Abstract
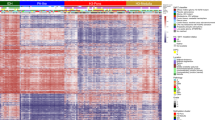
Pediatric high-grade glioma (HGG) is a devastating disease with a less than 20% survival rate 2 years after diagnosis1. We analyzed 127 pediatric HGGs, including diffuse intrinsic pontine gliomas (DIPGs) and non-brainstem HGGs (NBS-HGGs), by whole-genome, whole-exome and/or transcriptome sequencing. We identified recurrent somatic mutations in ACVR1 exclusively in DIPGs (32%), in addition to previously reported frequent somatic mutations in histone H3 genes, TP53 and ATRX, in both DIPGs and NBS-HGGs2,3,4,5. Structural variants generating fusion genes were found in 47% of DIPGs and NBS-HGGs, with recurrent fusions involving the neurotrophin receptor genes NTRK1, NTRK2 and NTRK3 in 40% of NBS-HGGs in infants. Mutations targeting receptor tyrosine kinase–RAS-PI3K signaling, histone modification or chromatin remodeling, and cell cycle regulation were found in 68%, 73% and 59% of pediatric HGGs, respectively, including in DIPGs and NBS-HGGs. This comprehensive analysis provides insights into the unique and shared pathways driving pediatric HGG within and outside the brainstem.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Gottardo, N.G. & Gajjar, A. Chemotherapy for malignant brain tumors of childhood. J. Child Neurol. 23, 1149–1159 (2008).
Pollack, I.F. et al. Age and TP53 mutation frequency in childhood malignant gliomas: results in a multi-institutional cohort. Cancer Res. 61, 7404–7407 (2001).
Schwartzentruber, J. et al. Driver mutations in histone H3.3 and chromatin remodelling genes in paediatric glioblastoma. Nature 482, 226–231 (2012).
Wu, G. et al. Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nat. Genet. 44, 251–253 (2012).
Khuong-Quang, D.A. et al. K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. Acta Neuropathol. 124, 439–447 (2012).
Faury, D. et al. Molecular profiling identifies prognostic subgroups of pediatric glioblastoma and shows increased YB-1 expression in tumors. J. Clin. Oncol. 25, 1196–1208 (2007).
Qu, H.Q. et al. Genome-wide profiling using single-nucleotide polymorphism arrays identifies novel chromosomal imbalances in pediatric glioblastomas. Neuro-oncol. 12, 153–163 (2010).
Paugh, B.S. et al. Genome-wide analyses identify recurrent amplifications of receptor tyrosine kinases and cell-cycle regulatory genes in diffuse intrinsic pontine glioma. J. Clin. Oncol. 29, 3999–4006 (2011).
Paugh, B.S. et al. Integrated molecular genetic profiling of pediatric high-grade gliomas reveals key differences with the adult disease. J. Clin. Oncol. 28, 3061–3068 (2010).
Schiffman, J.D. et al. Oncogenic BRAF mutation with CDKN2A inactivation is characteristic of a subset of pediatric malignant astrocytomas. Cancer Res. 70, 512–519 (2010).
Puget, S. et al. Mesenchymal transition and PDGFRA amplification/mutation are key distinct oncogenic events in pediatric diffuse intrinsic pontine gliomas. PLoS ONE 7, e30313 (2012).
Zarghooni, M. et al. Whole-genome profiling of pediatric diffuse intrinsic pontine gliomas highlights platelet-derived growth factor receptor α and poly (ADP-ribose) polymerase as potential therapeutic targets. J. Clin. Oncol. 28, 1337–1344 (2010).
Parsons, D.W. et al. An integrated genomic analysis of human glioblastoma multiforme. Science 321, 1807–1812 (2008).
Cancer Genome Atlas Research Network. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455, 1061–1068 (2008).
Bax, D.A. et al. A distinct spectrum of copy number aberrations in pediatric high-grade gliomas. Clin. Cancer Res. 16, 3368–3377 (2010).
Barrow, J. et al. Homozygous loss of ADAM3A revealed by genome-wide analysis of pediatric high-grade glioma and diffuse intrinsic pontine gliomas. Neuro-oncol. 13, 212–222 (2011).
Sturm, D. et al. Hotspot mutations in H3F3A and IDH1 define distinct epigenetic and biological subgroups of glioblastoma. Cancer Cell 22, 425–437 (2012).
Shore, E.M. & Kaplan, F.S. Role of altered signal transduction in heterotopic ossification and fibrodysplasia ossificans progressiva. Curr. Osteoporos. Rep. 9, 83–88 (2011).
Shore, E.M. et al. A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nat. Genet. 38, 525–527 (2006).
Chaikuad, A. et al. Structure of the bone morphogenetic protein receptor ALK2 and implications for fibrodysplasia ossificans progressiva. J. Biol. Chem. 287, 36990–36998 (2012).
Bagarova, J. et al. Constitutively active ALK2 receptor mutants require type II receptor cooperation. Mol. Cell. Biol. 33, 2413–2424 (2013).
Shen, Q. et al. The fibrodysplasia ossificans progressiva R206H ACVR1 mutation activates BMP-independent chondrogenesis and zebrafish embryo ventralization. J. Clin. Invest. 119, 3462–3472 (2009).
Cannon, J.E., Upton, P.D., Smith, J.C. & Morrell, N.W. Intersegmental vessel formation in zebrafish: requirement for VEGF but not BMP signalling revealed by selective and non-selective BMP antagonists. Br. J. Pharmacol. 161, 140–149 (2010).
Bond, A.M., Bhalala, O.G. & Kessler, J.A. The dynamic role of bone morphogenetic proteins in neural stem cell fate and maturation. Dev. Neurobiol. 72, 1068–1084 (2012).
Zhao, H., Ayrault, O., Zindy, F., Kim, J.H. & Roussel, M.F. Post-transcriptional down-regulation of Atoh1/Math1 by bone morphogenic proteins suppresses medulloblastoma development. Genes Dev. 22, 722–727 (2008).
Piccirillo, S.G. et al. Bone morphogenetic proteins inhibit the tumorigenic potential of human brain tumour–initiating cells. Nature 444, 761–765 (2006).
Lee, J. et al. Epigenetic-mediated dysfunction of the bone morphogenetic protein pathway inhibits differentiation of glioblastoma-initiating cells. Cancer Cell 13, 69–80 (2008).
Harel, L., Costa, B. & Fainzilber, M. On the death Trk. Dev. Neurobiol. 70, 298–303 (2010).
Thiele, C.J., Li, Z. & McKee, A.E. On Trk—the TrkB signal transduction pathway is an increasingly important target in cancer biology. Clin. Cancer Res. 15, 5962–5967 (2009).
Zhang, J. et al. Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nat. Genet. 45, 602–612 (2013).
Jones, D.T. et al. Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. Nat. Genet. 45, 927–932 (2013).
Frattini, V. et al. The integrated landscape of driver genomic alterations in glioblastoma. Nat. Genet. 45, 1141–1149 (2013).
Lannon, C.L. & Sorensen, P.H. ETV6-NTRK3: a chimeric protein tyrosine kinase with transformation activity in multiple cell lineages. Semin. Cancer Biol. 15, 215–223 (2005).
Li, Z. et al. ETV6-NTRK3 fusion oncogene initiates breast cancer from committed mammary progenitors via activation of AP1 complex. Cancer Cell 12, 542–558 (2007).
Eguchi, M. et al. Fusion of ETV6 to neurotrophin-3 receptor TRKC in acute myeloid leukemia with t(12;15)(p13;q25). Blood 93, 1355–1363 (1999).
Butti, M.G. et al. A sequence analysis of the genomic regions involved in the rearrangements between TPM3 and NTRK1 genes producing TRK oncogenes in papillary thyroid carcinomas. Genomics 28, 15–24 (1995).
Cetinbas, N. et al. Mutation of the salt bridge–forming residues in the ETV6 SAM domain interface blocks ETV6-NTRK3 induced cellular transformation. J. Biol. Chem. 288, 27940–27950 (2013).
Bax, D.A. et al. EGFRvIII deletion mutations in pediatric high-grade glioma and response to targeted therapy in pediatric glioma cell lines. Clin. Cancer Res. 15, 5753–5761 (2009).
Li, G. et al. Expression of epidermal growth factor variant III (EGFRvIII) in pediatric diffuse intrinsic pontine gliomas. J. Neurooncol. 108, 395–402 (2012).
Fontebasso, A.M. et al. Mutations in SETD2 and genes affecting histone H3K36 methylation target hemispheric high-grade gliomas. Acta Neuropathol. 125, 659–669 (2013).
Chan, K.M. et al. The histone H3.3K27M mutation in pediatric glioma reprograms H3K27 methylation and gene expression. Genes Dev. 27, 985–990 (2013).
Lewis, P.W. et al. Inhibition of PRC2 activity by a gain-of-function H3 H3 mutation found in pediatric glioblastoma. Science 340, 857–861 (2013).
Venneti, S. et al. Evaluation of histone 3 lysine 27 trimethylation (H3K27me3) and enhancer of zest 2 (EZH2) in pediatric glial and glioneuronal tumors shows decreased H3K27me3 in H3F3A K27M mutant glioblastomas. Brain Pathol. 23, 558–564 (2013).
Bender, S. et al. Reduced H3K27me3 and DNA hypomethylation are major drivers of gene expression in K27M mutant pediatric high-grade gliomas. Cancer Cell 24, 660–672 (2013).
Füllgrabe, J., Kavanagh, E. & Joseph, B. Histone onco-modifications. Oncogene 30, 3391–3403 (2011).
Zhang, J. et al. The genetic basis of early T-cell precursor acute lymphoblastic leukaemia. Nature 481, 157–163 (2012).
Robinson, G. et al. Novel mutations target distinct subgroups of medulloblastoma. Nature 488, 43–48 (2012).
Dubuc, A.M. et al. Aberrant patterns of H3K4 and H3K27 histone lysine methylation occur across subgroups in medulloblastoma. Acta Neuropathol. 125, 373–384 (2013).
Jones, D.T. et al. Dissecting the genomic complexity underlying medulloblastoma. Nature 488, 100–105 (2012).
Pugh, T.J. et al. Medulloblastoma exome sequencing uncovers subtype-specific somatic mutations. Nature 488, 106–110 (2012).
Nie, Z. et al. c-Myc is a universal amplifier of expressed genes in lymphocytes and embryonic stem cells. Cell 151, 68–79 (2012).
Lin, C.Y. et al. Transcriptional amplification in tumor cells with elevated c-Myc. Cell 151, 56–67 (2012).
Stephens, P.J. et al. Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell 144, 27–40 (2011).
Killela, P.J. et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc. Natl. Acad. Sci. USA 110, 6021–6026 (2013).
Kleiblova, P. et al. Gain-of-function mutations of PPM1D/Wip1 impair the p53-dependent G1 checkpoint. J. Cell Biol. 201, 511–521 (2013).
Torchia, E.C., Boyd, K., Rehg, J.E., Qu, C. & Baker, S.J. EWS/FLI-1 induces rapid onset of myeloid/erythroid leukemia in mice. Mol. Cell. Biol. 27, 7918–7934 (2007).
Zhang, J. et al. A novel retinoblastoma therapy from genomic and epigenetic analyses. Nature 481, 329–334 (2012).
Wang, J. et al. CREST maps somatic structural variation in cancer genomes with base-pair resolution. Nat. Methods 8, 652–654 (2011).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Zhang, J. et al. SNPdetector: a software tool for sensitive and accurate SNP detection. PLOS Comput. Biol. 1, e53 (2005).
Gordon, D., Abajian, C. & Green, P. Consed: a graphical tool for sequence finishing. Genome Res. 8, 195–202 (1998).
Rousseeuw, P. Least Median Squares Regression. J. Am. Stat. Assoc. 79, 871–880 (1984).
Holmfeldt, L. et al. The genomic landscape of hypodiploid acute lymphoblastic leukemia. Nat. Genet. 45, 242–252 (2013).
Szymczak, A.L. et al. Correction of multi-gene deficiency in vivo using a single 'self-cleaving' 2A peptide–based retroviral vector. Nat. Biotechnol. 22, 589–594 (2004).
Kawauchi, D. et al. A mouse model of the most aggressive subgroup of human medulloblastoma. Cancer Cell 21, 168–180 (2012).
Persons, D.A. et al. Enforced expression of the GATA-2 transcription factor blocks normal hematopoiesis. Blood 93, 488–499 (1999).
Bajenaru, M.L. et al. Astrocyte-specific inactivation of the neurofibromatosis 1 gene (NF1) is insufficient for astrocytoma formation. Mol. Cell. Biol. 22, 5100–5113 (2002).
Jonkers, J. et al. Synergistic tumor suppressor activity of BRCA2 and p53 in a conditional mouse model for breast cancer. Nat. Genet. 29, 418–425 (2001).
Fraser, M.M. et al. Pten loss causes hypertrophy and increased proliferation of astrocytes in vivo. Cancer Res. 64, 7773–7779 (2004).
Endersby, R., Zhu, X., Hay, N., Ellison, D.W. & Baker, S.J. Nonredundant functions for Akt isoforms in astrocyte growth and gliomagenesis in an orthotopic transplantation model. Cancer Res. 71, 4106–4116 (2011).
Korbel, J.O. & Campbell, P.J. Criteria for inference of chromothripsis in cancer genomes. Cell 152, 1226–1236 (2013).
Acknowledgements
We thank the St. Jude Children's Research Hospital Tissue Resource Facility and B. Gordon, M. Johnson, S. Brown and C. Calabrese in the St. Jude Small Animal Imaging Core for expert assistance with intracranial implantations. We thank E. Shore and A. Culbert (University of Pennsylvania) for helpful advice with antibody selection. This work was supported by the St. Jude Children's Research Hospital–Washington University Pediatric Cancer Genome Project, by the American Lebanese and Syrian Associated Charities (ALSAC) of St. Jude Children's Research Hospital, by grants from the US National Institutes of Health (P01 CA096832 to S.J.B., Jinghui Zhang and D.W.E. and R01 CA135554 to S.J.B.), by the Cure Starts Now Foundation and the Smile for Sophie Forever Foundation, and by Tyler's Treehouse and Musicians Against Childhood Cancer.
Author information
Authors and Affiliations
Consortia
Contributions
S.J.B., Jinghui Zhang, A.K.D., B.S.P., J.E., L.D., E.R.M., R.K.W., M.R.T., J.R.D. and D.W.E. designed experiments or supervised research. A.G., A.B., C.W., F.A.B. and C.J. provided samples or clinical data. G.W., A.K.D., B.S.P., S.L.R., B.J., Y.L., X.Z., C.Q., X.C., Junyuan Zhang, J.E., M.E., X.M., C.L., P.N., E.H., M.R., S.P., T.L., A.O.-T., R.H., R.K., M.P., P.G., J.B., L.W., H.L.M., K.B., B.V., D.Y., J.C.R., K.O., R.S.F., L.L.F., L.D., E.R.M., R.K.W., M.R.T., J.R.D., D.W.E., Jinghui Zhang and S.J.B. performed experiments, analyzed data or prepared tables and figures. D.W.E. completed all pathological evaluations. S.J.B., Jinghui Zhang, G.W. and A.K.D. wrote the manuscript with contributions from D.W.E., J.R.D. and M.R.T.
Corresponding authors
Ethics declarations
Competing interests
The author declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Note and Supplementary Figures 1–10 (PDF 5585 kb)
Supplementary Tables
Supplementary Tables 1–13 (XLSX 3927 kb)
Rights and permissions
About this article
Cite this article
the St. Jude Children's Research Hospital–Washington University Pediatric Cancer Genome Project. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet 46, 444–450 (2014). https://doi.org/10.1038/ng.2938
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.2938
This article is cited by
-
A new genomic framework to categorize pediatric acute myeloid leukemia
Nature Genetics (2024)
-
PRMT5 inhibition shows in vitro efficacy against H3K27M-altered diffuse midline glioma, but does not extend survival in vivo
Scientific Reports (2024)
-
Clinicohistoradiological and surgical outcome in diffuse midline glioma
Child's Nervous System (2024)
-
Pediatric glioma histone H3.3 K27M/G34R mutations drive abnormalities in PML nuclear bodies
Genome Biology (2023)
-
BMP signaling in cancer stemness and differentiation
Cell Regeneration (2023)