Abstract
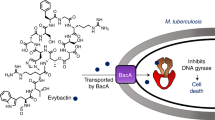
Although the classical antibiotic spectinomycin is a potent bacterial protein synthesis inhibitor, poor antimycobacterial activity limits its clinical application for treating tuberculosis. Using structure-based design, we generated a new semisynthetic series of spectinomycin analogs with selective ribosomal inhibition and excellent narrow-spectrum antitubercular activity. In multiple murine infection models, these spectinamides were well tolerated, significantly reduced lung mycobacterial burden and increased survival. In vitro studies demonstrated a lack of cross resistance with existing tuberculosis therapeutics, activity against multidrug-resistant (MDR) and extensively drug-resistant tuberculosis and an excellent pharmacological profile. Key to their potent antitubercular properties was their structural modification to evade the Rv1258c efflux pump, which is upregulated in MDR strains and is implicated in macrophage-induced drug tolerance. The antitubercular efficacy of spectinamides demonstrates that synthetic modifications to classical antibiotics can overcome the challenge of intrinsic efflux pump-mediated resistance and expands opportunities for target-based tuberculosis drug discovery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Accession codes
References
Zumla, A., Raviglione, M., Hafner, R. & von Reyn, C.F. Tuberculosis. N. Engl. J. Med. 368, 745–755 (2013).
Global Tuberculosis Report, WHO 2012. (WHO, Geneva, Switzerland, 2012).
Silver, L.L. Challenges of antibacterial discovery. Clin. Microbiol. Rev. 24, 71–109 (2011).
Newman, D.J. & Cragg, G.M. Natural products as sources of new drugs over the 30 years from 1981 to 2010. J. Nat. Prod. 75, 311–335 (2012).
Carter, A.P. et al. Functional insights from the structure of the 30S ribosomal subunit and its interactions with antibiotics. Nature 407, 340–348 (2000).
Borovinskaya, M.A., Shoji, S., Holton, J.M., Fredrick, K. & Cate, J.H. A steric block in translation caused by the antibiotic spectinomycin. ACS Chem. Biol. 2, 545–552 (2007).
Novak, E., Schlagel, C.A., LeZotte, L.A. & Pfeifer, R.T. The tolerance of high dose intravenous spectinomycin therapy in man. J. Clin. Pharmacol. 14, 442–447 (1974).
Akiyoshi, M., Yano, S. & Ikeda, T. [Ototoxicity of spectinomycin (author's transl)]. Jpn. J. Antibiot. 29, 771–782 (1976).
Thomas, R.C. & Fritzen, E.L. Spectinomycin modification. III. Spectinomycin analogs with C-3′-branched chain sugars. J. Antibiot. (Tokyo) 38, 208–219 (1985).
Woitun, E., Maier, R., Wetzel, B., Reuter, W. & Lechner, U. Modification of spectinomycin. 2. Derivatives of 4-dihydro-4-deoxy-4(R)-aminospectinomycin. J. Antibiot. (Tokyo) 34, 22–27 (1981).
Maier, R., Woitun, E., Reuter, A., Reuter, W. & Wetzel, B. Modification of spectinomycin. 1. Synthesis of 4-aminospectinomycins. J. Antibiot. (Tokyo) 34, 16–21 (1981).
Zurenko, G.E., Yagi, B.H., Vavra, J.J. & Wentworth, B.B. In vitro antibacterial activity of trospectomycin (U-63366F), a novel spectinomycin analog. Antimicrob. Agents Chemother. 32, 216–223 (1988).
Noskin, G.A. Tigecycline: a new glycylcycline for treatment of serious infections. Clin. Infect. Dis. 41 (suppl. 5), S303–S314 (2005).
Projan, S.J. Preclinical pharmacology of GAR-936, a novel glycylcycline antibacterial agent. Pharmacotherapy 20, 219S–223S (2000).
Wiley, P.F., Argoudelis, A.D. & Hoesema, H. The chemistry of actinospectacin. IV. The determination of the structure of actinospectacin. J. Am. Chem. Soc. 85, 2652–2659 (1963).
Foley, L., Lin, J.T. & Weigele, M. Spectinomycin chemistry. II.) 9-Deoxy-4(R)-dihydrospectinomycin and 9-deoxyspectinomycin. J. Antibiot. (Tokyo) 31, 979–984 (1978).
Foley, L., Lin, J.T. & Weigele, M. Preparation of 7-deoxyspectinomycin and 7-deoxy-8-epi-4(R)-dihydrospectinomycin. J. Antibiot. (Tokyo) 32, 418–419 (1979).
Rosenbrook, W. Jr. & Carney, R.E. Spectinomycin modification. I 7-EPI-9-deoxy-4(R)-dihydrospectinomycin. J. Antibiot. (Tokyo) 28, 953–959 (1975).
Balganesh, M. et al. Efflux pumps of Mycobacterium tuberculosis play a significant role in antituberculosis activity of potential drug candidates. Antimicrob. Agents Chemother. 56, 2643–2651 (2012).
Friesner, R.A. et al. Glide: a new approach for rapid, accurate docking and scoring. 1. Method and assessment of docking accuracy. J. Med. Chem. 47, 1739–1749 (2004).
Wilcken, R., Zimmermann, M.O., Lange, A., Joerger, A.C. & Boeckler, F.M. Principles and applications of halogen bonding in medicinal chemistry and chemical biology. J. Med. Chem. 56, 1363–1388 (2013).
Galimand, M., Gerbaud, G. & Courvalin, P. Spectinomycin resistance in Neisseria spp. due to mutations in 16S rRNA. Antimicrob. Agents Chemother. 44, 1365–1366 (2000).
Zaunbrecher, M.A., Sikes, R.D. Jr., Metchock, B., Shinnick, T.M. & Posey, J.E. Overexpression of the chromosomally encoded aminoglycoside acetyltransferase eis confers kanamycin resistance in Mycobacterium tuberculosis. Proc. Natl. Acad. Sci. USA 106, 20004–20009 (2009).
Honaker, R.W., Dhiman, R.K., Narayanasamy, P., Crick, D.C. & Voskuil, M.I. DosS responds to a reduced electron transport system to induce the Mycobacterium tuberculosis DosR regulon. J. Bacteriol. 192, 6447–6455 (2010).
Ramón-García, S. et al. Functional and genetic characterization of the tap efflux pump in Mycobacterium bovis BCG. Antimicrob. Agents Chemother. 56, 2074–2083 (2012).
Böttger, E.C., Springer, B., Prammananan, T., Kidan, Y. & Sander, P. Structural basis for selectivity and toxicity of ribosomal antibiotics. EMBO Rep. 2, 318–323 (2001).
Hobbie, S.N. et al. Genetic analysis of interactions with eukaryotic rRNA identify the mitoribosome as target in aminoglycoside ototoxicity. Proc. Natl. Acad. Sci. USA 105, 20888–20893 (2008).
Hobbie, S.N. et al. Mitochondrial deafness alleles confer misreading of the genetic code. Proc. Natl. Acad. Sci. USA 105, 3244–3249 (2008).
Barnhill, A.E., Brewer, M.T. & Carlson, S.A. Adverse effects of antimicrobials via predictable or idiosyncratic inhibition of host mitochondrial components. Antimicrob. Agents Chemother. 56, 4046–4051 (2012).
McKee, E.E., Ferguson, M., Bentley, A.T. & Marks, T.A. Inhibition of mammalian mitochondrial protein synthesis by oxazolidinones. Antimicrob. Agents Chemother. 50, 2042–2049 (2006).
Hobbie, S.N. et al. Engineering the rRNA decoding site of eukaryotic cytosolic ribosomes in bacteria. Nucleic Acids Res. 35, 6086–6093 (2007).
Shcherbakov, D. et al. Directed mutagenesis of Mycobacterium smegmatis 16S rRNA to reconstruct the in-vivo evolution of aminoglycoside resistance in Mycobacterium tuberculosis. Mol. Microbiol. 77, 830–840 (2010).
Drusano, G.L. Antimicrobial pharmacodynamics: critical interactions of 'bug and drug'. Nat. Rev. Microbiol. 2, 289–300 (2004).
Lenaerts, A.J., Gruppo, V., Brooks, J.V. & Orme, I.M. Rapid in vivo screening of experimental drugs for tuberculosis using γ-interferon gene–disrupted mice. Antimicrob. Agents Chemother. 47, 783–785 (2003).
Lenaerts, A.J. et al. Preclinical testing of the nitroimidazopyran PA-824 for activity against Mycobacterium tuberculosis in a series of in vitro and in vivo models. Antimicrob. Agents Chemother. 49, 2294–2301 (2005).
Bissantz, C., Kuhn, B. & Stahl, M. A medicinal chemist's guide to molecular interactions. J. Med. Chem. 53, 5061–5084 (2010).
Kuhn, B., Mohr, P. & Stahl, M. Intramolecular hydrogen bonding in medicinal chemistry. J. Med. Chem. 53, 2601–2611 (2010).
Adams, K.N. et al. Drug tolerance in replicating mycobacteria mediated by a macrophage-induced efflux mechanism. Cell 145, 39–53 (2011).
Lee, R.E., Brennan, P.J. & Besra, G.S. Mycobacterium tuberculosis cell envelope. Curr. Top. Microbiol. Immunol. 215, 1–27 (1996).
Akbergenov, R. et al. Molecular basis for the selectivity of antituberculosis compounds capreomycin and viomycin. Antimicrob. Agents Chemother. 55, 4712–4717 (2011).
Dartois, V. & Barry, C.E. III. A medicinal chemists' guide to the unique difficulties of lead optimization for tuberculosis. Bioorg. Med. Chem. Lett. 23, 4741–4750 (2013).
Louw, G.E. et al. Rifampicin reduces susceptibility to ofloxacin in rifampicin-resistant Mycobacterium tuberculosis through efflux. Am. J. Respir. Crit. Care Med. 184, 269–276 (2011).
Siddiqi, N. et al. Mycobacterium tuberculosis isolate with a distinct genomic identity overexpresses a tap-like efflux pump. Infection 32, 109–111 (2004).
Madhura, D.B., Lee, R. & Meibohm, B. Pharmacokinetic profile of spectinomycin in rats. Pharmazie 68, 675–676 (2013).
Case, D.A. et al. AMBER 11. (University of California, San Francisco, 2010).
Clinical Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard M7–A7 (Clinical Laboratory Standards Institute, Wayne, PA, 2006).
Hurdle, J.G. et al. A microbiological assessment of novel nitrofuranylamides as antituberculosis agents. J. Antimicrob. Chemother. 62, 1037–1045 (2008).
Mallari, J.P. et al. Development of potent purine-derived nitrile inhibitors of the trypanosomal protease TbcatB. J. Med. Chem. 51, 545–552 (2008).
Springer, B., Lucke, K., Calligaris-Maibach, R., Ritter, C. & Bottger, E.C. Quantitative drug susceptibility testing of Mycobacterium tuberculosis by use of MGIT 960 and EpiCenter instrumentation. J. Clin. Microbiol. 47, 1773–1780 (2009).
Bruell, C.M. et al. Conservation of bacterial protein synthesis machinery: initiation and elongation in Mycobacterium smegmatis. Biochemistry 47, 8828–8839 (2008).
Pallotti, F. & Lenaz, G. Isolation and subfractionation of mitochondria from animal cells and tissue culture lines. Methods Cell Biol. 65, 1–35 (2001).
McKee, E.E., Grier, B.L., Thompson, G.S. & McCourt, J.D. Isolation and incubation conditions to study heart mitochondrial protein synthesis. Am. J. Physiol. 258, E492–E502 (1990).
Fernández-Silva, P., Acin-Perez, R., Fernandez-Vizarra, E., Perez-Martos, A. & Enriquez, J.A. In vivo and in organello analyses of mitochondrial translation. Methods Cell Biol. 80, 571–588 (2007).
Hornig-Do, H.T. et al. Nonsense mutations in the COX1 subunit impair the stability of respiratory chain complexes rather than their assembly. EMBO J. 31, 1293–1307 (2012).
Budha, N.R. et al. Pharmacokinetically-guided lead optimization of nitrofuranylamide antituberculosis agents. AAPS J. 10, 157–165 (2008).
Budha, N.R., Lee, R.B., Hurdle, J.G., Lee, R.E. & Meibohm, B. A simple in vitro PK/PD model system to determine time-kill curves of drugs against Mycobacteria. Tuberculosis (Edinb.) 89, 378–385 (2009).
Lenaerts, A.J., Degroote, M.A. & Orme, I.M. Preclinical testing of new drugs for tuberculosis: current challenges. Trends Microbiol. 16, 48–54 (2008).
De Groote, M.A. et al. Comparative studies evaluating mouse models used for efficacy testing of experimental drugs against Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 55, 1237–1247 (2011).
De Groote, M.A. et al. Importance of confirming data on the in vivo efficacy of novel antibacterial drug regimens against various strains of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 56, 731–738 (2012).
Gonzalez-Juarrero, M., Woolhiser, L.K., Brooks, E., DeGroote, M.A. & Lenaerts, A.J. Mouse model for efficacy testing of antituberculosis agents via intrapulmonary delivery. Antimicrob. Agents Chemother. 56, 3957–3959 (2012).
Ordway, D. et al. XCL1 (lymphotactin) chemokine produced by activated CD8 T cells during the chronic stage of infection with Mycobacterium tuberculosis negatively affects production of IFN-γ by CD4 T cells and participates in granuloma stability. J. Leukoc. Biol. 82, 1221–1229 (2007).
Rosas-Taraco, A.G. et al. Intrapulmonary delivery of XCL1-targeting small interfering RNA in mice chronically infected with Mycobacterium tuberculosis. Am. J. Respir. Cell Mol. Biol. 41, 136–145 (2009).
Rosas-Taraco, A.G. et al. Local pulmonary immunotherapy with siRNA targeting TGFβ1 enhances antimicrobial capacity in Mycobacterium tuberculosis infected mice. Tuberculosis (Edinb.) 91, 98–106 (2011).
Acknowledgements
This study was supported by US National Institutes of Health (NIH) grant AI090810 (R.E.L., E.C.B., A.J.L. and B.M.), the National Institute of Allergy and Infectious Diseases (NIAID) Indefinite Delivery Indefinite Quantity (IDIQ) (R.E.L. and M.G.) Contract Task Order HHSN272201000009I/01, the American Lebanese Syrian Associated Charities (ALSAC) and St. Jude Children's Research Hospital (SJCRH) (R.E.L.) and in part by the Intramural Research Program of the NIAID, NIH (H.I.B.) and the Spanish Government (grant BIO-2009-09405) (J.A.A.). We thank L. Yang and J. Scarborough from SJCRH for their help with analysis of the final compounds, M. Maddox from SJCRH for technical assistance in determining MIC values, J. Ryman from the University of Tennessee Health Science Center for technical assistance in the performance of pharmacokinetic studies in mice, M. Butler from Microbiotix for coordination of the MDR tuberculosis testing and E. Tuomanen from SJCRH for critical evaluation of this manuscript.
Author information
Authors and Affiliations
Contributions
R.E.L. designed the compound series. J.G.H., D.F.B., R.B.L. and H.I.B. performed MIC testing and microbiology studies. J.L., J.Q., R., S.L.W. and D.S. performed the medicinal chemistry. T.M., R.A. and E.C.B. designed and performed MIC testing and ribosome inhibition studies. M.S.S., M.R.M., M.G.-J. and A.J.L. designed and performed the in vivo efficacy trials. P.K.V., C.R., D.B.M., A.T. and B.M. designed and performed the pharmacokinetic analysis. Z.Z. and S.D. performed the molecular modeling experiments. C.V., D.F.B. and J.A.A. designed and performed the efflux mutant testing. All authors discussed and analyzed the data. R.E.L., E.C.B., A.J.L., R.B.L., D.F.B., J.A.A. and B.M. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
R.E.L., J.Q., J.G.H., B.M., P.K.V., R. and J.L. disclose intellectual property rights ownership associated with the spectinamide series.
Supplementary information
Supplementary Text and Figures
Supplementary Scheme 1, Supplementary Analytical Data, Supplementary Tables 1–12 and Supplementary Figures 1–3 (PDF 1822 kb)
Rights and permissions
About this article
Cite this article
Lee, R., Hurdle, J., Liu, J. et al. Spectinamides: a new class of semisynthetic antituberculosis agents that overcome native drug efflux. Nat Med 20, 152–158 (2014). https://doi.org/10.1038/nm.3458
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.3458
This article is cited by
-
Anti-tuberculosis treatment strategies and drug development: challenges and priorities
Nature Reviews Microbiology (2022)
-
Discovery of a highly potent novel rifampicin analog by preparing a hybrid of the precursors of the antibiotic drugs rifampicin and clofazimine
Scientific Reports (2021)
-
Synthesis, antibacterial action, and ribosome inhibition of deoxyspectinomycins
The Journal of Antibiotics (2021)
-
Potential anti-TB investigational compounds and drugs with repurposing potential in TB therapy: a conspectus
Applied Microbiology and Biotechnology (2020)
-
Aminomethyl spectinomycins: a novel antibacterial chemotype for biothreat pathogens
The Journal of Antibiotics (2019)