Abstract
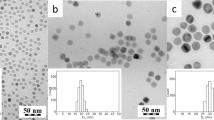
We report on a new straightforward magnetic cell-labeling approach that combines three US Food and Drug Administration (FDA)-approved drugs—ferumoxytol, heparin and protamine—in serum-free medium to form self-assembling nanocomplexes that effectively label cells for in vivo magnetic resonance imaging (MRI). We observed that the ferumoxytol-heparin-protamine (HPF) nanocomplexes were stable in serum-free cell culture medium. HPF nanocomplexes show a threefold increase in T2 relaxivity compared to ferumoxytol. Electron microscopy showed internalized HPF in endosomes, which we confirmed by Prussian blue staining of labeled cells. There was no long-term effect or toxicity on cellular physiology or function of HPF-labeled hematopoietic stem cells, bone marrow stromal cells, neural stem cells or T cells when compared to controls. In vivo MRI detected 1,000 HPF-labeled cells implanted in rat brains. This HPF labeling method should facilitate the monitoring by MRI of infused or implanted cells in clinical trials.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Daley, G.Q. Prospects for stem cell therapeutics: myths and medicines. Curr. Opin. Genet. Dev. 12, 607–613 (2002).
Mooney, D.J. & Vandenburgh, H. Cell delivery mechanisms for tissue repair. Cell Stem Cell 2, 205–213 (2008).
Motaln, H., Schichor, C. & Lah, T.T. Human mesenchymal stem cells and their use in cell-based therapies. Cancer 116, 2519–2530 (2010).
Arbab, A.S. et al. In vivo cellular imaging for translational medical research. Curr. Med. Imaging Rev. 5, 19–38 (2009).
Modo, M. Noninvasive imaging of transplanted cells. Curr. Opin. Organ Transplant. 13, 654–658 (2008).
Yaghoubi, S.S. & Gambhir, S.S. PET imaging of herpes simplex virus type 1 thymidine kinase (HSV1-tk) or mutant HSV1-sr39tk reporter gene expression in mice and humans using [18F]FHBG. Nat. Protoc. 1, 3069–3075 (2006).
Bulte, J.W. In vivo MRI cell tracking: clinical studies. AJR Am. J. Roentgenol. 193, 314–325 (2009).
Schwenk, M.H. Ferumoxytol: a new intravenous iron preparation for the treatment of iron deficiency anemia in patients with chronic kidney disease. Pharmacotherapy 30, 70–79 (2010).
Ferumoxytol (Feraheme)—a new parenteral iron formulation. Med. Lett. Drugs Ther. 52, 23 (2010).
Auerbach, M. Ferumoxytol as a new, safer, easier-to-administer intravenous iron: yes or no? Am. J. Kidney Dis. 52, 826–829 (2008).
Provenzano, R. et al. Ferumoxytol as an intravenous iron replacement therapy in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 4, 386–393 (2009).
Santoro, L. et al. Resovist enhanced MR imaging of the liver: does quantitative assessment help in focal lesion classification and characterization? J. Magn. Reson. Imaging 30, 1012–1020 (2009).
Neuwelt, E.A. et al. Ultrasmall superparamagnetic iron oxides (USPIOs): a future alternative magnetic resonance (MR) contrast agent for patients at risk for nephrogenic systemic fibrosis (NSF)? Kidney Int. 75, 465–474 (2009).
Corot, C., Robert, P., Idee, J.M. & Port, M. Recent advances in iron oxide nanocrystal technology for medical imaging. Adv. Drug Deliv. Rev. 58, 1471–1504 (2006).
Boutry, S. et al. Magnetic labeling of non-phagocytic adherent cells with iron oxide nanoparticles: a comprehensive study. Contrast Media Mol. Imaging 3, 223–232 (2008).
Arbab, A.S. et al. Efficient magnetic cell labeling with protamine sulfate complexed to ferumoxides for cellular MRI. Blood 104, 1217–1223 (2004).
Arbab, A.S. et al. Comparison of transfection agents in forming complexes with ferumoxides, cell labeling efficiency, and cellular viability. Mol. Imaging 3, 24–32 (2004).
Golovko, D.M. et al. Accelerated stem cell labeling with ferucarbotran and protamine. Eur. Radiol. 20, 640–648 (2010).
Walczak, P., Kedziorek, D.A., Gilad, A.A., Lin, S. & Bulte, J.W. Instant MR labeling of stem cells using magnetoelectroporation. Magn. Reson. Med. 54, 769–774 (2005).
Xie, D. et al. Optimization of magnetosonoporation for stem cell labeling. NMR Biomed. 23, 480–484 (2010).
Josephson, L., Tung, C.H., Moore, A. & Weissleder, R. High-efficiency intracellular magnetic labeling with novel superparamagnetic-Tat peptide conjugates. Bioconjug. Chem. 10, 186–191 (1999).
Janic, B. et al. Optimization and validation of FePro cell labeling method. PLoS ONE 4, e5873 (2009).
Balakumaran, A. et al. Superparamagnetic iron oxide nanoparticles labeling of bone marrow stromal (mesenchymal) cells does not affect their “stemness”. PLoS ONE 5, e11462 (2010).
Neuwelt, E.A. et al. The potential of ferumoxytol nanoparticle magnetic resonance imaging, perfusion, and angiography in central nervous system malignancy: a pilot study. Neurosurgery 60, 601–611 (2007).
Aborg, C.H. & Uvnas, B. Mode of binding of histamine and some other biogenic amines to a protamine-heparin complex in vitro. Acta Physiol. Scand. 74, 552–567 (1968).
Liang, J.F., Song, H., Li, Y.T. & Yang, V.C. A novel heparin/protamine-based pro-drug type delivery system for protease drugs. J. Pharm. Sci. 89, 664–673 (2000).
Liang, J.F. et al. ATTEMPTS: a heparin/protamine-based delivery system for enzyme drugs. J. Control. Release 78, 67–79 (2002).
Kemp, M.M. & Linhardt, R.J. Heparin-based nanoparticles. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2, 77–87 (2010).
Rossmann, P., Matousovic, K. & Horacek, V. Protamine-heparin aggregates. Their fine structure, histochemistry, and renal deposition. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 40, 81–98 (1982).
Liu, W. & Frank, J.A. Detection and quantification of magnetically labeled cells by cellular MRI. Eur. J. Radiol. 70, 258–264 (2009).
Khurshid, H. Development of heparin-coated nanoparticles for targeted drug delivery applications. J. Appl. Phys. 105, 07B308 (2009).
Castaneda, R.T., Khurana, A., Khan, R. & Daldrup-Link, H.E. Labeling stem cells with ferumoxytol, an FDA-approved iron oxide nanoparticle. J. Vis. Exp. 4, e3482 (2011).
Pawelczyk, E., Arbab, A.S., Pandit, S., Hu, E. & Frank, J.A. Expression of transferrin receptor and ferritin following ferumoxides-protamine sulfate labeling of cells: implications for cellular magnetic resonance imaging. NMR Biomed. 19, 581–592 (2006).
Arbab, A.S. et al. A model of lysosomal metabolism of dextran coated superparamagnetic iron oxide (SPIO) nanoparticles: implications for cellular magnetic resonance imaging. NMR Biomed. 18, 383–389 (2005).
Walczak, P., Kedziorek, D.A., Gilad, A.A., Barnett, B.P. & Bulte, J.W. Applicability and limitations of MR tracking of neural stem cells with asymmetric cell division and rapid turnover: the case of the shiverer dysmyelinated mouse brain. Magn. Reson. Med. 58, 261–269 (2007).
Pawelczyk, E. et al. In vivo uptake of intracellular label by tissue macrophages from prelabeled bone marrow stromal cells: quantitative analysis and implications for cellular therapy. PLoS ONE 4, e6712 (2009).
Oude Engberink, R.D., van der Pol, S.M., Dopp, E.A., de Vries, H.E. & Blezer, E.L. Comparison of SPIO and USPIO for in vitro labeling of human monocytes: MR detection and cell function. Radiology 243, 467–474 (2007).
Rad, A.M., Janic, B., Iskander, A.S., Soltanian-Zadeh, H. & Arbab, A.S. Measurement of quantity of iron in magnetically labeled cells: comparison among different UV/VIS spectrometric methods. Biotechniques 43, 627–628, 630, 632 passim (2007).
Acknowledgements
This work was supported by and performed in part in the intramural research program at the Clinical Center of the US National Institutes of Health (NIH). BMSCs were provided from the Center for Bone Marrow Stromal Cell Transplantation at the NIH. NSCs were provided as part of a material transfer agreement with K. Aboody (City of Hope Medical Center). The authors would like to acknowledge the Clinical Image Processing Section at the NIH. This work was also supported by NIH grant R01CA122031.
Author information
Authors and Affiliations
Contributions
J.A.F., M.S.T. and L.H.B. were guarantors of integrity of entire study; J.A.F. and M.S.T. conceptualized and designed the study; M.S.T., L.H.B., E.K.J., B.K.L., A.C., M.D.B., N.R.S.V., J.R., T.C. and A.S.A. performed experiments; J.A.F., M.S.T., L.H.B., E.K.J., J.R. and A.S.A. analyzed and interpreted the data; J.A.F., M.S.T. and L.H.B. drafted the manuscript or revised for important intellectual content; all authors approved the manuscript; M.S.T. performed statistical analysis; J.A.F. and M.S.T. edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–5, Supplementary Table 1 and Supplementary Methods (PDF 14869 kb)
Rights and permissions
About this article
Cite this article
Thu, M., Bryant, L., Coppola, T. et al. Self-assembling nanocomplexes by combining ferumoxytol, heparin and protamine for cell tracking by magnetic resonance imaging. Nat Med 18, 463–467 (2012). https://doi.org/10.1038/nm.2666
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.2666
This article is cited by
-
Advances in magnetic nanoparticle-based magnetic resonance imaging contrast agents
Nano Research (2023)
-
Angiogenic stem cell delivery platform to augment post-infarction neovasculature and reverse ventricular remodeling
Scientific Reports (2022)
-
Cell sorting microbeads as novel contrast agent for magnetic resonance imaging
Scientific Reports (2022)
-
Tracking Neural Stem Cells in vivo: Achievements and Limitations
Stem Cell Reviews and Reports (2022)
-
The sensitivity of magnetic particle imaging and fluorine-19 magnetic resonance imaging for cell tracking
Scientific Reports (2021)