Abstract
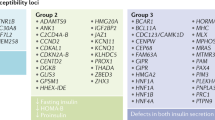
Type 1 (T1D) and type 2 (T2D) diabetes share pathophysiological characteristics, yet mechanistic links have remained elusive. T1D results from autoimmune destruction of pancreatic beta cells, whereas beta cell failure in T2D is delayed and progressive. Here we find a new genetic component of diabetes susceptibility in T1D non-obese diabetic (NOD) mice, identifying immune-independent beta cell fragility. Genetic variation in Xrcc4 and Glis3 alters the response of NOD beta cells to unfolded protein stress, enhancing the apoptotic and senescent fates. The same transcriptional relationships were observed in human islets, demonstrating the role of beta cell fragility in genetic predisposition to diabetes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Wicker, L.S. et al. Type 1 diabetes genes and pathways shared by humans and NOD mice. J. Autoimmun. 25 (suppl.) 29–33 (2005).
Islam, M.S. & Wilson, R.D. Experimentally induced rodent models of type 2 diabetes. Methods Mol. Biol. 933, 161–174 (2012).
Butler, A.E. et al. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 52, 102–110 (2003).
Bradfield, J.P. et al. A genome-wide meta-analysis of six type 1 diabetes cohorts identifies multiple associated loci. PLoS Genet. 7, e1002293 (2011).
DIAbetes Genetics Replication And Meta-analysis (DIAGRAM) Consortium, Asian Genetic Epidemiology Network Type 2 Diabetes (AGEN-T2D) Consortium, South Asian Type 2 Diabetes (SAT2D) Consortium, Mexican American Type 2 Diabetes (MAT2D) Consortium & Type 2 Diabetes Genetic Exploration by Nex-generation sequencing in muylti-Ethnic Samples (T2D-GENES) Consortium. Genome-wide trans-ancestry meta-analysis provides insight into the genetic architecture of type 2 diabetes susceptibility. Nat. Genet. 46, 234–244 (2014).
Fortune, M.D. et al. Statistical colocalization of genetic risk variants for related autoimmune diseases in the context of common controls. Nat. Genet. 47, 839–846 (2015).
Senée, V. et al. Mutations in GLIS3 are responsible for a rare syndrome with neonatal diabetes mellitus and congenital hypothyroidism. Nat. Genet. 38, 682–687 (2006).
Delépine, M. et al. EIF2AK3, encoding translation initiation factor 2-α kinase 3, is mutated in patients with Wolcott-Rallison syndrome. Nat. Genet. 25, 406–409 (2000).
Janssens, S., Pulendran, B. & Lambrecht, B.N. Emerging functions of the unfolded protein response in immunity. Nat. Immunol. 15, 910–919 (2014).
Tersey, S.A. et al. Islet beta-cell endoplasmic reticulum stress precedes the onset of type 1 diabetes in the nonobese diabetic mouse model. Diabetes 61, 818–827 (2012).
Engin, F. et al. Restoration of the unfolded protein response in pancreatic beta cells protects mice against type 1 diabetes. Sci. Transl. Med. 5, 211ra156 (2013).
Back, S.H. & Kaufman, R.J. Endoplasmic reticulum stress and type 2 diabetes. Annu. Rev. Biochem. 81, 767–793 (2012).
Planas, R., Pujol-Borrell, R. & Vives-Pi, M. Global gene expression changes in type 1 diabetes: insights into autoimmune response in the target organ and in the periphery. Immunol. Lett. 133, 55–61 (2010).
Chaparro, R.J. et al. Nonobese diabetic mice express aspects of both type 1 and type 2 diabetes. Proc. Natl. Acad. Sci. USA 103, 12475–12480 (2006).
Liston, A. et al. Generalized resistance to thymic deletion in the NOD mouse; a polygenic trait characterized by defective induction of Bim. Immunity 21, 817–830 (2004).
Liston, A., Lesage, S., Wilson, J., Peltonen, L. & Goodnow, C.C. Aire regulates negative selection of organ-specific T cells. Nat. Immunol. 4, 350–354 (2003).
Hill, S.W., Kipp, D.E., Melchers, I., Frelinger, J.A. & Sercarz, E.E. Multiple H-2 and non-H-2 genes controlling the antilysozyme response: alternative gene constellations can lead to responsiveness. Eur. J. Immunol. 10, 384–391 (1980).
Izumi, T. et al. Dominant negative pathogenesis by mutant proinsulin in the Akita diabetic mouse. Diabetes 52, 409–416 (2003).
Iwawaki, T., Akai, R., Kohno, K. & Miura, M. A transgenic mouse model for monitoring endoplasmic reticulum stress. Nat. Med. 10, 98–102 (2004).
Wicker, L.S., Todd, J.A. & Peterson, L.B. Genetic control of autoimmune diabetes in the NOD mouse. Annu. Rev. Immunol. 13, 179–200 (1995).
Puebla-Osorio, N. et al. A novel Ku70 function in colorectal homeostasis separate from nonhomologous end joining. Oncogene 33, 2748–2757 (2014).
Tavana, O., Puebla-Osorio, N., Sang, M. & Zhu, C. Absence of p53-dependent apoptosis combined with nonhomologous end-joining deficiency leads to a severe diabetic phenotype in mice. Diabetes 59, 135–142 (2010).
Nijnik, A. et al. DNA repair is limiting for haematopoietic stem cells during ageing. Nature 447, 686–690 (2007).
Nogueira, T.C. et al. GLIS3, a susceptibility gene for type 1 and type 2 diabetes, modulates pancreatic beta cell apoptosis via regulation of a splice variant of the BH3-only protein Bim. PLoS Genet. 9, e1003532 (2013).
Lindahl, M. et al. MANF is indispensable for the proliferation and survival of pancreatic beta cells. Cell Reports 7, 366–375 (2014).
Hall, E. et al. Effects of palmitate on genome-wide mRNA expression and DNA methylation patterns in human pancreatic islets. BMC Med. 12, 103 (2014).
Sone, H. & Kagawa, Y. Pancreatic beta cell senescence contributes to the pathogenesis of type 2 diabetes in high-fat diet–induced diabetic mice. Diabetologia 48, 58–67 (2005).
Fadista, J. et al. Global genomic and transcriptomic analysis of human pancreatic islets reveals novel genes influencing glucose metabolism. Proc. Natl. Acad. Sci. USA 111, 13924–13929 (2014).
Leiter, E.H. et al. Unexpected functional consequences of xenogeneic transgene expression in beta-cells of NOD mice. Diabetes Obes. Metab. 9 (suppl. 2), 14–22 (2007).
McCullough, K.D., Martindale, J.L., Klotz, L.O., Aw, T.Y. & Holbrook, N.J. Gadd153 sensitizes cells to endoplasmic reticulum stress by down-regulating Bcl2 and perturbing the cellular redox state. Mol. Cell. Biol. 21, 1249–1259 (2001).
Apostolou, A., Shen, Y., Liang, Y., Luo, J. & Fang, S. Armet, a UPR-upregulated protein, inhibits cell proliferation and ER stress–induced cell death. Exp. Cell Res. 314, 2454–2467 (2008).
Davenport, E.L. et al. Heat shock protein inhibition is associated with activation of the unfolded protein response pathway in myeloma plasma cells. Blood 110, 2641–2649 (2007).
Neuber, O., Jarosch, E., Volkwein, C., Walter, J. & Sommer, T. Ubx2 links the Cdc48 complex to ER-associated protein degradation. Nat. Cell Biol. 7, 993–998 (2005).
Leitman, J. et al. Herp coordinates compartmentalization and recruitment of HRD1 and misfolded proteins for ERAD. Mol. Biol. Cell 25, 1050–1060 (2014).
Liston, A. et al. Gene dosage—limiting role of Aire in thymic expression, clonal deletion, and organ-specific autoimmunity. J. Exp. Med. 200, 1015–1026 (2004).
Lesage, S. et al. Failure to censor forbidden clones of CD4 T cells in autoimmune diabetes. J. Exp. Med. 196, 1175–1188 (2002).
Wick, G. et al. The role of genetically-determined primary alterations of the target organ in the development of spontaneous autoimmune thyroiditis in obese strain (OS) chickens. Immunol. Rev. 94, 113–136 (1986).
DIAMOND Project Group. Incidence and trends of childhood type 1 diabetes worldwide 1990–1999. Diabet. Med. 23, 857–866 (2006).
Patterson, C.C., Dahlquist, G.G., Gyürüs, E., Green, A. & Soltész, G. Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet 373, 2027–2033 (2009).
TEDDY Study Group. The Environmental Determinants of Diabetes in the Young (TEDDY) Study. Ann. NY Acad. Sci. 1150, 1–13 (2008).
Laybutt, D.R. et al. Endoplasmic reticulum stress contributes to beta cell apoptosis in type 2 diabetes. Diabetologia 50, 752–763 (2007).
Oprescu, A.I. et al. Free fatty acid–induced reduction in glucose-stimulated insulin secretion: evidence for a role of oxidative stress in vitro and in vivo. Diabetes 56, 2927–2937 (2007).
Betts, P., Mulligan, J., Ward, P., Smith, B. & Wilkin, T. Increasing body weight predicts the earlier onset of insulin-dependant diabetes in childhood: testing the 'accelerator hypothesis' (2). Diabet. Med. 22, 144–151 (2005).
Gale, E.A. & Gillespie, K.M. Diabetes and gender. Diabetologia 44, 3–15 (2001).
Donahue, R.P., Bean, J.A., Donahue, R.A., Goldberg, R.B. & Prineas, R.J. Insulin response in a triethnic population: effects of sex, ethnic origin, and body fat. Miami Community Health Study. Diabetes Care 20, 1670–1676 (1997).
Zhou, R., Tardivel, A., Thorens, B., Choi, I. & Tschopp, J. Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nat. Immunol. 11, 136–140 (2010).
Cervin, C. et al. Genetic similarities between latent autoimmune diabetes in adults, type 1 diabetes, and type 2 diabetes. Diabetes 57, 1433–1437 (2008).
Podolin, P.L. et al. I-E+ nonobese diabetic mice develop insulitis and diabetes. J. Exp. Med. 178, 793–803 (1993).
Akkaraju, S. et al. A range of CD4 T cell tolerance: partial inactivation to organ-specific antigen allows nondestructive thyroiditis or insulitis. Immunity 7, 255–271 (1997).
Mombaerts, P. et al. RAG-1–deficient mice have no mature B and T lymphocytes. Cell 68, 869–877 (1992).
Ramsey, C. et al. Aire deficient mice develop multiple features of APECED phenotype and show altered immune response. Hum. Mol. Genet. 11, 397–409 (2002).
Prochazka, M., Gaskins, H.R., Shultz, L.D. & Leiter, E.H. The nonobese diabetic SCID mouse: model for spontaneous thymomagenesis associated with immunodeficiency. Proc. Natl. Acad. Sci. USA 89, 3290–3294 (1992).
Lyons, P.A. et al. The NOD Idd9 genetic interval influences the pathogenicity of insulitis and contains molecular variants of Cd30, Tnfr2, and Cd137. Immunity 13, 107–115 (2000).
Lyons, P.A. et al. Congenic mapping of the type 1 diabetes locus, Idd3, to a 780-kb region of mouse chromosome 3: identification of a candidate segment of ancestral DNA by haplotype mapping. Genome Res. 10, 446–453 (2000).
Hill, N.J. et al. NOD Idd5 locus controls insulitis and diabetes and overlaps the orthologous CTLA4/IDDM12 and NRAMP1 loci in humans. Diabetes 49, 1744–1747 (2000).
Mao, C., Dong, D., Little, E., Luo, S. & Lee, A.S. Transgenic mouse model for monitoring endoplasmic reticulum stress in vivo. Nat. Med. 10, 1013–1014 author reply 1014 (2004).
Kang, H.S. et al. Transcription factor Glis3, a novel critical player in the regulation of pancreatic beta-cell development and insulin gene expression. Mol. Cell. Biol. 29, 6366–6379 (2009).
Li, D.S., Yuan, Y.H., Tu, H.J., Liang, Q.L. & Dai, L.J. A protocol for islet isolation from mouse pancreas. Nat. Protoc. 4, 1649–1652 (2009).
Gysemans, C.A. et al. Disruption of the γ-interferon signaling pathway at the level of signal transducer and activator of transcription-1 prevents immune destruction of beta-cells. Diabetes 54, 2396–2403 (2005).
Kornete, M., Beauchemin, H., Polychronakos, C. & Piccirillo, C.A. Pancreatic islet cell phenotype and endocrine function throughout diabetes development in non-obese diabetic mice. Autoimmunity 46, 259–268 (2013).
Trapnell, C., Pachter, L. & Salzberg, S.L. TopHat: discovering splice junctions with RNA-Seq. Bioinformatics 25, 1105–1111 (2009).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl. Acad. Sci. USA 102, 15545–15550 (2005).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
DePristo, M.A. et al. A framework for variation discovery and genotyping using next-generation DNA sequencing data. Nat. Genet. 43, 491–498 (2011).
Robinson, M.D. & Oshlack, A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 11, R25 (2010).
Ghesquiere, B. et al. Redox proteomics of protein-bound methionine oxidation. Mol. Cell Proteomics 10, M110.006866 (2011).
Thimiri Govinda Raj, D.B. et al. A novel strategy for the comprehensive analysis of the biomolecular composition of isolated plasma membranes. Mol. Syst. Biol. 7, 541 (2011).
Helsens, K. et al. ms_lims, a simple yet powerful open source laboratory information management system for MS-driven proteomics. Proteomics 10, 1261–1264 (2010).
Sibanda, B.L. et al. Crystal structure of an Xrcc4–DNA ligase IV complex. Nat. Struct. Biol. 8, 1015–1019 (2001).
Jorgensen, W.L., Chandrasekhar, J., Madura, J.D., Impey, R.W. & Klein, M.L. Comparison of simple potential functions for simulating liquid water. J. Chem. Phys. 79, 926–935 (1983).
Duan, Y. et al. A point-charge force field for molecular mechanics simulations of proteins based on condensed-phase quantum mechanical calculations. J. Comput. Chem. 24, 1999–2012 (2003).
Cheatham, T.E., Miller, J.L., Fox, T., Darden, T.A. & Kollman, P.A. Molecular-dynamics simulations on solvated biomolecular systems—the particle mesh Ewald method leads to stable trajectories of DNA, RNA, and proteins. J. Am. Chem. Soc. 117, 4193–4194 (1995).
Ceriotti, M., Bussi, G. & Parrinello, M. Langevin equation with colored noise for constant-temperature molecular dynamics simulations. Phys. Rev. Lett. 102, 020601 (2009).
Feller, S.E., Zhang, Y.H., Pastor, R.W. & Brooks, B.R. Constant-pressure molecular-dynamics simulation—the Langevin piston method. J. Chem. Phys. 103, 4613–4621 (1995).
Ryckaert, J.P., Ciccotti, G. & Berendsen, H.J.C. Numerical-integration of Cartesian equations of motion of a system with constraints—molecular-dynamics of N-alkanes. J. Comput. Phys. 23, 327–341 (1977).
Miyamoto, S. & Kollman, P.A. Settle—an analytical version of the shake and rattle algorithm for rigid water models. J. Comput. Chem. 13, 952–962 (1992).
Acknowledgements
The authors thank P. Jeggo, C. Mathieu, D. Gray and A. Goris for critical insights and D. Pombal, J. Sreenivasan, A. Bullman, M. Koina and T. Dagpo for technical assistance. We acknowledge the Human Tissue Laboratory (HTL) of the Lund University Diabetes Centre (LUDC) for providing high-quality data from human pancreatic islets. This work was supported by the VIB, European Research Council (ERC) and a Juvenile Diabetes Research Foundation (JDRF) Career Development Award (A.L.) and by the National Health and Medical Research Council of Australia (project grant 1028108; C.J.N.). N.O. and V. Lyssenko acknowledge support by a Strategic Research Grant from the Swedish Research Council (2009-1039).
Author information
Authors and Affiliations
Contributions
A.L., S.M.S., S.L., N.P., C.J.N., D.R.L. and C.C.G. designed the study. J.D., L.T., S.S., V.D.-A., J.E.G.-P., E.P., D.D.M., D.F., L.O., J.V., G.C.-R., J.D., L.S., S.M.S., J.E.D. and A.L. performed the experiments. E.J.C., N.O., V. Lyssenko, V. Lagou, J.A., K.G., D.L., M.A.L. and A.L. analyzed results. A.M.J. provided reagents. A.L. wrote the manuscript. All authors discussed results and read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Equivalent islet insHEL expression on the B10 and NOD backgrounds.
RNA-seq was performed on the islets of wild-type (wt) B10k.Rag−/−, B10k.Rag−/−.insHEL, wt NODk.Rag−/− and (pre-diabetic) NODk.Rag−/−.insHEL mice (n = 3/group). (a) Reads were aligned to a custom genome build combining chicken chromosome 1 with the mouse genome, with normalized counts displayed for chicken Lyz, the gene encoding HEL. (b) Expression of H2k1, of which the transmembrane region is included in the insHEL construct to encode a membrane anchor. Means ± s.e.m.
Supplementary Figure 2 No effect of insHEL insertion on chemokine gene expression from the endogenous locus.
RNA-seq was performed on the islets of B10k.Rag−/−, B10k.Rag−/−.insHEL, NODk.Rag−/− and (pre-diabetic) NODk.Rag−/−.insHEL mice (n = 3/group). Expression of chemokines is given for each strain. Means ± s.e.m.: *P < 0.05.
Supplementary Figure 3 No effect of insHEL insertion on gene expression from the endogenous locus.
The gene insertion site of insHEL was defined by the congenic region remaining in the backcross to the NOD background. The outer boundaries of the integration site were identified on chromosome 12 (64,900,000–71,900,000). RNA-seq was performed on the islets of B10k.Rag−/−, B10k.Rag−/−.insHEL, NODk.Rag−/− and (pre-diabetic) NODk.Rag−/−.insHEL mice (n = 3/group). (a) Expression of genes within the integration boundaries in B10k.Rag−/− islets. (b) For all genes with reliable expression detection within the boundaries, the effect of insHEL expression was assessed as the expression in transgenic islets as a percentage of the expression in non-transgenic islets on the B10k strain (black), NODk strain (white) or average of the two strains (gray). No genes in the interval showed a significant change in expression.
Supplementary Figure 4 Altered insulin expression in the islets of insHEL transgenic mice.
(a) Immunofluorescence analysis was performed on the islets of wild-type (wt) B10k.Rag−/−, B10k.Rag−/−.insHEL, wt NODk.Rag−/− and (pre-diabetic) NODk.Rag−/−.insHEL mice with a polyclonal antibody to insulin, antibody to glucagon and DAPI. Staining is representative of three experiments. Scale bar, 100 μm. (b,c) RNA-seq analysis was performed on the islets of B10k.Rag−/−, B10k.Rag−/−.insHEL, NODk.Rag−/− and (pre-diabetic) NODk.Rag−/−.insHEL mice (n = 3/group). Expression is shown for Ins1 (b) and Ins2 (c). (d,e) ERAI mice were crossed to B10k.Rag−/−.insHEL and NODk.Rag−/−.insHEL mice, and islets were analyzed by flow cytometry. Histograms are shown of insulin (d) and side scatter in insulin-expressing beta cells (e). Results are representative of three experiments. Means ± s.e.m. **p<0.001.
Supplementary Figure 5 Transgene-induced beta cell stress results in disturbed insulin processing.
(a,b) Islets from B10k.Rag0/0, B10k.Rag0/0.insHEL, NODk.Rag0/0 and NODk.Rag0/0.insHEL mice were cultured in vitro in the presence of a high (25 mM) glucose concentration (n = 5/group) and assessed for insulin (a) and proinsulin (b) secretion by ELISA. (c,d) RNA-seq analysis was performed on the islets of B10k.Rag0/0, B10k.Rag0/0.insHEL, NODk.Rag0/0 and (pre-diabetic) NODk.Rag0/0.insHEL mice (n = 3/group). Expression is shown for Pcsk1 (prohormone convertase 1-3) (c) and Pcsk2 (prohormone convertase 2) (d). (e,f) Pancreas immunofluorescence with a polyclonal antibody to insulin, antibody to PC1 and PC3, and DAPI, with mice of the B10k.Rag0/0 and NODk.Rag0/0 backgrounds. Quantification is shown for islet raw fluorescence in the PC1-PC3 channel (n = 10, 16, 17, 16) (e), with representative sections (f). Scale bar, 100 μm. (g–i) Quantification of immunoblot analysis of islets from B10k, B10k.insHEL, NODk and NODk.insHEL mice for PC1-PC3 (g) and PC2 (h), with representative blots (n = 3/group) (i). Means ± s.e.m.: *P < 0.05, **P < 0.001, ***P < 0.0001.
Supplementary Figure 6 Glucose intolerance in insHEL transgenic mice.
(a,b) Blood glucose levels following a glucose tolerance test in B10k.Rag−/− (n = 15) and B10k.Rag−/−.insHEL (n = 17) mice at 12 (a) and 24 (b) weeks of age. (c,d) Blood glucose levels following a glucose tolerance test in (B10k × NODk).F1.Rag−/− (n = 11) and pre-diabetic (B10k × NODk)F1.Rag−/−.insHEL (n = 19) mice at 12 (c) and 24 (d) weeks of age. (e) Blood insulin levels following a glucose tolerance test in B10k (n = 5), B10k.insHEL (n = 4), NODk (n = 15) and NODk.insHEL (n = 9) mice at 12 weeks of age. Means ± s.e.m.: *P < 0.05, **P < 0.001, ***P < 0.0001.
Supplementary Figure 7 Sex hormones control susceptibility to islet stress and diabetes.
(a) Table of the incidence of diabetes at 26 weeks of age in female insHEL transgenic mice. (b) Representative electron microscopy images of beta cells from male and female NODk and NODk.insHEL mice at 12 weeks of age. Scale bar, 5 μm. (c) Images were used to assess the number of insulin granules per cellular cross-section (n = 3/group). (d,e) ERAI mice were crossed to NODk.Rag−/−.insHEL mice, and islets were analyzed by flow cytometry. Histograms show side scatter in insulin-expressing beta cells (d) and insulin (e). Results are representative of three experiments. (f–h) Fasting serum samples from male and female NODk and NODk.insHEL mice at 24 weeks of age were assessed by ELISA for insulin (n = 11, 11, 12, 7) (f), proinsulin (n = 11, 11, 12, 8) (g) and C-peptide (n = 11, 11, 9, 8) (h). (i,j) Pancreas immunofluorescence with a polyclonal antibody to insulin, antibody to PC1 and PC3, and DAPI, with female NODk.Rag−/− mice. Representative sections (scale bar, 100 μm) are shown (i), with quantification of islet raw fluorescence in the PC1-PC3 channel (n = 15, 25) (j). (k) Blood glucose levels in 12-week-old female NODk (n = 10) and NODk.insHEL (n = 9) mice following glucose tolerance test. (l) Average number of islets per pancreatic section in female NODk and NODk.insHEL mice at 28 weeks of age (n = 3 mice/group). (m) Incidence of diabetes in NODk insHEL transgenic male mice, with (n = 24) and without (n = 24) castration. Means ± s.e.m.: *P < 0.05, **P < 0.001, ***P < 0.0001.
Supplementary Figure 8 Expression of insHEL activates similar gene sets in B10 and NOD islets.
(a) Genes with significant expression changes between B10k.Rag−/− and NODk.Rag−/− islets were plotted for average expression. Outliers are annotated, Scg2 is not shown. (b,c) Cytoscape enrichment map for significant gene sets (FDR < 0.001) between B10k.Rag−/− islets and B10k.Rag−/−.insHEL islets (b) or NODk.Rag−/− islets and NODk.Rag−/−.insHEL islets (c). UPR and Xbp1 response gene sets are shown in yellow.
Supplementary Figure 9 Expression of insHEL induces similar transcriptional changes in qualitatively different B10 and NOD islets.
(a,b) Expression of genes significantly upregulated between B10k.Rag−/− islets and B10k.Rag−/−.insHEL islets (a) or between NODk.Rag−/− islets and NODk.Rag−/−.insHEL islets (b), with the average expression shown across all samples. Data represented are normalized to the expression in B10k.Rag−/− islets, with the average percentage and outliers annotated. H2k1 is not shown. (c,d) Expression of genes significantly downregulated between B10k.Rag−/− islets and B10k.Rag−/−.insHEL islets (c) or between NODk.Rag−/− islets and NODk.Rag−/−.insHEL islets (d), with the average expression shown across all samples. Data represented are normalized to the expression in B10k.Rag−/− islets, with the average percentage and outliers annotated.
Supplementary Figure 10 Molecular modeling of the effect of p.Ala27Thr and p.Glu125Asp mutations on Xrcc4 stability.
Simulation of the movements of the DNA ligase IV complex during 100-ns simulation. (a,b) Representative snapshots of the B10 allele (a) and NOD allele (b) for the DNA ligase IV complex extracted from the two trajectories at 0 ns, 60 ns, 80 ns and 100 ns. (c) Root-mean-square deviation of the BRCT2 domain of ligase 4 calculated with respect to the fixed position of BRCT1. Movements after the initial 70 ns of equilibrium were considered reliable. The black and gray lines represent ligase IV from the B10 and NOD alleles, respectively. Results are representative of four simulations.
Supplementary Figure 11 DNA ligase 4 hypomorph enhances susceptibility to diabetes.
B10k.insHEL mice were intercrossed with the ligase 4 hypomorph Tyr288Cys, and diabetes incidence was analyzed in B10 (n = 6), B10.Lig4Y228C/+ (n = 5), B10.insHEL (n = 7) and B10.Lig4Y228C/+.insHEL (n = 11) littermates. **P < 0.01.
Supplementary Figure 12 Transgene-induced beta cell stress results in disturbed insulin processing and glucose intolerance on the Glis3 heterozygous background.
(a–d) Fasting serum samples from wild-type (wt) B10 (n = 30), wt B10.Glis3+/– (n = 6), B10.insHEL (n = 51) and B10.Glis3+/–.insHEL (n = 7) mice at 10 weeks of age were assessed by ELISA for insulin (a), proinsulin (b), C-peptide (c) and proinsulin/insulin ratio (d). (e,f) Blood glucose levels in 12-week-old B10 (n = 6), B10.insHEL (n = 1), B10.Glis3+/– (n = 3) and (non-diabetic) B10.Glis3+/–.insHEL (n = 4) mice following glucose tolerance test (n = 28, 47, 9, 21) (e) or insulin tolerance test (n = 8, 17, 3, 13) (f). Means ± s.e.m.: *P < 0.05, **P < 0.001, ***P < 0.0001.
Supplementary Figure 13 Expression of GLIS3 and MANF in the islets of patients with T2D.
mRNA expression in human pancreatic islets from healthy individuals (n = 105) and individuals diagnosed with T2D (n = 14) was assessed through RNA-seq analysis. (a,b) Expression of GLIS3 (a) and MANF (b) in islets from healthy individuals as compared to islets from individuals with T2D. The median and interquartile range (box) are shown, with error bars indicating 1.5xIQR (interquartile range). Individual values are shown if beyond 1.5xIQR.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–13 and Supplementary Tables 1 and 2. (PDF 4390 kb)
Supplementary Data Set 1
Transcriptional analysis of the effect of insHEL on the B10 and NOD backgrounds. (XLSX 17127 kb)
Supplementary Data Set 2
Network analysis of the effect of insHEL on the B10 and NOD backgrounds. (XLSX 2954 kb)
Supplementary Data Set 3
Proteomics analysis of the effect of insHEL on the B10 and NOD backgrounds. (XLSX 153 kb)
Supplementary Data Set 4
Genomic variation analysis of islet-expressed genes on the B10 and NOD backgrounds. (XLSX 1842 kb)
Rights and permissions
About this article
Cite this article
Dooley, J., Tian, L., Schonefeldt, S. et al. Genetic predisposition for beta cell fragility underlies type 1 and type 2 diabetes. Nat Genet 48, 519–527 (2016). https://doi.org/10.1038/ng.3531
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.3531
This article is cited by
-
The emergence of obesity in type 1 diabetes
International Journal of Obesity (2024)
-
Pancreatic draining lymph nodes (PLNs) serve as a pathogenic hub contributing to the development of type 1 diabetes
Cell & Bioscience (2023)
-
Identification of the Genetic Association Between Type-2-Diabetes and Pancreatic Cancer
Biochemical Genetics (2023)
-
Study of the association between GLIS3 rs10758593 and type 2 diabetes mellitus in Egyptian population
Egyptian Journal of Medical Human Genetics (2022)
-
Functional characterization of T2D-associated SNP effects on baseline and ER stress-responsive β cell transcriptional activation
Nature Communications (2021)