Abstract
Leptin treatment reverses hyperglycemia in animal models of poorly controlled type 1 diabetes (T1D)1,2,3,4,5,6, spurring great interest in the possibility of treating patients with this hormone. The antidiabetic effect of leptin has been postulated to occur through suppression of glucagon production, suppression of glucagon responsiveness or both; however, there does not appear to be a direct effect of leptin on the pancreatic alpha cell7. Thus, the mechanisms responsible for the antidiabetic effect of leptin remain poorly understood. We quantified liver-specific rates of hepatic gluconeogenesis and substrate oxidation in conjunction with rates of whole-body acetate, glycerol and fatty acid turnover in three rat models of poorly controlled diabetes, including a model of diabetic ketoacidosis8. We show that the higher rates of hepatic gluconeogenesis in all these models could be attributed to hypoleptinemia-induced activity of the hypothalamic-pituitary-adrenal (HPA) axis, resulting in higher rates of adipocyte lipolysis, hepatic conversion of glycerol to glucose through a substrate push mechanism and conversion of pyruvate to glucose through greater hepatic acetyl-CoA allosteric activation of pyruvate carboxylase flux. Notably, these effects could be dissociated from changes in plasma insulin and glucagon concentrations and hepatic gluconeogenic protein expression. All the altered systemic and hepatic metabolic fluxes could be mimicked by infusing rats with Intralipid or corticosterone and were corrected by leptin replacement. These data demonstrate a critical role for lipolysis and substrate delivery to the liver, secondary to hypoleptinemia and HPA axis activity, in promoting higher hepatic gluconeogenesis and hyperglycemia in poorly controlled diabetes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Fujikawa, T. et al. Leptin engages a hypothalamic neurocircuitry to permit survival in the absence of insulin. Cell Metab. 18, 431–444 (2013).
Meek, T.H. et al. Leptin action in the ventromedial hypothalamic nucleus is sufficient, but not necessary, to normalize diabetic hyperglycemia. Endocrinology 154, 3067–3076 (2013).
Fujikawa, T., Chuang, J.C., Sakata, I., Ramadori, G. & Coppari, R. Leptin therapy improves insulin-deficient type 1 diabetes by CNS-dependent mechanisms in mice. Proc. Natl. Acad. Sci. USA 107, 17391–17396 (2010).
Wang, M.Y. et al. Leptin therapy in insulin-deficient type I diabetes. Proc. Natl. Acad. Sci. USA 107, 4813–4819 (2010).
Chinookoswong, N., Wang, J.L. & Shi, Z.Q. Leptin restores euglycemia and normalizes glucose turnover in insulin-deficient diabetes in the rat. Diabetes 48, 1487–1492 (1999).
Lin, C.Y., Higginbotham, D.A., Judd, R.L. & White, B.D. Central leptin increases insulin sensitivity in streptozotocin-induced diabetic rats. Am. J. Physiol. Endocrinol. Metab. 282, E1084–E1091 (2002).
Chen, L., Philippe, J. & Unger, R.H. Glucagon responses of isolated alpha cells to glucose, insulin, somatostatin, and leptin. Endocr. Prac. 17, 819–825 (2011).
Craighead, J.E. Experimental models of juvenile onset (insulin-dependent) diabetes mellitus. Monogr. Pathol. 21, 166–176 (1980).
Utter, M.F. & Keech, D.B. Formation of oxaloacetate from pyruvate and carbon dioxide. J. Biol. Chem. 235, PC17–PC18 (1960).
Scrutton, M.C. & White, M.D. Pyruvate carboxylase from rat liver: catalytic properties in the absence, and at low concentrations, of acetyl-CoA. Biochem. Biophys. Res. Commun. 48, 85–93 (1972).
McClure, W.R., Lardy, H.A. & Kneifel, H.P. Rat liver pyruvate carboxylase. I. Preparation, properties, and cation specificity. J. Biol. Chem. 246, 3569–3578 (1971).
Warren, G.B. & Tipton, K.F. Pig liver pyruvate carboxylase. The reaction pathway for the carboxylation of pyruvate. Biochem. J. 139, 311–320 (1974).
Sugden, M.C. & Holness, M.J. Recent advances in mechanisms regulating glucose oxidation at the level of the pyruvate dehydrogenase complex by PDKs. Am. J. Physiol. Endocrinol. Metab. 284, E855–E862 (2003).
Kitabchi, A.E. & Wall, B.M. Diabetic ketoacidosis. Med. Clin. North Am. 79, 9–37 (1995).
Minokoshi, Y., Toda, C. & Okamoto, S. Regulatory role of leptin in glucose and lipid metabolism in skeletal muscle. Indian J. Endocrinol. Metab. 16, S562–S568 (2012).
Toda, C. et al. Extracellular signal-regulated kinase in the ventromedial hypothalamus mediates leptin-induced glucose uptake in red-type skeletal muscle. Diabetes 62, 2295–2307 (2013).
Laker, R.C. et al. Central infusion of leptin does not increase AMPK signaling in skeletal muscle of sheep. Am. J. Physiol. Regul. Integr. Comp. Physiol. 300, R511–R518 (2011).
Previs, S.F., Cline, G.W. & Shulman, G.I. A critical evaluation of mass isotopomer distribution analysis of gluconeogenesis in vivo. Am. J. Physiol. 277, E154–E160 (1999).
Boden, G., Chen, X., Rosner, J. & Barton, M. Effects of a 48-h fat infusion on insulin secretion and glucose utilization. Diabetes 44, 1239–1242 (1995).
Dubuc, P.U. Basal corticosterone levels of young og/ob mice. Horm. Metab. Res. 9, 95–97 (1977).
Coleman, D.L. & Burkart, D.L. Plasma corticosterone concentrations in diabetic (db) mice. Diabetologia 13, 25–26 (1977).
Szücs, N. et al. Leptin inhibits cortisol and corticosterone secretion in pathologic human adrenocortical cells. Pituitary 4, 71–77 (2001).
Loose, D.S., Stover, E.P. & Feldman, D. Ketoconazole binds to glucocorticoid receptors and exhibits glucocorticoid antagonist activity in cultured cells. J. Clin. Invest. 72, 404–408 (1983).
da Silva, A.A., Tallam, L.S., Liu, J. & Hall, J.E. Chronic antidiabetic and cardiovascular actions of leptin: role of CNS and increased adrenergic activity. Am. J. Physiol. Regul. Integr. Comp. Physiol. 291, R1275–R1282 (2006).
Wang, J., Wernette, C.M., Judd, R.L., Huggins, K.W. & White, B.D. Guanethidine treatment does not block the ability of central leptin administration to decrease blood glucose concentrations in streptozotocin-induced diabetic rats. J. Endocrinol. 198, 541–548 (2008).
Hathout, E.H. et al. Changes in plasma leptin during the treatment of diabetic ketoacidosis. J. Clin. Endocrinol. Metab. 84, 4545–4548 (1999).
Kratzsch, J. et al. Metabolic decompensation in children with type 1 diabetes mellitus associated with increased serum levels of the soluble leptin receptor. Eur. J. Endocrinol. 155, 609–614 (2006).
Kitabchi, A.E. & Umpierrez, G.E. Changes in serum leptin in lean and obese subjects with acute hyperglycemic crises. J. Clin. Endocrinol. Metab. 88, 2593–2596 (2003).
Petersen, K.F. et al. Leptin reverses insulin resistance and hepatic steatosis in patients with severe lipodystrophy. J. Clin. Invest. 109, 1345–1350 (2002).
Perry, R.J. et al. Reversal of hypertriglyceridemia, fatty liver disease, and insulin resistance by a liver-targeted mitochondrial uncoupler. Cell Metab. 18, 740–748 (2013).
Erion, D.M. et al. The role of the carbohydrate response element-binding protein in male fructose-fed rats. Endocrinology 154, 36–44 (2013).
Alves, T.C. et al. Regulation of hepatic fat and glucose oxidation in rats with lipid-induced hepatic insulin resistance. Hepatology 53, 1175–1181 (2011).
Jurczak, M.J. et al. Dissociation of inositol-requiring enzyme (IRE1α)-mediated c-Jun N-terminal kinase activation from hepatic insulin resistance in conditional X-box-binding protein-1 (XBP1) knock-out mice. J. Biol. Chem. 287, 2558–2567 (2012).
Jucker, B.M., Rennings, A.J., Cline, G.W., Petersen, K.F. & Shulman, G.I. In vivo NMR investigation of intramuscular glucose metabolism in conscious rats. Am. J. Physiol. 273, E139–E148 (1997).
Hosokawa, Y., Shimomura, Y., Harris, R.A. & Ozawa, T. Determination of short-chain acyl-coenzyme A esters by high-performance liquid chromatography. Anal. Biochem. 153, 45–49 (1986).
Roughan, G. A semi-preparative enzymic synthesis of malonyl-CoA from [14C]acetate and 14CO2: labelling in the 1, 2 or 3 position. Biochem. J. 300, 355–358 (1994).
Kumashiro, N. et al. Role of patatin-like phospholipase domain-containing 3 on lipid-induced hepatic steatosis and insulin resistance in rats. Hepatology 57, 1763–1772 (2013).
Acknowledgements
We thank V. Samuel, D. Befroy and K. Petersen for helpful discussions and J. Dong, Y. Kosover, M. Kahn, B. Perler, J. Stack and M. Batsu for expert technical support. This study was funded by grants from the US National Institutes of Health (R01 DK-40936, R24 DK-085638, U24 DK-059635 and P30 DK-45735), an American Diabetes Association–Merck Clinical/Translational Science Postdoctoral Fellowship Award from the American Diabetes Association and the Novo Nordisk Foundation for Basic Metabolic Research.
Author information
Authors and Affiliations
Contributions
R.J.P. and G.I.S. designed the experimental protocols. R.J.P., X.-M.Z., D.Z., N.K., J.-P.G.C. and G.W.C. performed the studies. All authors contributed to the analysis of data. R.J.P. and G.I.S. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–9 and Supplementary Tables 1–2 (PDF 678 kb)
Supplementary Methods
Supplementary Methods (PDF 685 kb)
Rights and permissions
About this article
Cite this article
Perry, R., Zhang, XM., Zhang, D. et al. Leptin reverses diabetes by suppression of the hypothalamic-pituitary-adrenal axis. Nat Med 20, 759–763 (2014). https://doi.org/10.1038/nm.3579
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3579
This article is cited by
-
Arcuate AgRP, but not POMC neurons, modulate paraventricular CRF synthesis and release in response to fasting
Cell & Bioscience (2022)
-
Codon-optimized FAM132b gene therapy prevents dietary obesity by blockading adrenergic response and insulin action
International Journal of Obesity (2022)
-
Hepatic non-parenchymal S100A9-TLR4-mTORC1 axis normalizes diabetic ketogenesis
Nature Communications (2022)
-
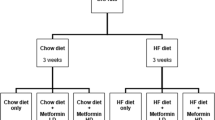
Metformin effectively restores the HPA axis function in diet-induced obese rats
International Journal of Obesity (2021)
-
A neural basis for brain leptin action on reducing type 1 diabetic hyperglycemia
Nature Communications (2021)