Abstract
Angiosarcoma is an aggressive malignancy that arises spontaneously or secondarily to ionizing radiation or chronic lymphoedema1. Previous work has identified aberrant angiogenesis, including occasional somatic mutations in angiogenesis signaling genes, as a key driver of angiosarcoma1. Here we employed whole-genome, whole-exome and targeted sequencing to study the somatic changes underpinning primary and secondary angiosarcoma. We identified recurrent mutations in two genes, PTPRB and PLCG1, which are intimately linked to angiogenesis. The endothelial phosphatase PTPRB, a negative regulator of vascular growth factor tyrosine kinases, harbored predominantly truncating mutations in 10 of 39 tumors (26%). PLCG1, a signal transducer of tyrosine kinases, encoded a recurrent, likely activating p.Arg707Gln missense variant in 3 of 34 cases (9%). Overall, 15 of 39 tumors (38%) harbored at least one driver mutation in angiogenesis signaling genes. Our findings inform and reinforce current therapeutic efforts to target angiogenesis signaling in angiosarcoma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Young, R.J., Brown, N.J., Reed, M.W., Hughes, D. & Woll, P.J. Angiosarcoma. Lancet Oncol. 11, 983–991 (2010).
Fachinger, G., Deutsch, U. & Risau, W. Functional interaction of vascular endothelial-protein-tyrosine phosphatase with the angiopoietin receptor Tie-2. Oncogene 18, 5948–5953 (1999).
Winderlich, M. et al. VE-PTP controls blood vessel development by balancing Tie-2 activity. J. Cell Biol. 185, 657–671 (2009).
Bamford, S. et al. The COSMIC (Catalogue of Somatic Mutations in Cancer) database and website. Br. J. Cancer 91, 355–358 (2004).
Guo, T. et al. Consistent MYC and FLT4 gene amplification in radiation-induced angiosarcoma but not in other radiation-associated atypical vascular lesions. Genes Chromosom. Cancer 50, 25–33 (2011).
Dominguez, M.G. et al. Vascular endothelial tyrosine phosphatase (VE-PTP)-null mice undergo vasculogenesis but die embryonically because of defects in angiogenesis. Proc. Natl. Acad. Sci. USA 104, 3243–3248 (2007).
Bäumer, S. et al. Vascular endothelial cell–specific phosphotyrosine phosphatase (VE-PTP) activity is required for blood vessel development. Blood 107, 4754–4762 (2006).
Broermann, A. et al. Dissociation of VE-PTP from VE-cadherin is required for leukocyte extravasation and for VEGF-induced vascular permeability in vivo. J. Exp. Med. 208, 2393–2401 (2011).
Carra, S. et al. Ve-ptp modulates vascular integrity by promoting adherens junction maturation. PLoS ONE 7, e51245 (2012).
Hayashi, M. et al. VE-PTP regulates VEGFR2 activity in stalk cells to establish endothelial cell polarity and lumen formation. Nat. Commun. 4, 1672 (2013).
Li, Z. et al. Embryonic stem cell tumor model reveals role of vascular endothelial receptor tyrosine phosphatase in regulating Tie2 pathway in tumor angiogenesis. Proc. Natl. Acad. Sci. USA 106, 22399–22404 (2009).
Mellberg, S. et al. Transcriptional profiling reveals a critical role for tyrosine phosphatase VE-PTP in regulation of VEGFR2 activity and endothelial cell morphogenesis. FASEB J. 23, 1490–1502 (2009).
Nawroth, R. et al. VE-PTP and VE-cadherin ectodomains interact to facilitate regulation of phosphorylation and cell contacts. EMBO J. 21, 4885–4895 (2002).
Nottebaum, A.F. et al. VE-PTP maintains the endothelial barrier via plakoglobin and becomes dissociated from VE-cadherin by leukocytes and by VEGF. J. Exp. Med. 205, 2929–2945 (2008).
Saharinen, P., Eklund, L., Pulkki, K., Bono, P. & Alitalo, K. VEGF and angiopoietin signaling in tumor angiogenesis and metastasis. Trends Mol. Med. 17, 347–362 (2011).
Zhou, Q. et al. A hypermorphic missense mutation in PLCG2, encoding phospholipase Cγ2, causes a dominantly inherited autoinflammatory disease with immunodeficiency. Am. J. Hum. Genet. 91, 713–720 (2012).
Everett, K.L. et al. Characterization of phospholipase Cγ enzymes with gain-of-function mutations. J. Biol. Chem. 284, 23083–23093 (2009).
Ombrello, M.J. et al. Cold urticaria, immunodeficiency, and autoimmunity related to PLCG2 deletions. N. Engl. J. Med. 366, 330–338 (2012).
Bunney, T.D. et al. Structural and functional integration of the PLCγ interaction domains critical for regulatory mechanisms and signaling deregulation. Structure 20, 2062–2075 (2012).
Covassin, L.D. et al. A genetic screen for vascular mutants in zebrafish reveals dynamic roles for Vegf/Plcg1 signaling during artery development. Dev. Biol. 329, 212–226 (2009).
Lawson, N.D., Mugford, J.W., Diamond, B.A. & Weinstein, B.M. Phospholipase Cγ-1 is required downstream of vascular endothelial growth factor during arterial development. Genes Dev. 17, 1346–1351 (2003).
Liao, H.J. et al. Absence of erythrogenesis and vasculogenesis in Plcg1-deficient mice. J. Biol. Chem. 277, 9335–9341 (2002).
Antonescu, C.R. et al. KDR activating mutations in human angiosarcomas are sensitive to specific kinase inhibitors. Cancer Res. 69, 7175–7179 (2009).
Behjati, S. et al. Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nat. Genet. 45, 1479–1482 (2013).
Tarpey, P.S. et al. Frequent mutation of the major cartilage collagen gene COL2A1 in chondrosarcoma. Nat. Genet. 45, 923–926 (2013).
Li, H. & Durbin, R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics 26, 589–595 (2010).
Ye, K., Schulz, M.H., Long, Q., Apweiler, R. & Ning, Z. Pindel: a pattern growth approach to detect break points of large deletions and medium sized insertions from paired-end short reads. Bioinformatics 25, 2865–2871 (2009).
Trapnell, C., Pachter, L. & Salzberg, S.L. TopHat: discovering splice junctions with RNA-Seq. Bioinformatics 25, 1105–1111 (2009).
Trapnell, C. et al. Transcript assembly and quantification by RNA-Seq reveals unannotated transcripts and isoform switching during cell differentiation. Nat. Biotechnol. 28, 511–515 (2010).
Van Loo, P. et al. Allele-specific copy number analysis of tumors. Proc. Natl. Acad. Sci. USA 107, 16910–16915 (2010).
Greenman, C., Wooster, R., Futreal, P.A., Stratton, M.R. & Easton, D.F. Statistical analysis of pathogenicity of somatic mutations in cancer. Genetics 173, 2187–2198 (2006).
Acknowledgements
We thank M. Taylor and R. Leek for sample preparation. We are grateful to the patients for participating in the research and to the clinicians and support staff involved in their care from the Oxford University Hospitals NHS Trust, the University of Texas MD Anderson Cancer Center Sarcoma Program and the London Sarcoma Service. This work was supported by funding from the Wellcome Trust (grant reference 077012/Z/05/Z). The material was obtained from the Royal National Orthopaedic Hospital Musculoskeletal Research Program and Biobank and from the Oxford Radcliffe Biobank. Support was provided to A.M.F. by the National Institute for Health Research, the University College London Hospital Biomedical Research Centre and the Cancer Research UK University College London Experimental Cancer Medicine Centre. Support was provided to A.H. by Cancer Research UK, the Oxford Biomedical Research Centre and the Breast Cancer Research Foundation. P.J.C. is personally funded through a Wellcome Trust Senior Clinical Research Fellowship (grant reference WT088340MA). P.V.L. is a postdoctoral researcher of the Research Foundation–Flanders (FWO). H.K.M.V. is supported by the Norwegian Radium Hospital's Foundation. S.B. is funded through the Wellcome Trust PhD Programme for Clinicians. P.A.F. is supported by the Cancer Prevention Research Institute of Texas and the Welch Foundation.
Author information
Authors and Affiliations
Contributions
S.B. and P.S.T. performed analyses of sequencing data. H.S. performed in vitro experiments. P.V.L. performed copy number analysis. D.C.W. and I.M. performed statistical analyses. S.L.C. performed rearrangement analysis. G.G., N.P., M.R., H.K.M.V. and E.P. contributed to data analysis. H.K., T.D.B. and M.K. contributed structural analyses. C.H., O.R.J., L.M., H.M., A.P., J.T., L.L., Y.C. and C.G. coordinated sample processing and technical investigations. S.M. coordinated sample acquisition. A.B., J.W.T., S.S., X.S. and J.Z. coordinated informatics analyses. B.K., D.H., D.B., M.P., G.S., I.R., R.T., M.F.A., A.M.F., C.B., V.R., K.E.T., D.I., A.J.L., G.A.A.S. and A.H. provided samples and clinical data. P.J.C., M.R.S., A.H., P.A.F., U.M. and A.M.F. directed the research. M.R.S., P.J.C., S.B. and P.S.T. wrote the manuscript, with contributions from A.H., A.M.F. and P.A.F.
Corresponding author
Ethics declarations
Competing interests
C.B. is an employee of Pfizer.
Integrated supplementary information
Supplementary Figure 1 Genome-wide structural rearrangements.
CIRCOS plots representing rearrangement in the three genomes studied at the whole-genome level. Colors represent rearrangement class: orange, inversion type (tail to tail); blue, inversion type (head to head); green, deletion type; black, tandem duplication type; purple, interchromosomal.
Supplementary Figure 2 Mutation frequency in tumor suppressor genes.
Publicly available catalogs of somatic mutations in cancers (n = 4,073) were analyzed for the frequency of 2 mutations (point mutations or LOH) in established tumor suppressor genes. For every gene, we selected all those samples in which the gene had a truncating mutation (nonsense, essential splice site or out-of-frame indel) and quantified the frequency of a second mutation, truncating, LOH, missense or in-frame indel, in the gene. Error bars represent the 95% confidence intervals of the total fraction of two-hit samples (using a Chi-square approximation, as implemented in the function prop.test in R (version 3.0.1).
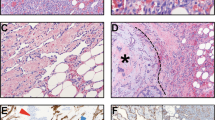
Supplementary Figure 3 Assessment of PTPRB silencing.
(A) PTPRB levels after silencing demonstrating ~80% reduction in PTPRP transcript levels. (B) Following PTPRB silencing, VE-cadherin expression is greatly reduced. (C) PTPRB silencing increases the phosphorylation levels of VEGFR2.
Supplementary Figure 4 Activation of PLCγ enzymes by loss of autoinhibition.
(A) Diagram showing the domains in PLCγ. The regulatory region (comprising the spPH, nSH2, cSH2 and SH3 domains; amino acids 465–952 in PLCγ1) is inserted in a loop that connects two halves (X and Y boxes) of the catalytic domain (purple). The cSH2 domain (red), involved in autoinhibition, is in direct contact with the catalytic domain. Disruption of the cSH2 domain by deletion or point mutation can cause constitutive PLCγ activation. The R707Q alteration in the cSH2 domain is indicated in blue. Residue numbering is per human PLCγ1. (B) Structure of the PLCγ1 cSH2 domain (PDB 4EY0). The interface involved in autoinhibition and residue R707 are shown. (C) Possible impact of R707Q alterations on the PLCγ1 cSH2 domain. R707 is involved in interactions with several residues (left, doted lines) that are likely to be important for domain stability and conformational changes. These interactions are disrupted when R707 is replaced by glutamine (right).
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–4 and Supplementary Table 6 (PDF 3604 kb)
Supplementary Table 1
Clinical features of cases included in this study with likely driver mutations. (XLSX 72 kb)
Supplementary Table 2
Coding mutations in 11 angiosarcomas subjected to whole-genome or whole-exome sequencing. (XLSX 88 kb)
Supplementary Table 3
Substitutions and indels identified in three angiosarcoma genomes. (XLSX 1137 kb)
Supplementary Table 4
Rearrangements identified in three angiosarcoma genomes. (XLSX 105 kb)
Supplementary Table 5
Amplification and homozygous deletions identified in three angiosarcoma genomes. (XLSX 17122 kb)
Supplementary Table 7
Cancer genes screened by targeted sequencing. (XLSX 69 kb)
Source data
Rights and permissions
About this article
Cite this article
Behjati, S., Tarpey, P., Sheldon, H. et al. Recurrent PTPRB and PLCG1 mutations in angiosarcoma. Nat Genet 46, 376–379 (2014). https://doi.org/10.1038/ng.2921
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.2921
This article is cited by
-
Radiation-induced angiosarcoma of the breast: retrospective analysis at a regional treatment centre
Breast Cancer (2024)
-
Spatial transcriptomics reveal topological immune landscapes of Asian head and neck angiosarcoma
Communications Biology (2023)
-
Phospholipase Cγ1 (PLCG1) overexpression is associated with tumor growth and poor survival in IDH wild-type lower-grade gliomas in adult patients
Laboratory Investigation (2022)
-
Impaired Fanconi anemia pathway causes DNA hypomethylation in human angiosarcomas
Human Cell (2022)
-
Update from the 5th Edition of the World Health Organization Classification of Head and Neck Tumors: Soft Tissue Tumors
Head and Neck Pathology (2022)