Abstract
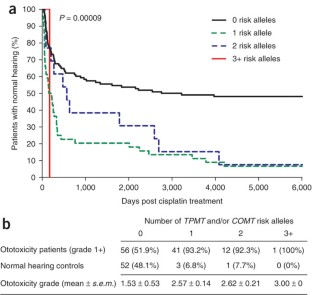
Cisplatin is a widely used and effective chemotherapeutic agent, although its use is restricted by the high incidence of irreversible ototoxicity associated with it1. In children, cisplatin ototoxicity is a serious and pervasive problem, affecting more than 60% of those receiving cisplatin2,3,4,5 and compromising language and cognitive development. Candidate gene studies have previously reported associations of cisplatin ototoxicity with genetic variants in the genes encoding glutathione S-transferases and megalin6,7,8. We report association analyses for 220 drug-metabolism genes in genetic susceptibility to cisplatin-induced hearing loss in children. We genotyped 1,949 SNPs in these candidate genes in an initial cohort of 54 children treated in pediatric oncology units, with replication in a second cohort of 112 children recruited through a national surveillance network for adverse drug reactions in Canada. We identified genetic variants in TPMT (rs12201199, P value = 0.00022, OR = 17.0, 95% CI 2.3–125.9) and COMT (rs9332377, P value = 0.00018, OR = 5.5, 95% CI 1.9–15.9) associated with cisplatin-induced hearing loss in children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Change history
21 March 2013
In the version of this article initially published, the units for treatment duration in Table 1 were incorrectly given as weeks rather than months. This error has been corrected in the HTML and PDF versions of the article.
References
Brock, P. & Bellman, S. Ototoxicity of cisplatinum. Br. J. Cancer 63, 159–160 (1991).
Li, Y., Womer, R.B. & Silber, J.H. Predicting cisplatin ototoxicity in children: the influence of age and the cumulative dose. Eur. J. Cancer 40, 2445–2451 (2004).
Coradini, P.P., Cigana, L., Selistre, S.G., Rosito, L.S. & Brunetto, A.L. Ototoxicity from cisplatin therapy in childhood cancer. J. Pediatr. Hematol. Oncol. 29, 355–360 (2007).
Knight, K.R., Kraemer, D.F. & Neuwelt, E.A. Ototoxicity in children receiving platinum chemotherapy: underestimating a commonly occurring toxicity that may influence academic and social development. J. Clin. Oncol. 23, 8588–8596 (2005).
Kushner, B.H., Budnick, A., Kramer, K., Modak, S. & Cheung, N.K. Ototoxicity from high-dose use of platinum compounds in patients with neuroblastoma. Cancer 107, 417–422 (2006).
Oldenburg, J., Kraggerud, S.M., Cvancarova, M., Lothe, R.A. & Fossa, S.D. Cisplatin-induced long-term hearing impairment is associated with specific glutathione S-transferase genotypes in testicular cancer survivors. J. Clin. Oncol. 25, 708–714 (2007).
Peters, U. et al. Glutathione S-transferase genetic polymorphisms and individual sensitivity to the ototoxic effect of cisplatin. Anti-Cancer Drugs. Anticancer Drugs 11, 639–643 (2000).
Riedemann, L. et al. Megalin genetic polymorphisms and individual sensitivity to the ototoxic effect of cisplatin. Pharmacogenomics J. 8, 23–28 (2008).
Blakley, B.W., Gupta, A.K., Myers, S.F. & Schwan, S. Risk factors for ototoxicity due to cisplatin. Arch. Otolaryngol. Head Neck Surg. 120, 541–546 (1994).
Bess, F.H., Dodd-Murphy, J. & Parker, R.A. Children with minimal sensorineural hearing loss: prevalence, educational performance, and functional status. Ear Hear. 19, 339–354 (1998).
Ekborn, A. et al. Cisplatin-induced hearing loss: influence of the mode of drug administration in the guinea pig. Hear. Res. 140, 38–44 (2000).
Hirschhorn, J.N. & Daly, M.J. Genome-wide association studies for common diseases and complex traits. Nat. Rev. Genet. 6, 95–108 (2005).
Ujiie, S., Sasaki, T., Mizugaki, M., Ishikawa, M. & Hiratsuka, M. Functional characterization of 23 allelic variants of thiopurine S-methyltransferase gene (TPMT*2 - *24). Pharmacogenet. Genomics 18, 887–893 (2008).
Diatchenko, L. et al. Genetic basis for individual variations in pain perception and the development of a chronic pain condition. Hum. Mol. Genet. 14, 135–143 (2005).
Nackley, A.G. et al. Human catechol-O-methyltransferase haplotypes modulate protein expression by altering mRNA secondary structure. Science 314, 1930–1933 (2006).
Price, A.L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909 (2006).
Visscher, H. et al. Application of principal component analysis to pharmacogenomic studies in Canada. Pharmacogenomics J. advance online publication, doi:10.1038/tpj.2009.36 (4 August 2009).
The International HapMap Consortium. A haplotype map of the human genome. Nature 437, 1299–1320 (2005).
Shord, S.S., Thompson, D.M., Krempl, G.A. & Hanigan, M.H. Effect of concurrent medications on cisplatin-induced nephrotoxicity in patients with head and neck cancer. Anticancer Drugs 17, 207–215 (2006).
Krynetski, E.Y., Krynetskaia, N.F., Yanishevski, Y. & Evans, W.E. Methylation of mercaptopurine, thioguanine, and their nucleotide metabolites by heterologously expressed human thiopurine S-methyltransferase. Mol. Pharmacol. 47, 1141–1147 (1995).
Yates, C.R. et al. Molecular diagnosis of thiopurine S-methyltransferase deficiency: genetic basis for azathioprine and mercaptopurine intolerance. Ann. Intern. Med. 126, 608–614 (1997).
Relling, M.V. et al. Mercaptopurine therapy intolerance and heterozygosity at the thiopurine S-methyltransferase gene locus. J. Natl. Cancer Inst. 91, 2001–2008 (1999).
Weinshilboum, R.M. Pharmacogenomics: catechol O-methyltransferase to thiopurine S-methyltransferase. Cell. Mol. Neurobiol. 26, 539–561 (2006).
Weinshilboum, R.M. & Sladek, S.L. Mercaptopurine pharmacogenetics: monogenic inheritance of erythrocyte thiopurine methyltransferase activity. Am. J. Hum. Genet. 32, 651–662 (1980).
Ochoa, B., Bobadilla, N., Arrellin, G. & Herrera, L.A. S-Adenosyl-L-methionine increases serum BUN and creatinine in cisplatin-treated mice. Arch. Med. Res. 40, 54–58 (2009).
Ahmed, Z.M. et al. Mutations of LRTOMT, a fusion gene with alternative reading frames, cause nonsyndromic deafness in humans. Nat. Genet. 40, 1335–1340 (2008).
Du, X. et al. A catechol-O-methyltransferase that is essential for auditory function in mice and humans. Proc. Natl. Acad. Sci. USA 105, 14609–14614 (2008).
Nelson, M.R. et al. Genome-wide approaches to identify pharmacogenetic contributions to adverse drug reactions. Pharmacogenomics J. 9, 23–33 (2008).
Link, E. et al. SLCO1B1 variants and statin-induced myopathy—a genomewide study. N. Engl. J. Med. 359, 789–799 (2008).
Ross, C.J. et al. Genotypic approaches to therapy in children: a national active surveillance network (GATC) to study the pharmacogenomics of severe adverse drug reactions in children. Ann. NY Acad. Sci. 1110, 177–192 (2007).
Carlson, C.S. et al. Selecting a maximally informative set of single-nucleotide polymorphisms for association analyses using linkage disequilibrium. Am. J. Hum. Genet. 74, 106–120 (2004).
Guo, S.W. & Thompson, E.A. Performing the exact test of Hardy-Weinberg proportion for multiple alleles. Biometrics 48, 361–372 (1992).
Gao, X., Starmer, J. & Martin, E.R. A multiple testing correction method for genetic association studies using correlated single nucleotide polymorphisms. Genet. Epidemiol. 32, 361–369 (2008).
Acknowledgements
We especially want to acknowledge the study participants and their families for their participation in the Canadian Pharmacogenomics Network for Drug Safety (CPNDS) network; this work could not have been done without your help and support. We also want to acknowledge the support of the CPNDS active ADR surveillance consortium, as well as S. Langlois and B. Casey (Supplementary Note). The study was funded by Genome Canada, and additional funding was also provided by Genome British Columbia, Child and Family Research Institute, University of British Columbia Faculty of Pharmaceutical Sciences, Canadian Institutes of Health Research, Canada Foundation for Innovation, Canada Gene Cure Foundation, Canadian Society of Clinical Pharmacology, BC Clinical Genomics Network, C17 Research Network and Childhood Cancer Foundation–Candlelighters Canada, Michael Smith Foundation for Health Research, Health Canada, Pfizer, Eli Lilly, Merck Frosst and Janssen-Ortho. This work was funded as part of the peer-reviewed Genome Canada Applied Health Research Program; the pharmaceutical industry partners had no formal or informal role in this program of research.
Author information
Authors and Affiliations
Consortia
Contributions
B.C.C., S.R.R., M.J.R., P.C.R. and members of the CPNDS consortium recruited subject cohorts. B.B., B.C.C. and S.R.R. phenotyped subject cohorts. C.J.D.R., H.K.-E., H.V., A.M.K.B. and M.S.P. designed and performed genotyping studies. C.J.D.R., H.K.-E., H.V., A.B., Y.F.-Z. and M.-P.D. analyzed genotyping data. B.C.C. and M.R.H. planned and coordinated the study. All authors contributed to the final version of the manuscript.
Corresponding author
Additional information
A full list of members is provided in the Supplementary Note.
Supplementary information
Supplementary Text and Figures
Supplementary Note, Supplementary Figures 1 and 2 and Supplementary Tables 2–5. (PDF 782 kb)
Supplementary Table 1
Allele frequencies and results of the case-control tests of association (XLS 803 kb)
Rights and permissions
About this article
Cite this article
Ross, C., Katzov-Eckert, H., Dubé, MP. et al. Genetic variants in TPMT and COMT are associated with hearing loss in children receiving cisplatin chemotherapy. Nat Genet 41, 1345–1349 (2009). https://doi.org/10.1038/ng.478
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.478
This article is cited by
-
Mechanisms in cochlear hair cell mechano-electrical transduction for acquisition of sound frequency and intensity
Cellular and Molecular Life Sciences (2021)
-
GSTM1 null and GSTT1 null: predictors of cisplatin-caused acute ototoxicity measured by DPOAEs
Journal of Molecular Medicine (2020)
-
2-Hydroxypropyl-β-cyclodextrin Ototoxicity in Adult Rats: Rapid Onset and Massive Destruction of Both Inner and Outer Hair Cells Above a Critical Dose
Neurotoxicity Research (2020)
-
Genetic variation of cisplatin-induced ototoxicity in non-cranial-irradiated pediatric patients using a candidate gene approach: The International PanCareLIFE Study
The Pharmacogenomics Journal (2020)



