Abstract
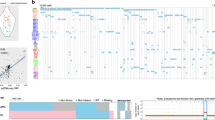
To elucidate differential roles of mutations in myelodysplastic syndromes (MDS), we investigated clonal dynamics using whole-exome and/or targeted sequencing of 699 patients, of whom 122 were analyzed longitudinally. Including the results from previous reports, we assessed a total of 2,250 patients for mutational enrichment patterns. During progression, the number of mutations, their diversity and clone sizes increased, with alterations frequently present in dominant clones with or without their sweeping previous clones. Enriched in secondary acute myeloid leukemia (sAML; in comparison to high-risk MDS), FLT3, PTPN11, WT1, IDH1, NPM1, IDH2 and NRAS mutations (type 1) tended to be newly acquired, and were associated with faster sAML progression and a shorter overall survival time. Significantly enriched in high-risk MDS (in comparison to low-risk MDS), TP53, GATA2, KRAS, RUNX1, STAG2, ASXL1, ZRSR2 and TET2 mutations (type 2) had a weaker impact on sAML progression and overall survival than type-1 mutations. The distinct roles of type-1 and type-2 mutations suggest their potential utility in disease monitoring.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Accession codes
References
Harris, N.L. et al. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting–Airlie House, Virginia, November 1997. J. Clin. Oncol. 17, 3835–3849 (1999).
Vardiman, J.W. et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114, 937–951 (2009).
Malcovati, L. et al. Prognostic factors and life expectancy in myelodysplastic syndromes classified according to WHO criteria: a basis for clinical decision making. J. Clin. Oncol. 23, 7594–7603 (2005).
Cancer Genome Atlas Research Network. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N. Engl. J. Med. 368, 2059–2074 (2013).
Mardis, E.R. et al. Recurring mutations found by sequencing an acute myeloid leukemia genome. N. Engl. J. Med. 361, 1058–1066 (2009).
Ley, T.J. et al. DNMT3A mutations in acute myeloid leukemia. N. Engl. J. Med. 363, 2424–2433 (2010).
Delhommeau, F. et al. Mutation in TET2 in myeloid cancers. N. Engl. J. Med. 360, 2289–2301 (2009).
Papaemmanuil, E. et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N. Engl. J. Med. 365, 1384–1395 (2011).
Yoshida, K. et al. Frequent pathway mutations of splicing machinery in myelodysplasia. Nature 478, 64–69 (2011).
Gelsi-Boyer, V. et al. Mutations of Polycomb-associated gene ASXL1 in myelodysplastic syndromes and chronic myelomonocytic leukaemia. Br. J. Haematol. 145, 788–800 (2009).
Grossmann, V. et al. Whole-exome sequencing identifies somatic mutations of BCOR in acute myeloid leukemia with normal karyotype. Blood 118, 6153–6163 (2011).
Sanada, M. et al. Gain-of-function of mutated C-CBL tumour suppressor in myeloid neoplasms. Nature 460, 904–908 (2009).
Ernst, T. et al. Inactivating mutations of the histone methyltransferase gene EZH2 in myeloid disorders. Nat. Genet. 42, 722–726 (2010).
Maxson, J.E. et al. Oncogenic CSF3R mutations in chronic neutrophilic leukemia and atypical CML. N. Engl. J. Med. 368, 1781–1790 (2013).
Makishima, H. et al. Somatic SETBP1 mutations in myeloid malignancies. Nat. Genet. 45, 942–946 (2013).
Kurtovic-Kozaric, A. et al. PRPF8 defects cause missplicing in myeloid malignancies. Leukemia 29, 126–136 (2015).
Huang, D. et al. BRCC3 mutations in myeloid neoplasms. Haematologica 100, 1051–1057 (2015).
Walter, M.J. et al. Clonal architecture of secondary acute myeloid leukemia. N. Engl. J. Med. 366, 1090–1098 (2012).
Walter, M.J. et al. Clonal diversity of recurrently mutated genes in myelodysplastic syndromes. Leukemia 27, 1275–1282 (2013).
Lindsley, R.C. et al. Acute myeloid leukemia ontogeny is defined by distinct somatic mutations. Blood 125, 1367–1376 (2015).
Bejar, R. et al. Clinical effect of point mutations in myelodysplastic syndromes. N. Engl. J. Med. 364, 2496–2506 (2011).
Bejar, R. et al. Validation of a prognostic model and the impact of mutations in patients with lower-risk myelodysplastic syndromes. J. Clin. Oncol. 30, 3376–3382 (2012).
Haferlach, T. et al. Landscape of genetic lesions in 944 patients with myelodysplastic syndromes. Leukemia 28, 241–247 (2014).
Papaemmanuil, E. et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood 122, 3616–3627, quiz 3699 (2013).
Rocquain, J. et al. Combined mutations of ASXL1, CBL, FLT3, IDH1, IDH2, JAK2, KRAS, NPM1, NRAS, RUNX1, TET2 and WT1 genes in myelodysplastic syndromes and acute myeloid leukemias. BMC Cancer 10, 401 (2010).
Roth, A. et al. PyClone: statistical inference of clonal population structure in cancer. Nat. Methods 11, 396–398 (2014).
Badar, T. et al. Detectable FLT3-ITD or RAS mutation at the time of transformation from MDS to AML predicts for very poor outcomes. Leuk. Res. 39, 1367–1374 (2015).
Schnittger, S. et al. Characterization of NPM1-mutated AML with a history of myelodysplastic syndromes or myeloproliferative neoplasms. Leukemia 25, 615–621 (2011).
Shih, L.Y. et al. Acquisition of FLT3 or N-ras mutations is frequently associated with progression of myelodysplastic syndrome to acute myeloid leukemia. Leukemia 18, 466–475 (2004).
Dicker, F. et al. Mutation analysis for RUNX1, MLL-PTD, FLT3-ITD, NPM1 and NRAS in 269 patients with MDS or secondary AML. Leukemia 24, 1528–1532 (2010).
Malcovati, L. et al. Clinical significance of SF3B1 mutations in myelodysplastic syndromes and myelodysplastic/myeloproliferative neoplasms. Blood 118, 6239–6246 (2011).
Makishima, H. et al. Mutations in the spliceosome machinery, a novel and ubiquitous pathway in leukemogenesis. Blood 119, 3203–3210 (2012).
Malcovati, L. et al. SF3B1 mutation identifies a distinct subset of myelodysplastic syndrome with ring sideroblasts. Blood 126, 233–241 (2015).
Busque, L. et al. Recurrent somatic TET2 mutations in normal elderly individuals with clonal hematopoiesis. Nat. Genet. 44, 1179–1181 (2012).
Genovese, G. et al. Clonal hematopoiesis and blood-cancer risk inferred from blood DNA sequence. N. Engl. J. Med. 371, 2477–2487 (2014).
Xie, M. et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat. Med. 20, 1472–1478 (2014).
Jaiswal, S. et al. Age-related clonal hematopoiesis associated with adverse outcomes. N. Engl. J. Med. 371, 2488–2498 (2014).
Shlush, L.I. et al. Identification of pre-leukaemic haematopoietic stem cells in acute leukaemia. Nature 506, 328–333 (2014).
Gilliland, D.G. & Griffin, J.D. The roles of FLT3 in hematopoiesis and leukemia. Blood 100, 1532–1542 (2002).
Fröhling, S., Scholl, C., Gilliland, D.G. & Levine, R.L. Genetics of myeloid malignancies: pathogenetic and clinical implications. J. Clin. Oncol. 23, 6285–6295 (2005).
Kihara, R. et al. Comprehensive analysis of genetic alterations and their prognostic impacts in adult acute myeloid leukemia patients. Leukemia 28, 1586–1595 (2014).
Merlevede, J. et al. Mutation allele burden remains unchanged in chronic myelomonocytic leukaemia responding to hypomethylating agents. Nat. Commun. 7, 10767 (2016).
Yoshida, K. et al. The landscape of somatic mutations in Down syndrome–related myeloid disorders. Nat. Genet. 45, 1293–1299 (2013).
Kon, A. et al. Recurrent mutations in multiple components of the cohesin complex in myeloid neoplasms. Nat. Genet. 45, 1232–1237 (2013).
Dunbar, A.J. et al. 250K single nucleotide polymorphism array karyotyping identifies acquired uniparental disomy and homozygous mutations, including novel missense substitutions of c-Cbl, in myeloid malignancies. Cancer Res. 68, 10349–10357 (2008).
Jankowska, A.M. et al. Loss of heterozygosity 4q24 and TET2 mutations associated with myelodysplastic/myeloproliferative neoplasms. Blood 113, 6403–6410 (2009).
Makishima, H. et al. CBL, CBLB, TET2, ASXL1, and IDH1/2 mutations and additional chromosomal aberrations constitute molecular events in chronic myelogenous leukemia. Blood 117, e198–e206 (2011).
Makishima, H. et al. Mutations of E3 ubiquitin ligase Cbl family members constitute a novel common pathogenic lesion in myeloid malignancies. J. Clin. Oncol. 27, 6109–6116 (2009).
Huh, J. et al. Characterization of chromosome arm 20q abnormalities in myeloid malignancies using genome-wide single nucleotide polymorphism array analysis. Genes Chromosom. Cancer 49, 390–399 (2010).
Tiu, R.V. et al. New lesions detected by single nucleotide polymorphism array-based chromosomal analysis have important clinical impact in acute myeloid leukemia. J. Clin. Oncol. 27, 5219–5226 (2009).
Nannya, Y. et al. A robust algorithm for copy number detection using high-density oligonucleotide single nucleotide polymorphism genotyping arrays. Cancer Res. 65, 6071–6079 (2005).
Sato, Y. et al. Integrated molecular analysis of clear-cell renal cell carcinoma. Nat. Genet. 45, 860–867 (2013).
Shah, S.P. et al. The clonal and mutational evolution spectrum of primary triple-negative breast cancers. Nature 486, 395–399 (2012).
Suzuki, H. et al. Mutational landscape and clonal architecture in grade II and III gliomas. Nat. Genet. 47, 458–468 (2015).
Tibshirani, R. Regression shrinkage and selection via the Lasso. J. R. Stat. Soc. Series B Stat. Methodol. 58, 267–288 (1996).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. B 57, 289–300 (1995).
Acknowledgements
This work was supported by US National Institutes of Health (NIH) grants RO1HL-082983 (J.P.M.), U54 RR019391 (J.P.M.) and K24 HL-077522 (J.P.M.), a grant from the AA & MDS International Foundation (J.P.M., M.A.S. and H.M.), the Robert Duggan Charitable Fund (J.P.M.), a grant from Edward P. Evans Foundation (J.P.M. and M.A.S.), Scott Hamilton CARES grant (H.M.), Grant-in-Aids from the Ministry of Health, Labor and Welfare of Japan, the Japanese Agency for Medical Research and Development (Health and Labour Sciences Research Expenses for Commission and Applied Research for Innovative Treatment of Cancer) and KAKENHI (26221308, 23249052, 22134006, 15H05909, hp160219 and 21790907; S.O.), (15km0305018h0101, 16H05338; H.M.), (26890016; K.Y.), project for development of innovative research on cancer therapies (FIRST, p-direct; S.O.), the Japan Society for the Promotion of Science (JSPS) through the 'Funding Program for World-Leading Innovative R&D on Science and Technology', initiated by the Council for Science and Technology Policy (CSTP) (S.O.), NHRI-EX100-10003NI Taiwan (L.-Y.S.), National Aeronautics and Space Administration grant NNJ13ZSA001N (T.R.), and a grant from the American Cancer Society (Research Scholar Grant 123436-RSG-12-159-01-DMC, to T.L.). Supercomputing resources were also provided by the Human Genome Center, the Institute of Medical Science, The University of Tokyo.
Author information
Authors and Affiliations
Contributions
H.M.: project leader, analysis coordination, variant validation production and manuscript preparation. T.Y.: project leader, sequence analysis, microarray data analysis and manuscript preparation. K.Y.: data analysis team and variant validation production. M.A.S.: clinical data and specimen acquisition and manuscript preparation. T.R.: data analysis, manuscript preparation. H.S.: data analysis team and variant validation production. B.P.: supervisor data analysis team and variant validation production. Y.N.: hybridization-based capture next-generation platform development. M.M.: clinical data and specimen acquisition, data analysis. M.S.: sequence analysis. Y.O.: auto-analysis and manuscript preparation. C. Hirsch: clinical data and specimen acquisition, data analysis. T.K.: clinical data and specimen acquisition, data analysis. Y. Sato: microarray data analysis. A.S.-O.: data management, data analysis. T.L.: data analysis and manuscript preparation. N.H.: variant validation production. Y. Shiraishi: data management, data analysis. K.C.: data management, data analysis. C. Haferlach: clinical data and specimen acquisition, data analysis. W.K.: clinical data and specimen acquisition, data analysis. H.T.: data management, data analysis. Y. Shiozawa: data analysis. I.G.-S.: clinical data management. H.D.H.: clinical data management. S.T.: clinical data management. K.M.G.: specimen acquisition. B.D.: specimen acquisition. T.N.: clinical data management and specimen acquisition. S. Miyawaki: clinical data management and specimen acquisition. Y. Saunthararajah: clinical data management and specimen acquisition. S.C.: clinical data management and specimen acquisition. S. Miyano: data management, data analysis automation leader. L.-Y.S.: clinical data and specimen acquisition, study design. T.H.: clinical data and specimen acquisition, study design. S.O. and J.P.M.: project leaders, study design, execution and analysis, manuscript preparation.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–19 and Supplementary Tables 1–7. (PDF 13467 kb)
Rights and permissions
About this article
Cite this article
Makishima, H., Yoshizato, T., Yoshida, K. et al. Dynamics of clonal evolution in myelodysplastic syndromes. Nat Genet 49, 204–212 (2017). https://doi.org/10.1038/ng.3742
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.3742
This article is cited by
-
Decoding leukemia at the single-cell level: clonal architecture, classification, microenvironment, and drug resistance
Experimental Hematology & Oncology (2024)
-
Role of reactive oxygen species in myelodysplastic syndromes
Cellular & Molecular Biology Letters (2024)
-
The role of genetic factors in pediatric myelodysplastic syndromes with different outcomes
BMC Pediatrics (2024)
-
Recent advances in targeted therapies in acute myeloid leukemia
Journal of Hematology & Oncology (2023)
-
Novel scheme for defining the clinical implications of TP53 mutations in myeloid neoplasia
Journal of Hematology & Oncology (2023)