Abstract
Cancer cells metastasize through the bloodstream either as single migratory circulating tumor cells (CTCs) or as multicellular groupings (CTC clusters). Existing technologies for CTC enrichment are designed to isolate single CTCs, and although CTC clusters are detectable in some cases, their true prevalence and significance remain to be determined. Here we developed a microchip technology (the Cluster-Chip) to capture CTC clusters independently of tumor-specific markers from unprocessed blood. CTC clusters are isolated through specialized bifurcating traps under low–shear stress conditions that preserve their integrity, and even two-cell clusters are captured efficiently. Using the Cluster-Chip, we identified CTC clusters in 30–40% of patients with metastatic breast or prostate cancer or with melanoma. RNA sequencing of CTC clusters confirmed their tumor origin and identified tissue-derived macrophages within the clusters. Efficient capture of CTC clusters will enable the detailed characterization of their biological properties and role in metastasis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Accession codes
References
Pantel, K., Brakenhoff, R.H. & Brandt, B. Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat. Rev. Cancer 8, 329–340 (2008).
Yu, M., Stott, S., Toner, M., Maheswaran, S. & Haber, D.A. Circulating tumor cells: approaches to isolation and characterization. J. Cell Biol. 192, 373–382 (2011).
Nagrath, S. et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology. Nature 450, 1235–1239 (2007).
Stott, S.L. et al. Isolation of circulating tumor cells using a microvortex-generating herringbone-chip. Proc. Natl. Acad. Sci. USA 107, 18392–18397 (2010).
Ozkumur, E. et al. Inertial focusing for tumor antigen-dependent and -independent sorting of rare circulating tumor cells. Sci. Transl. Med. 5, 179ra47 (2013).
Yoon, H.J. et al. Sensitive capture of circulating tumour cells by functionalized graphene oxide nanosheets. Nat. Nanotechnol. 8, 735–741 (2013).
Yu, M. et al. Circulating breast tumor cells exhibit dynamic changes in epithelial and mesenchymal composition. Science 339, 580–584 (2013).
Watanabe, S. The metastasizability of tumor cells. Cancer 7, 215–223 (1954).
Fidler, I.J. The relationship of embolic homogeneity, number, size and viability to the incidence of experimental metastasis. Eur. J. Cancer 9, 223–227 (1973).
Yu, M. et al. RNA sequencing of pancreatic circulating tumour cells implicates WNT signalling in metastasis. Nature 487, 510–513 (2012).
Brandt, B. et al. Isolation of prostate-derived single cells and cell clusters from human peripheral blood. Cancer Res. 56, 4556–4561 (1996).
Molnar, B., Ladanyi, A., Tanko, L., Sréter, L. & Tulassay, Z. Circulating tumor cell clusters in the peripheral blood of colorectal cancer patients. Clin. Cancer Res. 7, 4080–4085 (2001).
Cho, E.H. et al. Characterization of circulating tumor cell aggregates identified in patients with epithelial tumors. Phys. Biol. 9, 016001 (2012).
Krebs, M.G. et al. Analysis of circulating tumor cells in patients with non-small cell lung cancer using epithelial marker-dependent and-independent approaches. J. Thorac. Oncol. 7, 306–315 (2012).
Hou, H.W. et al. Isolation and retrieval of circulating tumor cells using centrifugal forces. Sci. Rep. 3, 1259 (2013).
Duda, D.G. et al. Malignant cells facilitate lung metastasis by bringing their own soil. Proc. Natl. Acad. Sci. USA 107, 21677–21682 (2010).
Hou, J.M. et al. Clinical significance and molecular characteristics of circulating tumor cells and circulating tumor microemboli in patients with small-cell lung cancer. J. Clin. Oncol. 30, 525–532 (2012).
Aceto, N. et al. Circulating tumor cell clusters are oligoclonal precursors of breast cancer metastasis. Cell 158, 1110–1122 (2014).
Vona, G. et al. Isolation by size of epithelial tumor cells: a new method for the immunomorphological and molecular characterization of circulating tumor cells. Am. J. Pathol. 156, 57–63 (2000).
Coumans, F.A.W., van Dalum, G., Beck, M. & Terstappen, L.W.M.M. Filtration parameters influencing circulating tumor cell enrichment from whole blood. PLoS ONE 8, e61774 (2013).
Yu, M. et al. A developmentally regulated inducer of EMT, LBX1, contributes to breast cancer progression. Genes Dev. 23, 1737–1742 (2009).
Rico, F., Chu, C., Abdulreda, M.H., Qin, Y. & Moy, V.T. Temperature modulation of integrin-mediated cell adhesion. Biophys. J. 99, 1387–1396 (2010).
Kattlove, H.E. & Alexander, B. The effect of cold on platelets. I. Cold-induced platelet aggregation. Blood 38, 39–48 (1971).
Shah, A.M. et al. Biopolymer system for cell recovery from microfluidic cell capture devices. Anal. Chem. 84, 3682–3688 (2012).
Luo, X. et al. Isolation and molecular characterization of circulating melanoma cells. Cell Rep. 7, 645–653 (2014).
Miyamoto, D.T. et al. Androgen receptor signaling in circulating tumor cells as a marker of hormonally responsive prostate cancer. Cancer Discov. 2, 995–1003 (2012).
Inwald, E.C. et al. Ki-67 is a prognostic parameter in breast cancer patients: results of a large population-based cohort of a cancer registry. Breast Cancer Res. Treat. 139, 539–552 (2013).
Labelle, M., Begum, S. & Hynes, R.O. Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell 20, 576–590 (2011).
Kuvaja, P. et al. Tumor tissue inhibitor of metalloproteinases-1 (TIMP-1) in hormone-independent breast cancer might originate in stromal cells, and improves stratification of prognosis together with nodal status. Exp. Cell Res. 318, 1094–1103 (2012).
Hekmat, O. et al. TIMP-1 increases expression and phosphorylation of proteins associated with drug resistance in breast cancer cells. J. Proteome Res. 12, 4136–4151 (2013).
Würtz, S.O., Schrohl, A.-S., Mouridsen, H. & Brünner, N. TIMP-1 as a tumor marker in breast cancer–an update. Acta Oncol. 47, 580–590 (2008).
Würtz, S.Ø. et al. Tissue inhibitor of metalloproteinases-1 in breast cancer. Endocr. Relat. Cancer 12, 215–227 (2005).
Talasaz, A.H. et al. Isolating highly enriched populations of circulating epithelial cells and other rare cells from blood using a magnetic sweeper device. Proc. Natl. Acad. Sci. USA 106, 3970–3975 (2009).
Qian, B.-Z. & Pollard, J.W. Macrophage diversity enhances tumor progression and metastasis. Cell 141, 39–51 (2010).
Wyckoff, J.B. et al. Direct visualization of macrophage-assisted tumor cell intravasation in mammary tumors. Cancer Res. 67, 2649–2656 (2007).
Pardoll, D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 12, 252–264 (2012).
Kojic´, N. et al. A 3-D model of ligand transport in a deforming extracellular space. Biophys. J. 99, 3517–3525 (2010).
Acknowledgements
We express our gratitude to all patients and healthy volunteers who participated in this study and contributed blood samples. We thank O. Hurtado, A.J. Aranyosi and L. Libby for coordination of the research laboratories; D.M. Lewis for his help in instrumentation; and L. Nieman, J. Walsh and T.N. Lewis for their help with microscopy. N.A. was supported by the Swiss National Science Foundation and the Human Frontiers Science Program. This work was supported by the US National Institutes of Health (NIH) P41 Resource Center (M.T.); an NIH National Institute of Biomedical Imaging and Bioengineering Quantum Grant (M.T. and D.A.H.); Stand Up to Cancer (D.A.H., M.T. and S.M.); the Howard Hughes Medical Institute (D.A.H.); the Prostate Cancer Foundation and the Charles Evans Foundation (D.A.H. and M.T.); and Johnson and Johnson (M.T. and S.M.).
Author information
Authors and Affiliations
Contributions
A.F.S., N.A., S.M., D.A.H. and M.T. designed the research, analyzed the data and prepared the manuscript. N.K. performed computer simulations. M.C.D., M.Z. and A.E. processed clinical samples, performed immunofluorescence staining and scanning. B.H. manufactured devices for clinical studies. H.Z. and T.S. performed amplification and RNA sequencing. T.K.S., D.T.M., X.L. and A.B. provided clinical samples. B.S.W. performed statistical analysis on the RNA sequencing data. S.R., D.T.T., S.L.S. and R.K. commented on the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.F.S. and M.T. are inventors on a patent Massachusetts General Hospital filed to protect the Cluster-Chip technology.
Integrated supplementary information
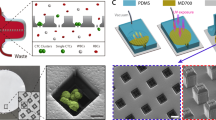
Supplementary Figure 1 Finite-element analysis of cell cluster dynamics in different cluster trap architectures.
(a) Cluster-Chip (b) Filter (c) A structure identical to the Cluster-Chip except that one of the openings is closed d) A filter formed by two triangular pillars. In all cases except the Cluster-Chip, cluster larger than the opening size passes due to its elastic behavior. The cluster being missed points to the importance of split flow fields simultaneously effecting the cluster in the Cluster-Chip and proves that the capture in the Cluster-Chip is not simply due to filtering. In all simulations, the opening widths and diameters of individual cells are 14 μm.
Supplementary Figure 2 Probability of chip-mediated artifact cluster formation from single cells on the Cluster-Chip.
The calculated probabilities are based on simplifying assumptions on chip geometry and cell adhesion. We assume a blood sample with 1000 CTCs. In addition, each of the 4096 parallel cluster traps on the Cluster-Chip is assumed to have equal probability of receiving CTCs and whenever multiple CTCs go into the same trap, a CTC-cluster is formed. We used Poisson approximation to calculate probability of forming a CTC-cluster composed of a specific number of cells. Our model confirms that it is extremely unlikely to form artifact CTC clusters on the Cluster-Chip.
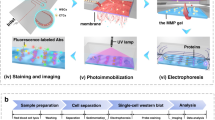
Supplementary Figure 3 Experimental setup used to quantify the capture efficiency of the Cluster-Chip.
A smaller version of the Cluster-Chip is connected to a large microfluidic waste chamber, which permits to accurately identify and analyze non-captured cell clusters in whole blood. Both the chip and waste chamber are imaged using fluorescence microscopy to calculate the cell cluster capture efficiency.
Supplementary Figure 4 Distribution of captured small and large clusters on the Cluster-Chip.
Normalized distribution of (a) 2-cell clusters (b) 3-cell clusters (c) clusters containing 4 or more cells across the Cluster-Chip. We used simulated whole blood samples spiked with artificial clusters of MDA-MB-231 breast cancer cell line. The Cluster-Chip was operated at 2.5 ml/hr and was on a thermoelectric cooler set at 4°C.
Supplementary Figure 5 Characterization of MDA-MB-231 cell cluster size distribution before spiking.
We prepare clusters of fluorescently labeled MDA-MB-231 cancer cells and deposit the suspension on an ultra-low attachment culture dish. Using fluorescence microscopy, we count the number of cells within each cluster and then spike into whole blood in order to prepare a simulated sample containing characterized cluster population for quantitative device testing.
Supplementary Figure 6 Intact and damaged cell clusters captured using a membrane filter.
Fluorescent and brightftield images of intact and damaged MDA-MB-231 cell clusters when captured using a polycarbonate track-etched membrane filter operated under 1.5 psi.
Supplementary Figure 7 Viability of cell clusters released from the Cluster-Chip.
The Cluster-Chip is operated at 4°C and the clusters were released at 250 ml/hr reverse flow rate (A) Fluorescent images of MDA-MB-231 clusters treated with two-color viability (green)/cytotoxicity (red) assay. The cells are divided in two batches: Control and cell clusters captured and released from Cluster-Chip (B) Percentage of viable clusters captured and released using Cluster-Chip against the control. Scale bar 100 μm.
Supplementary Figure 8 Images of CTC -clusters isolated from a breast cancer patient and released in solution.
CTC-clusters isolated from a patient with metastatic breast cancer using the Cluster-Chip operated at 4°C and released with reverse flow. CTC clusters are not fixed and live stained for common breast cancer surface markers. Scale bar 20 μm.
Supplementary Figure 9 Correlation between the number of CTCs and CTC clusters in patients.
Comparison of number of CTC clusters isolated using the Cluster-Chip and number of single CTCs isolated using CTC-iChip from the same patient at the same timepoint. Among the 19 cases studied, we found no correlation between the numbers of CTC-clusters and that of single CTCs.
Supplementary Figure 10 Proliferative index of single CTCs isolated from a breast cancer patient.
Representative images of a Ki67-negative (-) and a Ki67-positive (+) CTC stained with antibodies against wide spectrum cytokeratin (CK, red), Ki67 (yellow) and CD45 (green). Nuclei are stained with DAPI (blue). The bar graph shows the mean percentage of Ki67-positive cells isolated from a breast cancer patient across multiple time points. All together, 439 single CTCs were stained and 162 resulted positive for Ki67.
Supplementary Figure 11 Heat map showing expression levels of CTC clusters isolated from a patient.
Heatmap showing expression levels of representative epithelial-to-mesenchymal transition (EMT) genes in released CTC-clusters and healthy donor white blood cells (WBCs). Epithelial markers E-cadherin (CDH1), EpCAM and Mucin1 (MUC1), as well as mesenchymal markers Vimentin (VIM), Fibronectin1 (FN1), N-cadherin (CDH2) and TWIST1 are shown.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–11 and Supplementary Table 1 (PDF 778 kb)
Real-time capture of cell clusters in whole blood on the Cluster-Chip
Real-time video of the Cluster-Chip processing a simulated sample at 2.5 ml/hr. The sample is prepared by spiking artificially formed clusters of fluorescently labeled MDA-MB-231 cancer cells into whole blood samples collected from a healthy donor. Unlabeled blood cells flowing through the chip are not visible in the fluorescent channel but can be noticed as they obscure the fluorescence emission from captured clusters. (MP4 7507 kb)
Source data
Rights and permissions
About this article
Cite this article
Sarioglu, A., Aceto, N., Kojic, N. et al. A microfluidic device for label-free, physical capture of circulating tumor cell clusters. Nat Methods 12, 685–691 (2015). https://doi.org/10.1038/nmeth.3404
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nmeth.3404
This article is cited by
-
Proof-of-principle study using Saccharomyces cerevisiae for universal screening test for cancer through ultrasound-based size distinction of circulating tumor cell clusters
Journal of Biosciences (2024)
-
Modular microfluidics for life sciences
Journal of Nanobiotechnology (2023)
-
Ex vivo expansion of circulating tumour cells (CTCs)
Scientific Reports (2023)
-
The journey from melanocytes to melanoma
Nature Reviews Cancer (2023)
-
The epithelial–mesenchymal plasticity landscape: principles of design and mechanisms of regulation
Nature Reviews Genetics (2023)