by Dunnet's test. The effect of 100 nM staurosporine on Ca increase for each group was determined with paired t-test. Comparing intracellular Ca response among the three groups, data were analyzed for statistical significance by one-way ANOVA for multiple comparisons followed by Scheffe's test.
RESULTS
In the study investigating the relation between Ca increase and 5-HT2A receptor number, the maximal increase of intracellular Ca concentration after 10 μM 5-HT stimulation ranged from 36.8 to 128 nM with a standard deviation of 31.3 nM. The Bmax of 5-HT2A receptors were from 7.6 to 13.5 fmol/mg protein with a standard deviation of 1.8 fmol/mg protein. The KD of 5-HT2A receptors ranged from 0.24 to 0.84 nM with a standard deviation of 0.16 nM. There were no significant correlations between the magnitude of 5-HT-induced Ca response and the Bmax (r=0.109, p=0.730) (Figure 1) or KD (r=0.386, p=0.198) of 5-HT2A receptors.
As shown in Figure 2, there is no remarkable change in 5-HT-induced Ca increase when preincubated with staurosporine at lower concentrations than 10 nM, while Ca increases induced by 5-HT were significantly reduced when platelets were incubated in the presence of 100 nM or 1 μM staurosporine compared with those in the absence of staurosporine (control) (72.3% of control for 100 nM, 64.9% of control for 1 μM staurosporine, p<0.01 for each dose).
Effect of preincubation with staurosporine on 10 μM 5-HT-induced platelet intracellular Ca mobilization. Platelet suspension was prewarmed for 4 min in the presence of various concentrations of staurosporine. One-factor repeated measures of ANOVA was performed to analyze an effect of staurosporine. Significant modulating action of staurosporine was observed on 5-HT-induced Ca response (df=4, F=11.6, N=8, p<0.0001). *p<0.01 compared with the data in the absence of staurosporine; calculated by Dunnett's test.
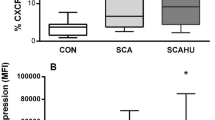
There was no significant difference in 5-HT-induced Ca increase between the three groups (df=2, F=0.275, p=0.761: 91.7±6.4 nM for normal controls; 94.7±5.9 nM for patients with major depressive disorder; 99.3±9.2 nM for patients with bipolar disorder). In the presence of 100 nM staurosporine, Ca increases elicited by 5-HT in not only normal control but also major depressive disorder were markedly lower than that in the absence of staurosporine (vehicle) (71.2±3.8% of vehicle, p<0.0001 for normal control; 74.0±5.7% of vehicle, p=0.0017 for major depressive disorder) (Figure 3). However, 5-HT-induced Ca mobilization in bipolar disorder was not changed when preincubated with 100 nM staurosporine (102.0±8.1% of vehicle, p=0.5888) (Figure 3).
Effect of 100 nM staurosporine on 5-HT-induced Ca increase in the platelets with normal controls and unmedicated patients with affective disorders. Platelet suspensions from the same individual were prewarmed for 4 min in the presence or absence (which is mentioned as vehicle) of 100 nM staurosporine. Paired t-test was performed to determine the effect of 100 nM staurosporine. #p=0.0001 for normal control (N=11); ##p=0.0017 for major depressive disorder (N=11); nonsignificant (NS) effect observed in bipolar disorder (N=10).
DISCUSSION
Several investigators have indicated increased 5-HT2A receptor density in the frontal cortex (McKeith et al, 1987; Yates et al, 1990) or in the platelets (McBride RA et al, 1983; Biegon et al, 1987; Arora and Meltzer, 1989; Pandy et al, 1990; Hrdina et al, 1995; Sheline et al, 1995) of depressed patients. However, these findings have not always been confirmed (Cowen et al, 1987; Cheetham et al, 1988; McBride et al, 1994; Neuger et al, 1999). The number of platelet 5-HT2A binding sites in manic subjects has also been reported to be the same as in controls (Velayudhan et al, 1999). Furthermore, decreased 5-HT2A receptors in frontal cortex in drug-free depressed patients has been observed in a positron emission tomography (PET) study (Biver et al, 1997; Attar-Levy et al, 1999; Yatham et al, 2000). Biegon et al (1990) suggested that 5-HT2A receptor binding on blood platelet is a state-dependent marker in depression. Thus, it is possible that the density of 5-HT2A receptors might change in the clinical course of affective disorders. It is reported, as mentioned above, that Ca response to 5-HT in the platelet could be a trait-dependent rather than a state-dependent value (Kusumi et al, 1994; Tomiyoshi et al, 1999). In the present study, no positive correlation between the density of 5-HT2A receptors and intracellular Ca response to 5-HT was found in platelets with normal subjects. This result suggests that the number of 5-HT2A receptors may not influence platelet intracellular Ca mobilization after 5-HT stimulation. Therefore, even in the case of the platelets of affective disorders, it is unlikely that increased Ca response to 5-HT may be because of the number of 5-HT2A binding sites. Further studies are required to investigate the correlation between the two measures in the platelet of patients with affective disorders. Ca mobilization elicited by thrombin has been also reported to be enhanced in platelets with bipolar disorder, but not in unipolar depressive disorder (Dubovsky et al, 1991; Kusumi et al, 1992). Thus, there might be some alterations in intracellular signal transduction in platelets with bipolar disorder that are common to both the 5-HT- and thrombin-induced Ca mobilizing pathways, which is not influenced by the density of 5-HT2A receptors.
Although we failed to observe the difference in 5-HT-induced platelet intracellular Ca increase between patients and controls in this study, we showed apparent higher Ca response to 5-HT in bipolar disorder than unipolar depression and normal control in the presence of staurosporine. Two reasons can be considered for the failure in this study to produce the difference in 5-HT-elicited Ca mobilization among three groups in the absence of staurosporine.
First, the sample number examined in this study is relatively small compared with the previous report. The Ca mobilization in bipolar disorder was larger than that in control and unipolar depression, but it was not statistically significant. Enhanced platelet intracellular Ca response to 5-HT in untreated affective disorder is a relatively common finding except one report (Bothwell et al, 1994). In our previous report, both unipolar and bipolar disorder patients showed higher Ca response to 5-HT compared with control (Kusumi et al, 1994). However, the Ca mobilization in patients whose diagnoses have changed from unipolar depression to bipolar disorder, during the follow-up for a period of 8–10 years, was significantly higher than in patients whose diagnoses remain unipolar depression (Suzuki et al, 2001).
Second, we intended to choose control subjects in this study who had showed relatively high Ca response to 5-HT in the previous trial, for the purpose of defining the pathophysiology of bipolar disorder. Although the Ca response in the platelet induced by 5-HT is a stable biological index (Kusumi et al, 1991a), there exists some normal subjects whose Ca response show relatively high value to a degree of bipolar disorder patients. In other words, even if relatively high response to 5-HT is obtained in the platelets from normal control and major depressive disorder, we may be able to clarify whether the diagnosis of the subject is bipolar disorder or not, by means of preincubating platelets with staurosporine.
Staurosporine, a nonspecific protein kinase inhibitor, is often used as a PKC inhibitor because it is reported to inhibit PKC at the nanomolar level (Tamaoki et al, 1986). Half maximal concentration of staurosporine to inhibit purified PKC activity interacting with the ATP-binding site has been reported to be 2–6 nM (Tamaoki et al, 1986; Meyer et al, 1989; Asano et al, 1995). Staurosporine at a concentration lower than 100 nM had no remarkable effect on 5-HT-induced platelet intracellular Ca increase in the present study. Human platelets contain α-, β-, δ-, and ζ-PKC isozymes (Wang et al, 1999). In these isozymes, the activity of purified ζ-PKC is reported to be not sufficiently inhibited by staurosporine at concentrations lower than 100 nM (Geiges et al, 1997). Wang and Friedman (1996,2001) suggested that membrane-associated ζ-PKC was elevated in bipolar disorder brains. If ζ-PKC are related to the mechanism of agonist-induced Ca mobilization, inhibition of this isozyme may be responsible for reduced Ca mobilization by staurosporine at concentrations higher than 100 nM, that is demonstrated in platelets from normal subjects, and increased activity of this isozyme in bipolar disorder patients may prevent this inhibitory effect of 100 nM staurosporine. However, staurosporine at 100 nM can also inhibit cyclic AMP-dependent protein kinase (PKA), phosphorylase kinase, tyrosin kinase, and other kinases (Meyer et al, 1989). And 5-HT has been reported not to translocate ζ-PKC in platelets from cytosol to membrane (Wang et al, 1999). The precise mechanism of inhibitory effect of 100 nM staurosporine on Ca mobilization observed in this study remains to be complicated. Staurosporine at 100 nM seems at least to act on the protein related to the regulation of Ca release from intracellular Ca storage site and decrease the Ca mobilization, because with preincubation with 100 nM staurosporine, 5-HT-induced Ca mobilization also reduced in the absence of external Ca in healthy subjects (62.8% of control) (data not shown).
In conclusion, this study suggests that enhanced 5-HT-induced platelet intracellular Ca mobilization in bipolar disorder may have a relation with increased activity of PKC rather than increased 5-HT2A receptor number. And there is a possibility that measurement of platelet intracellular Ca response both in the absence and presence of staurosporine could be a specific biological marker for unipolar–bipolar dichotomy.
References
Affolter H, Erne P, Buergisser E, Pletscher A (1984). Ca2+ as messenger of 5HT2-receptor stimulation in human blood platelets. Naunyn-Schmiedeberg's Arch Pharmacol 325: 337–342.
Arora RC, Meltzer HY (1989). Increased serotonin2 (5-HT2) receptor binding as measured by 3H-lysergic acid diethylamide (3H-LSD) in the blood platelets of depressed patients. Life Sci 44: 725–734.
Asano M, Matsunaga K, Miura M, Ito KM, Seto M, Sakurada K et al (1995). Selectivity of action of staurosporine on Ca2+ movements and concentrations in vascular smooth muscles. Eur J Pharmacol 294: 693–701.
Attar-Levy D, Martinet JL, Bin J, Dao-Castellana MH, Crouzel C, Mazoyer B et al (1999). The cortical serotonin2 receptors studied with positron-emission tomography and [18F]setoperone during depressive illness and antidepressant treatment with clomipramine. Biol Psychiatry 15: 180–186.
Biegon A, Essar N, Israeli M, Elizur A, Bruch S, Bar-Nathan AA (1990). Serotonin 5-HT2 receptor binding on blood platelets as a state dependent marker in major affective disorder. Psychopharmacology 102: 73–75.
Biegon A, Weizman A, Karp L, Ram A, Tiano S, Wolff M (1987). Serotonin 5-HT2 receptor binding on blood platelets: a peripheral marker for depression? Life Sci 41: 2485–2492.
Biver F, Wikler D, Lotstra F, Damhaut P, Goldman S, Mendlewicz J (1997). Serotonin 5-HT2 receptor imaging in major depression: Focal changes in orbitor-insular cortex. Br J Psychiatry 171: 444–448.
Bothwell RA, Eccleston D, Marshall E (1994). Platelet intracellular calcium in patients with recurrent affective disorders. Psychopharmacology 114: 375–381.
Cheetham SC, Crompton MR, Katona CLE, Horton RW (1988). Brain 5-HT2 receptor binding sites in depressed suicide victims. Brain Res 443: 272–280.
Cowen PJ, Charig EM, Fraser S, Elliott JM (1987). Platelet 5-HT receptor binding during depressive illness and tricyclic antidepressant treatment. J Affect Disord 13: 45–50.
de Chaffoy de Courcelles D, Leysen JE, De Clerck F, Van Belle H, Janssen PA (1985). Evidence that phospholipid turnover is the signal transducing system coupled to serotonin-S2 receptor sites. J Biol Chem 260: 7603–7608.
Dubovsky SL, Lee C, Christiano J, Murphy J (1991). Elevated platelet intracellular calcium concentration in bipolar depression. Biol Psychiatry 29: 441–450.
Eckert A, Riemann GD, Aldenhoff J, Mueller WE (1993). Elevated intracellular calcium levels after 5-HT2 receptor stimulation in platelets of depressed patients. Biol Psychiatry 34: 565–568.
Friedman E, Wang HY, Levinson D, Connel TA, Singh H (1993). Altered platelet protein kinase C activity in bipolar affective disorder, manic episode. Biol Psychiatry 33: 520–525.
Geiges D, Meyer T, Marte B, Vanek M, Weissgerber G, Stabel S et al (1997). Activation of protein kinase C subtypes α, γ, δ, ɛ, ζ, and η by tumor-promoting and nontumor-promoting agents. Biochem Pharmacol 53: 865–875.
Grynkiewicz G, Poenie M, Tsien RY (1985). A new generation of Ca2+ indicators with greatly improved fluorescence properties. J Biol Chem 260: 3440–3450.
Hrdina PD, Bakish D, Chudzik J, Ravindran A, Lapierre I (1995). Serotonergic markers in platelets with major depression: upregulation of 5-HT2 receptors. J Psychiatr Neurosci 20: 11–19.
Kagaya A, Mikuni M, Yamamoto H, Takahashi K (1990). Serotonin-induced acute desensitization of serotonin2 receptors in human platelets via a mechanism involving protein kinase C. J Pharmacol Exp Ther 255: 305–311.
Kusumi I, Koyama T, Yamashita I (1991a). Effect of various factors on serotonin-induced Ca2+ response in human platelets. Life Sci 48: 2405–2412.
Kusumi I, Koyama T, Yamashita I (1991b). Serotonin-stimulated Ca response is increased in the blood platelets of depressed patients. Biol Psychiatry 30: 310–312.
Kusumi I, Koyama T, Yamashita I (1992). Thrombin-induced platelet calcium mobilization is enhanced in bipolar disorder. Biol Psychiatry 32: 731–734.
Kusumi I, Koyama T, Yamashita I (1994). Serotonin-induced platelet intracellular calcium mobilization in depressed patients. Psychopharmacology 113: 322–327.
Kusumi I, Suzuki K, Sasaki Y, Takahashi Y, Kameda K, Koyama T (2000). Treatment response in depressed patients with enhanced calcium mobilization stimulated by serotonin. Neuropsychopharmacology 23: 690–696.
McBride PA, Brown RP, DeMeo M, Kelip J, Mieczkwoski T, Mann JJ (1994). The relationship of platelet 5-HT2-receptor indices to major depression disorder, personality traits and suicidal behavior. Biol Psychiatry 35: 295–308.
McBride PA, Mann JJ, McEwen B, Biegon A (1983). Characterization of serotonin binding sites on human platelets. Life Sci 33: 2033–2041.
McKeith IG, Marshall EF, Ferrie IN, Armstrong MM, Kennedy WN, Perry RH et al (1987). 5-HT receptor binding in post-mortem brain from patients with affective disorder. J Affect Disord 13: 67–74.
Meyer T, Regenass U, Fabbro D, Alteri E, Rosel J, Muller M et al (1989). A derivative of staurosporine (CGP 41 251) shows selectivity for protein kinase C inhibition and in vitro anti-proliferative as well as in vivo anti-tumor activity. Int J Cancer 43: 851–856.
Mikuni M, Kagaya A, Takahashi K, Meltzer HY (1992). Serotonin but not norepinephrine-induced calcium mobilization of platelets is enhanced in affective disorders. Psychopharmacology 106: 311–314.
Neuger J, El Khoury A, Kjellman BF, Wahlund B, Aberg-Wistedt A, Stain-Malmgren R (1999). Platelet serotonin functions in untreated major depression. Psychiatry Res 85: 189–198.
Okamoto Y, Kagaya A, Shinno H, Motohashi N, Yamawaki S (1994). Serotonin-induced platelet calcium mobilization is enhanced in mania. Life Sci 56: 327–332.
Pandey GN, Dwivedi Y, Kumari R, Janicak PG (1998). Protein kinase C in platelets of depressed patients. Biol Psychiatry 44: 909–911.
Pandey GN, Pandey SC, Janicak PG, Marks RC, Davis JM (1990). Platelet serotonin-2 receptor binding sites in depression and suicide. Biol Psychiatry 28: 215–222.
Rittenhouse-Simmons S (1979). Production of diglyceride from phosphatidylinositol in activated human platelets. J Clin Invest 63: 580–587.
Sheline YI, Bardgett ME, Jackson JL, Newcomer JW, Csernansky JG (1995). Platelet serotonin markers and depressive symptomatology. Biol Psychiatry 37: 442–447.
Suzuki K, Kusumi I, Sasaki Y, Koyama T (2001). Serotonin-induced platelet intracellular calcium mobilization in various psychiatric disorders: is it specific to bipolar disorder? J Affect Disord 64: 291–296.
Tamaoki T, Nomoto H, Takahashi I, Kato Y, Morimoto M, Tomita F (1986). Staurosporine, a potent inhibitor of phospholipid/Ca2+ dependent protein kinase. Biochem Biophys Res Commun 135: 397–402.
Tomiyoshi R, Kamei K, Muraoka S, Muneoka K, Takigawa M (1999). Serotonin-induced intracellular Ca2+ responses in untreated depressed patients and imipramine responders in remission. Biol Psychiatry 45: 1042–1048.
Velayudhan A, Sunitha TA, Balachander S, Reddy JYC, Khanna S (1999). A study of platelet serotonin receptor in mania. Biol Psychiatry 45: 1059–1062.
Wang H-Y, Friedman E (1996). Enhanced protein kinase C activity and translocation in bipolar affective disorder brains. Biol Psychiatry 40: 568–575.
Wang H-Y, Friedman E (2001). Increased association of brain protein kinase C with the receptor for activated C kinase-1 (RACK1) in bipolar affective disorder. Biol Psychiatry 50: 364–370.
Wang H-Y, Markowitz P, Levinson D, Undie AS, Friedman E (1999). Increased membrane-associated protein kinase C activity and translocation in blood platelets from bipolar affective disorder patients. J Psychiatr Res 33: 171–179.
Yates M, Leake A, Candy JM, Fairbrairn AF, McKieth IG, Ferrier IN (1990). 5-HT2 receptor changes in major depression. Biol Psychiatry 27: 489–496.
Yatham LN, Liddle PF, Shiah I, Scarrow G, Lam RW, Adam MJ et al (2000). Brain serotonin2 receptors in major depression: a positron emission tomography study. Arch Gen Psychiatry 57: 850–858.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suzuki, K., Kusumi, I., Akimoto, T. et al. Altered 5-HT-Induced Calcium Response in the Presence of Staurosporine in Blood Platelets from Bipolar Disorder Patients. Neuropsychopharmacol 28, 1210–1214 (2003). https://doi.org/10.1038/sj.npp.1300159
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300159
Keywords
This article is cited by
-
Reelin is a platelet protein and functions as a positive regulator of platelet spreading on fibrinogen
Cellular and Molecular Life Sciences (2010)
-
Serotonin-induced decrease of intracellular Ca2+ release in platelets of bulimic patients normalizes during treatment
Journal of Neural Transmission (2009)