Abstract
The rat medial prefrontal cortex (mPFC) regulates subcortical dopamine transmission via projections to the striatum and ventral tegmental area. We used in vivo proton magnetic resonance spectroscopy (1H-MRS) at 4.7 T to determine whether excitotoxic lesions of the mPFC result in alterations of N-acetylaspartate (NAA), a marker of neuronal integrity, both locally and downstream in the striatum. Lesioned rats exhibited persistent reductions of NAA and other metabolites within the prefrontal cortex; selective reductions of NAA were seen in the striatum, but not in the parietal cortex. Consistent with earlier reports, lesioned rats exhibited a transient enhancement in amphetamine-induced hyperlocomotion. Prefrontal NAA losses correlated with lesion extent. In the striatum, while there was no change in tissue volume, expression of striatal glutamic acid decarboxylase-67 mRNA was significantly reduced. In vivo NAA levels thus appear sensitive to both local and downstream alterations in neuronal integrity, and may signal meaningful effects at cellular and behavioral levels.
Similar content being viewed by others
Main
Dysfunction of the prefrontal cortex has been consistently implicated in neuropsychological and functional neuroimaging studies of patients with schizophrenia (Weinberger et al. 1986; Weinberger 1987; Andreasen et al. 1994; Goldberg and Gold 1995; Carter et al. 1998; Fletcher et al. 1998; Callicott et al. 1998, Manoach et al. 1999). Postmortem studies have demonstrated alterations in cell-packing density (Selemon et al. 1995), cortical thickness (Pakkenberg 1987), and markers of glutamate metabolism (Tsai and Coyle 1995; Tsai et al. 1995) in the prefrontal cortex. The efficacy of neuroleptic medications in ameliorating certain positive symptoms (Peroutka and Snyder 1980), and of dopamine agonists in exacerbating these symptoms (Lieberman et al. 1987), has long contributed to the idea that dopamine dysregulation may underlie part of the pathophysiology of schizophrenia.
Speculation that such prefrontal and dopaminergic dysfunction are related (Weinberger 1987; Davis et al. 1991; Grace 1991) has been supported by recent work in patients and in monkeys which indicated that neuronal pathology in the dorsolateral prefrontal cortex may cause dysregulated release of subcortical dopamine (Saunders et al. 1998; Bertolino et al. 1999). In the latter of these studies (Bertolino et al. 1999), neuronal pathology in the prefrontal cortex has been inferred from the measurement of N-acetylaspartate (NAA) signals with proton magnetic resonance spectroscopy (1H-MRS). NAA, the second most abundant amino acid in the brain next to glutamate, is a neuron-specific molecule (Urenjak et al. 1993) which is thought to be a marker of neuronal integrity. This measure has been shown to be reduced in several recent in vivo studies of patients with schizophrenia (Nasrallah et al. 1994; Bertolino et al. 1996, 1998; Yurgelun-Todd et al. 1996) as well as other neuropsychatric disorders (for a review see Tsai and Coyle 1995).
Work in rodents has elucidated the regulatory role of the prefrontal cortex in subcortical dopamine transmission. The rat medial prefrontal cortex (mPFC) sends monosynaptic projections to the ventral tegmental area (VTA), caudate nucleus, and nucleus accumbens (Sesack et al. 1989; Takagishi and Chiba 1991; Sesack and Pickel 1992; Gerfen and Wilson 1996; Gorelova and Yang 1997). Glutamate injections into the prefrontal cortex or direct electrical stimulation of the mPFC increases firing of VTA neurons and enhances release of dopamine in the nucleus accumbens (Murase et al. 1993; Taber and Fibiger 1995); moreover, excitatory amino acid antagonists infused into the VTA block prefrontal-mediated striatal dopamine release, suggesting that the PFC exerts a tonic excitatory control of striatal dopamine via the substantia nigra/VTA (Taber et al. 1995; Karreman and Moghaddam 1996). However, lesions or pharmacologic manipulations of mPFC inputs to these downstream targets result in abnormal locomotor behaviors and changes in firing characteristics of VTA dopaminergic neurons in response to stimuli (Jaskiw et al. 1990; Murase et al. 1993).
The present study was conducted to determine whether both local and downstream cellular changes might be detected in vivo following excitotoxic lesions in the prefrontal cortex. We examined whether lesions of the rat medial prefrontal cortex result in NAA alterations, as assessed with 1H-MRS at 4.7 Tesla, both within the mPFC and downstream in the striatum. To determine whether striatal NAA alterations seen in vivo are associated with functional changes in postsynaptic neurons, we performed in situ hybridization histochemistry to glutamic acid decarboxylase-67 (GAD-67) mRNA in striatal sections. GAD-67 is an enzyme in the GABA synthesis pathway (Cooper et al. 1991), and its message is used here as a functional marker of GABAergic neurons, which comprise the majority of neuronal cell bodies in the striatum (Gerfen and Wilson 1996). Finally, we have also examined whether an association exists between NAA alterations in the prefrontal-striatal circuit and changes in dopamine-related activity, as assessed by amphetamine-induced locomotion.
MATERIALS AND METHODS
Animal Care and Surgery
Animals were handled in accordance with NIH Animal Research Advisory Committee guidelines for the use and care of laboratory animals. Adult male Sprague-Dawley rats weighing approximately 300 g (Harlan Labs) were paired and housed in cages with a 12-hour light-dark cycle and free access to food and water. After anesthesia with Equithesin (3 ml/kg, i.p.) rats were immobilized in a stereotaxic frame (Kopf Instruments) with the incisor bar set at 2.5 mm below the interaural line. Rats in the lesion group (n = 11) were infused with ibotenic acid (Sigma, 7 μg/0.7 μl over 3.5 minutes) bilaterally into the mPFC (coordinates AP +3.5 and ML ± 0.7 mm relative to bregma, DV −3.5 mm relative to dura) through 26-gauge stainless steel canulae. Rats in the sham group (n = 8) received similar infusions of artificial cerebrospinal fluid. Rats were then returned to their home cages, grouped 2–3 per cage by lesion status, and allowed two weeks to recover.
Behavioral Testing
Two and eight weeks following surgery, locomotor activity was assessed during the light phase of the light-dark cycle by individual placement in Plexiglas cages with photocell monitors (Omnitech; model RXYZCM). After a habituation period of 60 minutes, rats were injected with saline (1 ml/kg, i.p.) and monitored for an additional 60 minutes. Rats were then given injections of d-amphetamine sulfate (RBI, 1.5 mg/kg, i.p) and monitored for an additional 90 minutes. Locomotor activity (total distance traveled) was assessed in 5-minute intervals over the entire testing period. Four animals in the lesion group were excluded from the 2-week behavioral analysis due to the failure of one batch of d-amphetamine to increase locomotion above baseline in any animal. In addition, one animal in the sham group was not tested at two or eight weeks because it was unavoidably housed by itself (thus, the final n = 7 in each group).
In Vivo NMR Spectroscopy
Rats underwent in vivo NMR spectroscopy one day after each behavioral testing session (two and eight weeks post-surgery). Rats were anesthetized with 10:1 ketamine:xylazine (100 mg/ml, i.p.) and maintained under the same anesthesia throughout scanning via a 22-gauge i.p catheter. Following insertion into a 1-meter-long plastic tray assembly and placement of a 20-mm-diameter circular surface coil centered above the cranium, rats were positioned in a 4.7 Tesla Varian INOVA horizontal bore magnet with a 120 mm, 310 mTesla/meter gradient coil. The surface coil was tuned for 1H and global shimming was performed. Two-millimiter-thick sagittal and coronal scout images (GEMS, TR = 300 msec, TE = 25 msec) were acquired through the regions of interest (identified using the atlas of Paxinos and Watson 1986), with slices passing through planes 4.7, 2.7, and 0.7 mm anterior to bregma, and 1.3 mm posterior to bregma.
Localized shimming was performed and spectra were acquired from voxels in bilateral prefrontal cortex and the left anterior striatum (in a subset of five sham and seven lesioned animals) using STEAM 1H-MRS (TR = 3 sec, TE = 12 msec). The prefrontal voxel, centered in the plane of the second coronal slice, was acquired with the dimensions x = 4 mm, y = 3 mm, z = 3 mm. The center of the striatal voxel, with dimensions x = 4 mm, y = 4 mm, z = 2 mm, was positioned in the z-plane 2.5 mm posterior to the prefrontal voxel, resulting in maximal anatomical coverage of the anterior striatum with no overlap of the prefrontal voxel. In addition, 1H-MRS from the right parietal cortex (x = 2 mm, y = 4 mm, z = 4 mm) was acquired as a control area at two weeks.
Because absolute measures of 1H-MRS metabolites are influenced by various technical parameters including transmit gain and receiver settings, MRS signals are commonly measured as ratios of one metabolite over another. However, due to the expected decrease of all metabolites in the mPFC following the excitotoxic lesion, the former approach was invalid in the present study. Therefore, after shimming, the signal of water was acquired for use as an internal standard. At such a short echo time the contribution of CSF to the signal of water is very minimal (see also results). Following acquisition of the water signal, water-suppression pulses (CHESS) were switched on and other metabolites were obtained, including NAA, choline-containing compounds (Cho), creatine plus phosphocreatine (Cre), and glutamate, glutamine, and GABA (identified as one peak, tGlx). Total acquisition time for the water-suppressed spectra was 26 minutes per voxel. Respiration rate and core body temperature were monitored throughout the experiment.
Spectra were analyzed by a rater blind to lesion status using Varian software. Spectral peaks were integrated to obtain the absolute metabolite signals for unsuppressed water (4.8–4.6 ppm), Cho (3.3–3.1 ppm), Cre (3.1–2.9 ppm), tGlx (2.4–2.2), and NAA (2.1–1.9). Metabolite values are reported as ratios of absolute metabolite signals to the unsuppressed water signal.
Tissue Preparation
Following the second scan rats were decapitated; brains were collected, rapidly frozen in isopentane, and stored at −80°C. Twenty-micron-thick coronal sections through the prefrontal cortex and striatum were cut using a cryostat and collected on double gelatin-subbed slides. Representative sections were Nissl-stained for histological analysis of the lesion and for striatal size analysis.
Histology
Lesion size in the prefrontal cortex was evaluated by a rater blind to all other measures. Each lesion was rated on a scale from 1 (small) to 5 (large) in terms of both medial-lateral and anterior-posterior extent. These two scores were summed to produce an overall lesion size rating for each lesioned rat.
Nissl-stained coronal sections through the striatum were examined for any evidence of direct incidental neurotoxic damage. To examine striatal size, striatal sections were then matched for rostral-caudal position and scanned into a Macintosh computer. With the aid of an atlas (Paxinos and Watson 1986), left striatal area was traced by a rater blind to lesion status using NIH Image software. Slices were sampled from four rostral-to-caudal striatal regions separated by 200 microns each; four consecutive slices were averaged in each region (total n = 16 slices measured per rat).
In Situ Hybridization
Slices through the anterior and middle part of the striatum (corresponding to Plates 11 and 14, respectively) (Paxinos and Watson 1986) were used for in situ hybridization with an antisense riboprobe to glutamic acid decarboxylase-67 (GAD-67) mRNA. A 3.2 kilobase-pair-containing clone (a gift from Dr. Kalpana Merchant, Pharmacia & Upjohn, Inc.) was linearized with Bam HI restriction enzyme; 0.2 ng (1 μl) of linearized plasmid was labeled using 150 μCi of [35S]dUTP and 1 μl T7 RNA polymerase (for a sense probe Sol I enzyme and T3 polymerase were used). The total volume of this reaction was 10 μl (1 μl each of 10 mM rATP, rCTP, rGTP, 2 μl of 5X transcription buffer, 1 μl of 100 mM dithiothreitol, 1 μl of RNAsin, and 1 μl DEPC water).
After incubation for 15 min at 37°C, the labeled RNA was precipitated with ethanol in the presence of tRNA and ammonium acetate. After extraction with phenol/chloroform and precipitation with ethanol, the probe (specific activity 3.2 x 109 dpm/μg) was resuspended in DEPC water, and added to the hybridization buffer (1200 nM NaCl, 20 mM Tris-HCl, 0.04% Ficoll, 0.04% BSA, 0.04% PVP, 2 mM pH 8 EDTA, 0.02% salmon sperm, 0.1% total yeast RNA, 0.01% yeast tRNA, 20% dextran sulfate) to yield the final concentration of 5 ng/ml corresponding to approximately 5 x 105 dpm per section (per 25 μl). The sections were fixed in 4% formaldehyde, acetylated using acetic anhydride, dehydrated in ethanol, and defatted in chloroform.
In situ hybridization was carried out overnight at 55°C. After removing the coverslips in 2 X SSC, the sections were treated with RNase A for 30 min at 37°C, washed in RNase-free buffer for 30 min at 37°C, washed twice in 2 X SSC for 15 minutes each at room temperature, once in 0.5 X SSC for 60 min at 55°C, twice in 0.1 X SSC for 30 min at 60°C, and once in 0.1 X SSC for 15 minutes at room temperature. The sections were then rinsed with 50% to 100% ethanol solutions with ammonium acetate (300 mM), air-dried, and apposed with 14C standards to Kodak BioMax film for three days.
Densitometric analysis of films was performed blind to lesion status using NIH Image software. Optical densities were assessed for the whole striatal regions as well as subdivisions of the striatum (dorsolateral and medial striatum, nucleus accumbens core and shell) according to Paxinos and Watson (1986) from four anterior sections per rat, and averaged; the same was done for more posterior sections taken from mid-striatum. Densities interpolated along a 14C standard curve were converted to disintegrations per min/mm squared (24 dpm/mm2 for every μCi/g of 14C).
Statistical Analysis
Analysis was conducted using Statistica, Version 5 (StatSoft, Inc.). Group means for lesioned and sham animals were compared using unpaired T-tests assuming unequal variance for behavior, in vivo spectroscopy, and in situ hybridization measures. Correlation between prefrontal NAA levels and mPFC lesion size was evaluated using Spearman's Rho. Level of significance was set at p < .05.
RESULTS
Behavioral Testing
When assessed two weeks following surgery, lesioned and sham rats did not differ in total distance traveled in response to novelty or saline injection (Figure 1a). However, lesioned animals exhibited significantly greater amphetamine-induced hyperlocomotion (t[12] = 2.67, p < .05). When animals were retested six weeks later, no differences were found between groups in response to novelty, saline, or amphetamine (Figure 1b).
Total distance traveled by rats with prefrontal lesions (solid bars) or sham surgery (open bars) after exposure to novelty (NOV), saline injection (SAL), and amphetamine (AMPH). Two weeks after surgery (A), lesioned rats exhibited significantly greater amphetamine-induced hyperlocomotion than sham animals, but this difference disappeared by eight weeks (B). *p < .05; in this and following figures, error bars indicate standard deviation
In Vivo NMR Spectroscopy
A typical spectrum and structural images through the regions of interest are illustrated in Figure 2. Two weeks following surgery, lesioned rats exhibited reductions of all metabolites in the mPFC compared to sham animals (Figure 3a) (Cho: t[17] = 1.87, p = .07; Cre: t[17] = 3.03, p< .01; tGLX: t[17] = 2.70, p < .05; NAA: t[17] = 4.21, p< .001). The mean difference in NAA (38%) was the greatest between groups. No differences in the signal of the unsuppressed water peak were observed (mean ± standard deviation: lesion, 1202 ± 236; sham, 1339 ± 351; t[17] = −1.02, p = .32, graph not shown). Downstream in the striatum, the only metabolite significantly altered by the prefrontal lesion was NAA, which exhibited a mean 13% reduction (Figure 3b) (NAA: t[10] = 2.79, p < .05). No differences were seen between groups in any metabolite in the parietal cortex (Figure 3c).
(A) Typical spectrum acquired with in vivo 1H-MRS indicating peaks for choline (Cho), creatine (Cre), glutamate/glutamine/GABA (tGLX), and n-acetylaspartate (NAA). Scale is parts per million. Below are structural images taken from the mPFC (B, lesion visible), striatum (C), and parietal cortex (D) indicating spectroscopy voxel boundaries
Metabolite ratios obtained with in vivo 1H-MRS two weeks after surgery. Among lesioned rats all metabolites were reduced in the prefrontal cortex (A), with NAA exhibiting the most significant change. In the striatum (B) the only metabolite significantly altered by the prefrontal lesion was NAA. No changes were observed in the parietal cortex (C). Open bars: sham, solid bars: lesion; *p = .07, **p < .05, ***p < .01, ****p < .001
To assess the stability of these findings over time, rats were studied again eight weeks following surgery. One rat in each treatment condition died prior to the second set of scans. Among re-tested rats, NAA reductions persisted in both the prefrontal cortex (Figure 4a) (NAA: t[15] = 3.99, p < .001) and striatum (Figure 4b) (NAA: t[10] = 2.00, p < .05, one-tailed). The mean difference in the striatum between groups at 8 weeks was 19%.
Histology
Postmortem analysis of 20-micron-thick sections through the mPFC indicated medium- to large-sized lesions with some central cavitation (Figure 5). Affected areas were confined to the cingulate cortex (area 1), medial orbital cortex, prelimbic cortex, infralimbic cortex, and in larger lesions, dorsal peduncular cortex. A negative correlation was found between lesion size and NAA signals, indicating that the larger the lesion, the greater the extent of NAA reduction (Figure 6) (Spearman's Rho = −0.59, p = .05). There was no correlation between lesion size and any other metabolite signal in the mPFC (p > .7 for each of Cho, Cre, and tGlx).
Boundaries of largest (shaded) and smallest (striped) lesions. Although lesions were bilateral, only the left side is drawn so that the anatomy may be appreciated on the right. Coordinates refer to distance in millimeters anterior to bregma. PrL = prelimbic cortex; MO = medial orbital cortex; Cg1 = cingulate cortex area 1; IL = infralimbic cortex; DP = dorsal peduncular cortex. Figure adapted from Paxinos and Watson (1986)
Microscopic examination of Nissl-stained sections through the striatum indicated no evidence of neurotoxic damage. To determine whether striatal NAA reductions reflected gross tissue shrinkage, striatal size was compared between groups. No difference in striatal size was found (sum of cross-sectional areas in sham, 12.78 ± 0.52 cm2; lesion, 12.47 ± 0.48 cm2; t[17] = 1.35, p = .19, graph not shown).
In Situ Hybridization
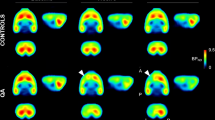
Examination of GAD-67 mRNA expression in the left anterior striatum revealed a mean 29% reduction in the lesioned animals (Figure 7) (t[15] = 2.63, p< .05). More posterior sections of the striatum, which receive less prefrontal afferentation (Sesack et al. 1989), did not differ in GAD-67 mRNA expression between groups.
Striatal GAD-67 mRNA expression, as indicated by in situ hybridization, in lesioned and sham rats. In sections through the anterior striatum (A), GAD-67 mRNA was significantly reduced in the whole striatum (WHOLE), as well as in dorsolateral striatum (DL STR), medial striatum (MED STR), accumbens core (NAC) and accumbens shell (NAS) regions, in rats with mPFC lesions. In more posterior sections (B), no differences between groups were found. Open bars: sham, solid bars: lesion; *p < .05
DISCUSSION
Our findings confirm that 1H-MRS may be useful in the detection of both local and downstream sequelae of neuronal injury in vivo. Two weeks following excitotoxic lesions of the mPFC, all metabolites measured were found to be reduced at the site of the lesion, with NAA exhibiting the most profound loss. Prefrontal NAA reductions were found to persist at eight weeks. These findings are consistent with previous reports of local NAA reductions following tissue damage: Strauss et al. (1997) described dose-dependent reductions of striatal NAA following local infusion of 30-400 nmol quinolinic acid, whereas Guimaraes et al. (1995) reported analogous reductions in in vivo striatal NAA, in vitro NAA from striatal homogenates, and striatal GAD activity following 2 μg kainic acid lesions of the striatum. Furthermore, our finding that NAA reductions correlate with lesion extent is in agreement with the comparison described by Guimaraes et al. (1995) between in vivo NAA levels (71% of unoperated hemisphere) and gross morphology (79.9% of unoperated hemisphere volume). Our prefrontal findings are not surprising given the gross neuronal loss and cavitation that accompanied the lesion. The loss of signals throughout the proton spectra likely reflects both the loss of these chemicals and some partial volume effects. Although a non-significant 10% variation was found in the absolute water signal between groups, the water signal was higher for sham rats, which, if anything, would tend to reduce the magnitude of the NAA/unsuppressed water difference between groups.
While transsynaptic reductions in NAA have been reported in tissue homogenates ex vivo in the visual pathway following optic nerve lesions (Rango et al. 1995), we know of no previous, direct evidence suggesting that NAA is capable of providing in vivo measures of downstream effects. We report here that striatal NAA is selectively reduced two weeks following prefrontal lesions; similar reductions were found when the same animals were scanned again eight weeks after surgery. Care was taken to ensure that the prefrontal and striatal voxels did not overlap; the fact that, unlike in the prefrontal cortex, striatal metabolites other than NAA were unaffected by the lesion suggests that the striatal findings are not an artifact of imprecise localization. Moreover, since histologic examination of striatal sections from lesioned animals indicated no evidence of neurotoxic damage, it is unlikely that striatal NAA losses could reflect a direct extension of the primary lesion. No differences between groups were found in the parietal cortex, which receives minimal prefrontal innervation in comparison to the striatum (Sesack et al. 1989). Although corroboration of in vivo metabolite findings with absolute quantitative measures (as obtained with HPLC) could strengthen the results in this study, previous work has established a good concordance between in vivo and in vitro NAA (Guimaraes et al. 1995).
Our striatal findings raised additional questions about the source of these downstream NAA losses. To address the possibility that striatal NAA losses reflected lesion-induced tissue shrinkage, striatal size was compared in tissue from lesioned and sham animals; no difference was found between groups. Although we cannot rule out the possibility that striatal NAA losses reflect presynaptic changes, our finding of reduced GAD-67 mRNA expression in the anterior striatum indicates functional changes in postsynaptic GABAergic neurons, which comprise 95% of the neuronal population within the striatum (Gerfen and Wilson 1996). Given the normal histologic appearance of the striatum, the possibility of direct, lesion-induced neurotoxic effects on striatal GAD-67 mRNA seems unlikely. A previous report (Baca et al. 1998) indicated no alteration in striatal GAD-65 mRNA expression following similar (although smaller) lesions; although both GAD-65 and GAD-67 are expressed in many, if not all striatal neurons, the isoforms are differentially regulated by dopamine receptor subtypes (Laprade and Soghomonian 1995) and by GABA levels (Sheikh and Martin 1998). To the extent that striatal reductions in GAD-67 mRNA may be considered an index of neuronal dysfunction (Guimaraes et al. 1995), the colocalization of the spectroscopic and histochemical effects suggests that the NAA changes reflect transsynaptic pathology. Further work is required to determine by what mechanism striatal NAA losses and GAD-67 mRNA reductions might be linked; reductions in neuron count (the more unlikely), diminution of neuropil (also unlikely given the lack of volume change), or alterations in postsynaptic cellular machinery (e.g., mitochondria) all represent potential bridging phenomena.
Congruent with a prior report from our laboratory (Jaskiw et al. 1990), we observed that lesioned rats exhibited a greater degree of hyperlocomotion in response to amphetamine than sham rats two weeks following surgery; however, also similar to the results reported by Jaskiw et al. (1990) at 28 days postoperatively, we saw no difference between groups when animals were retested at eight weeks. The persistence of NAA alterations in both the mPFC and striatum at eight weeks despite the normalization of amphetamine-induced locomotion suggests that compensation occurs at another level and may be independent of the gross integrity of the prefrontal-striatal circuit.
Given the importance of the prefrontal-nigral-VTA circuit in the regulation of dopamine release (Murase et al. 1993; Taber and Fibiger 1995; Taber et al. 1995; Karreman and Moghaddam 1996), the subtantia nigra and VTA represent logical targets for future studies examining this compensatory response. Prefrontal lesions result in reduced D1 receptor expression (Dewar et al. 1997) and altered spontaneous activity of dopamine neurons in the VTA (Shim et al. 1996) 10 to 14 days after surgery, but long term effects have not been assessed. The resolution of 1H-MRS at 4.7 T precludes the possibility of examining smaller structures such as the VTA in vivo; however, future application of magnets with higher field strengths might prove useful in further delineating the relationship between alterations in neuronal integrity and prefrontal-subcortical dopamine regulation. In conclusion, our data indicate that NAA measures acquired in vivo with 1H-MRS may reflect local and downstream changes in neuronal integrity.
References
Andreasen NC, Flashman L, Flaum M, Arndt S, Swayze VN, O'Leary DS, Ehrhardt JC, Yuh WT . (1994): Regional brain abnormalities in schizophrenia measured with magnetic resonance imaging. JAMA 272: 1763–1769
Baca SM, Lipska BK, Egan MF, Bachus SE, Ferguson JN, Hyde TM . (1998): Effects of prefrontal cortical lesions on neuropeptide and dopamine receptor gene expression in the striatum-accumbens complex. Brain Res 797: 55–64
Bertolino A, Callicott JH, Nawroz S, Mattay VS, Duyn JH, Tedeschi G, Frank JA, Weinberger DR . (1998): Reproducibility of proton magnetic resonance spectroscopic imaging in patients with schizophrenia. Neuropsychopharmacology 18: 1–9
Bertolino A, Knable MB, Saunders RC, Callicott JH, Kolachana B, Mattay VS, Bachevalier J, Frank JA, Egan MF, Weinberger DR . (1999): The relationship between dorsolateral prefrontal N-acetylaspartate measures and striatal dopamine activity in schizophrenia. Biol Psychiatry 45: 660–667
Bertolino A, Nawroz S, Mattay VS, Barnett AS, Duyn JH, Moonen CTW, Frank JA, Tedeschi G, Weinberger DR . (1996): Regionally specific pattern of neurochemical pathology in schizophrenia as assessed by multislice proton magnetic resonance spectroscopic imaging. Am J Psychiatry 153: 1554–1563
Callicott JH, Ramsey NF, Tallent K, Bertolino A, Knable MB, Coppola R, Goldberg T, van Gelderen P, Mattay VS, Frank JA, Moonen CT, Weinberger DR . (1998): Functional magnetic resonance brain mapping in psychiatry: Methodological issues illustrated in a study of working memory in schizophrenia. Neuropsychopharmacology 18: 186–196
Carter CS, Perlstein W, Ganguli R, Brar J, Mintun M, Cohen JD . (1998): Functional hypofrontality and working memory dysfunction in schizophrenia. Am J Psychiatry 155: 1285–1287
Cooper JR, Bloom FE, Roth RH . (1991): The Biochemical Basis of Neuropharmacology, 6th ed. New York, Oxford University Press
Davis KL, Kahn RS, Ko G, Davidson M . (1991): Dopamine in schizophrenia: A review and reconceptualization. Am J Psychiatry 148: 1474–1486
Dewar KM, Rompré P-P, Stewart J, Warren RA . (1997): Excitotoxic lesions of the prefrontal cortex reduce dopamine D1-like receptors in the ventral tegmental area. Eur J Pharmacol 336: 155–158
Fletcher PC, McKenna PJ, Frith CD, Crasby PM, Friston KJ, Dolan RJ . (1998): Brain activations in schizophrenia during a graded memory task studied with functional neuroimaging. Arch Gen Psychiatry 55: 1001–1008
Gerfen CR, Wilson CJ . (1996): The basal ganglia. In Swanson LW, Björklund A, Hökfelt T (eds), Handbook of Chemical Neuroanatomy. Vol 12. Integrated Systems of the CNS, Part III. New York, Elsevier, pp 371–468
Goldberg TE, Gold JM . (1995): Neurocognitive deficits in schizophrenia. In Hirsch SR, Weinberger DR (eds), Schizophrenia. Oxford, Blackwell Science Ltd, pp 146–162
Gorelova N, Yang CR . (1997): The course of neural projection from the prefrontal cortex to the nucleus accumbens in the rat. Neuroscience 76: 689–706
Grace AA . (1991): Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: A hypothesis for the etiology of schizophrenia. Neuroscience 41: 1–24
Guimaraes AR, Schwartz P, Prakash MR, Carr CA, Berger UV, Jenkins BG, Coyle JT, González RG . (1995): Quantitative in vivo 1H nuclear magnetic resonance spectroscopic imaging of neuronal loss in rat brain. Neuroscience 69: 1095–1101
Jaskiw GE, Karoum F, Freed WJ, Phillips I, Kleinman JE, Weinberger DR . (1990): Effect of ibotenic acid lesions of the medial prefrontal cortex on amphetamine-induced locomotion and regional brain catecholamine concentrations in the rat. Brain Res 534: 263–272
Karreman M, Moghaddam B . (1996): The prefrontal cortex regulates the basal release of dopamine in the limbic striatum: An effect mediated by ventral tegmental area. J Neurochem 66: 589–598
Laprade N, Soghomonian JJ . (1995): Differential regulation of mRNA levels encoding for the two isoforms of glutamate decarboxylase (GAD65 and GAD67) by dopamine receptors in the rat striatum. Mol Brain Res 34: 65–74
Lieberman J, Kane J, Alvir J . (1987): Provocative tests with psychostimulant drugs in schizophrenia. Psychopharmacology 91: 415–433
Manoach DS, Press DZ, Thangaraj V, Searl MM, Goff DC, Halpern E, Saper CB, Warach S . (1999): Schizophrenic subjects activate dorsolateral prefrontal cortex during a working memory task, as measured by fMRI. Biol Psychiatry 45: 1128–1137
Murase S, Grenhoff J, Chouvet G, Gonon FG, Svensson TH . (1993): Prefrontal cortex regulates burst firing and transmitter release in rat mesolimbic dopamine neurons studied in vivo. Neurosci Lett 157: 53–56
Nasrallah HA, Skinner TE, Schmalbrock P, Robitaille PM . (1994): Proton magnetic resonance spectroscopy of the hippocampal formation in schizophrenia: A pilot study. Br J Psychiatry 165: 481–485
Pakkenberg B . (1987): Post-mortem study of chronic schizophrenic brains. Br J Psychiatry 151: 744–752
Paxinos G, Watson C . (1986): The Rat Brain in Stereotaxic Coordinates, Compact 3rd ed. Sydney, Orlando, Academic Press
Peroutka SJ, Snyder SH . (1980): Relationship between neuroleptic effects at brain dopamine, serotonin, alpha-adrenergic, and histamine receptors to clinical potency. Am J Psychiatry 137: 1518–1522
Rango M, Spagnoli D, Tomei G, Balmonti F, Scarlato G, Zetta L . (1995): Central nervous system trans-synaptic effects of acute axonal injury: A 1H magnetic resonance spectroscopy study. Magn Reson Med 33: 595–600
Saunders RC, Kolachana BS, Bachevalier J, Weinberger DR . (1998): Neonatal lesions of the medial temporal lobe disrupt prefrontal cortical regulation of striatal dopamine. Nature 393: 169–171
Selemon LD, Rajkowska G, Goldman-Rakic PS . (1995): Abnormally high neuronal density in the schizophrenic cortex. A morphometric analysis of prefrontal area 9 and occipital area 17. Arch Gen Psychiatry 52: 805–818
Sesack SR, Deutch AY, Roth RH, Bunney BS . (1989): Topographical organization of the efferent projections of the medial prefrontal cortex in the rat: An anterograde tract-tracing study with Phaseolus vulgaris leucoagglutinin. J Comp Neurol 290: 213–242
Sesack SR, Pickel VM . (1992): Prefrontal cortical efferents in the rat synapse on unlabeled neuronal targets of catecholamine terminals in the nucleus accumbens septi and on dopamine neurons in the ventral tegmental area. J Comp Neurol 320: 145–160
Sheikh SN, Martin DL . (1998): Elevation of brain GABA levels with vigabatrin (gamma-vinylGABA) differentially affects GAD65 and GAD67 expression in various regions of rat brain. J Neurosci Res 52: 736–741
Shim SS, Bunney BS, Shi W-X . (1996): Effects of lesions in the medial prefrontal cortex on the activity of midbrain dopamine neurons. Neuropsychopharmacology 15: 437–441
Strauss I, Williamson JM, Bertram EH, Lothman EW, Fernandez EJ . (1997): Histological and 1H magnetic resonance spectroscopic imaging analysis of quinolinic acid-induced damage to the rat striatum. Magn Reson Med 37: 24–33
Taber MT, Das S, Fibiger HC . (1995): Cortical regulation of subcortical dopamine release: Mediation via the ventral tegmental area. J Neurochem 65: 1407–1410
Taber MT, Fibiger HC . (1995): Electrical stimulation of the prefrontal cortex increases dopamine release in the nucleus accumbens of the rat: Modulation by metabotropic glutamate receptors. J Neurosci 5: 3896–3904
Takagishi M, Chiba T . (1991): Efferent projections of the infralimbic (area 25) region of the medial prefrontal cortex in the rat: An anterograde tracer PHA-L study. Brain Res 566: 26–39
Tsai G, Coyle JT . (1995): N-acetylaspartate in neuropsychiatric disorders. Prog Neurobiol 46: 531–540
Tsai G, Passani LA, Slusher BS, Carter R, Kleinman JE, Coyle JT . (1995): Changes of excitatory neurotransmitter metabolism in schizophrenic brains. Arch Gen Psychiatry 52: 829–836
Urenjak J, Williams SR, Gadian DG, Noble M . (1993): Proton nuclear magnetic resonance spectroscopy unambiguously identifies different neural cell types. J Neurosci 13: 981–989
Weinberger DR . (1987): Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry 44: 660–669
Weinberger DR, Berman KF, Zec RF . (1986): Physiological dysfunction of dorsolateral prefrontal cortex in schizophrenia. I. Regional cerebral blood flow evidence. Arch Gen Psychiatry 43: 114–125
Yurgelun-Todd DA, Renshaw PF, Gruber SA, Waternaux CM, Cohen BM . (1996): Proton magnetic resonance spectroscopy of the temporal lobes in schizophrenics and normal controls. Schizophr Res 19: 55–59
Acknowledgements
We are grateful to Daryl DesPres, Rebecca Rakow, Karin Weidenhammer, and Michael Valentine for their essential contributions to this work. Supported in part by the H.H.M.I.-N.I.H. Research Scholars Program.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Roffman, J., Lipska, B., Bertolino, A. et al. Local and Downstream Effects of Excitotoxic Lesions in the Rat Medial Prefrontal Cortex on In Vivo 1H-MRS Signals. Neuropsychopharmacol 22, 430–439 (2000). https://doi.org/10.1016/S0893-133X(99)00143-8
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00143-8
Keywords
This article is cited by
-
Asenapine restores cognitive flexibility in rats with medial prefrontal cortex lesions
Psychopharmacology (2009)