Abstract
For several decades scientists have speculated that the key to understanding age-related neurodegenerative disorders may be found in the unusual biology of the prion diseases. Recently, owing largely to the advent of new disease models, this hypothesis has gained experimental momentum. In a remarkable variety of diseases, specific proteins have been found to misfold and aggregate into seeds that structurally corrupt like proteins, causing them to aggregate and form pathogenic assemblies ranging from small oligomers to large masses of amyloid. Proteinaceous seeds can therefore serve as self-propagating agents for the instigation and progression of disease. Alzheimer’s disease and other cerebral proteopathies seem to arise from the de novo misfolding and sustained corruption of endogenous proteins, whereas prion diseases can also be infectious in origin. However, the outcome in all cases is the functional compromise of the nervous system, because the aggregated proteins gain a toxic function and/or lose their normal function. As a unifying pathogenic principle, the prion paradigm suggests broadly relevant therapeutic directions for a large class of currently intractable diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Uversky, V. N. & Dunker, A. K. The case for intrinsically disordered proteins playing contributory roles in molecular recognition without a stable 3D structure. F1000 Biol. Rep. 5, 1 (2013)
Malinovska, L., Kroschwald, S. & Alberti, S. Protein disorder, prion propensities, and self-organizing macromolecular collectives. Biochim. Biophys. Acta 1834, 918–931 (2013)
Balch, W. E., Morimoto, R. I., Dillin, A. & Kelly, J. W. Adapting proteostasis for disease intervention. Science 319, 916–919 (2008)
Hartl, F. U., Bracher, A. & Hayer-Hartl, M. Molecular chaperones in protein folding and proteostasis. Nature 475, 324–332 (2011)
Thal, D. R., Rub, U., Orantes, M. & Braak, H. Phases of amyloid-β-deposition in the human brain and its relevance for the development of AD. Neurology 58, 1791–1800 (2002)
Braak, H. & Braak, E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 82, 239–259 (1991)
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211 (2003)
Brettschneider, J. et al. Stages of pTDP-43 pathology in amyotrophic lateral sclerosis. Ann. Neurol. http://dx.doi.org/10.1002/ana.23937 (2013)
Prusiner, S. B. Prions. Proc. Natl Acad. Sci. USA 95, 13363–13383 (1998)
Collinge, J. Prion diseases of humans and animals: their causes and molecular basis. Annu. Rev. Neurosci. 24, 519–550 (2001)
Aguzzi, A. & Calella, A. M. Prions: protein aggregation and infectious diseases. Physiol. Rev. 89, 1105–1152 (2009)
Caughey, B., Baron, G. S., Chesebro, B. & Jeffrey, M. Getting a grip on prions: oligomers, amyloids, and pathological membrane interactions. Annu. Rev. Biochem. 78, 177–204 (2009)
Head, M. W. & Ironside, J. W. Review: Creutzfeldt–Jakob disease: prion protein type, disease phenotype and agent strain. Neuropathol. Appl. Neurobiol. 38, 296–310 (2012)
DeArmond, S. J. & Prusiner, S. B. Etiology and pathogenesis of prion diseases. Am. J. Pathol. 146, 785–811 (1995)
Wadsworth, J. D. & Collinge, J. Molecular pathology of human prion disease. Acta Neuropathol. 121, 69–77 (2011)
Tanaka, M., Collins, S. R., Toyama, B. H. & Weissman, J. S. The physical basis of how prion conformations determine strain phenotypes. Nature 442, 585–589 (2006)
Collinge, J. & Clarke, A. R. A general model of prion strains and their pathogenicity. Science 318, 930–936 (2007)
Colby, D. W. & Prusiner, S. B. Prions. Cold Spring Harb. Perspect. Biol. 3, a006833 (2011)
Silveira, J. R. et al. The most infectious prion protein particles. Nature 437, 257–261 (2005)
Sandberg, M. K., Al-Doujaily, H., Sharps, B., Clarke, A. R. & Collinge, J. Prion propagation and toxicity in vivo occur in two distinct mechanistic phases. Nature 470, 540–542 (2011)
Jarrett, J. T. & Lansbury, P. T., Jr Seeding “one-dimensional crystallization” of amyloid: a pathogenic mechanism in Alzheimer's disease and scrapie? Cell 73, 1055–1058 (1993)One of the first papers to suggest a common pathogenic mechanism between prion diseases and Alzheimer's disease based on in vitro protein aggregation studies.
Sipe, J. D. et al. Amyloid fibril protein nomenclature: 2012 recommendations from the Nomenclature Committee of the International Society of Amyloidosis. Amyloid 19, 167–170 (2012)
Buxbaum, J. N. & Linke, R. P. A molecular history of the amyloidoses. J. Mol. Biol. 421, 142–159 (2012)
Blancas-Mejía, L. M. & Ramirez-Alvarado, M. Systemic amyloidoses. Annu. Rev. Biochem. 82, 745–774 (2013)
Dobson, C. M. Protein misfolding, evolution and disease. Trends Biochem. Sci. 24, 329–332 (1999) An early paper suggesting that all proteins have the intrinsic potential to form amyloid under suitable conditions.
Chiti, F. & Dobson, C. M. Protein misfolding, functional amyloid, and human disease. Annu. Rev. Biochem. 75, 333–366 (2006)
Maji, S. K. et al. Functional amyloids as natural storage of peptide hormones in pituitary secretory granules. Science 325, 328–332 (2009)
Greenwald, J. & Riek, R. Biology of amyloid: structure, function, and regulation. Structure 18, 1244–1260 (2010)
Hou, F. et al. MAVS forms functional prion-like aggregates to activate and propagate antiviral innate immune response. Cell 146, 448–461 (2011)
Blanco, L. P., Evans, M. L., Smith, D. R., Badtke, M. P. & Chapman, M. R. Diversity, biogenesis and function of microbial amyloids. Trends Microbiol. 20, 66–73 (2012)
Wickner, R. B. et al. Amyloids and yeast prion biology. Biochemistry 52, 1514–1527 (2013)
Eisenberg, D. & Jucker, M. The amyloid state of proteins in human diseases. Cell 148, 1188–1203 (2012)
Mucke, L. & Selkoe, D. J. Neurotoxicity of amyloid β-protein: synaptic and network dysfunction. Cold Spring Harbor Perspect. Med. 2, a006338 (2012)
Tycko, R. & Wickner, R. B. Molecular structures of amyloid and prion fibrils: consensus versus controversy. Acc. Chem. Res. 46, 1487–1496 (2013)
Liu, C. et al. Out-of-register β-sheets suggest a pathway to toxic amyloid aggregates. Proc. Natl Acad. Sci. USA 109, 20913–20918 (2012)
Laganowsky, A. et al. Atomic view of a toxic amyloid small oligomer. Science 335, 1228–1231 (2012)
Jan, A. et al. Aβ42 neurotoxicity is mediated by ongoing nucleated polymerization process rather than by discrete Aβ42 species. J. Biol. Chem. 286, 8585–8596 (2011)
Petkova, A. T. et al. Self-propagating, molecular-level polymorphism in Alzheimer's β-amyloid fibrils. Science 307, 262–265 (2005)This study demonstrates that the morphology and toxicity of synthetic β-amyloid fibrils are linked to variations in the molecular structure of the protein, and that these properties can be propagated to subsequent generations of fibrils in vitro by a seeding mechanism.
Toyama, B. H. & Weissman, J. S. Amyloid structure: conformational diversity and consequences. Annu. Rev. Biochem. 80, 557–585 (2011)
Westermark, G. T. & Westermark, P. Prion-like aggregates: infectious agents in human disease. Trends Mol. Med. 16, 501–507 (2010)An overview of the prion-like properties of systemic amyloids.
Yan, J. et al. Cross-seeding and cross-competition in mouse apolipoprotein A-II amyloid fibrils and protein A amyloid fibrils. Am. J. Pathol. 171, 172–180 (2007)
Xing, Y. et al. Transmission of mouse senile amyloidosis. Lab. Invest. 81, 493–499 (2001)
Zhang, B. et al. Fecal transmission of AA amyloidosis in the cheetah contributes to high incidence of disease. Proc. Natl Acad. Sci. USA 105, 7263–7268 (2008)
Korenaga, T. et al. Transmission of amyloidosis in offspring of mice with AApoAII amyloidosis. Am. J. Pathol. 168, 898–906 (2006)
De Strooper, B. Proteases and proteolysis in Alzheimer disease: a multifactorial view on the disease process. Physiol. Rev. 90, 465–494 (2010)
Holtzman, D. M., Morris, J. C. & Goate, A. M. Alzheimer's disease: the challenge of the second century. Sci. Transl. Med. 3, 77s71 (2011)
Bateman, R. J. et al. Clinical and biomarker changes in dominantly inherited Alzheimer's disease. N. Engl. J. Med. 367, 795–804 (2012)
Villemagne, V. L. et al. Amyloid β deposition, neurodegeneration, and cognitive decline in sporadic Alzheimer's disease: a prospective cohort study. Lancet Neurol. 12, 357–367 (2013)
Baker, H. F., Ridley, R. M., Duchen, L. W., Crow, T. J. & Bruton, C. J. Evidence for the experimental transmission of cerebral β-amyloidosis to primates. Int. J. Exp. Pathol. 74, 441–454 (1993)Evidence that senile plaques in the brains of nonhuman primates are inducible by the intracerebral injection of Alzheimer's brain homogenates.
Jucker, M. The benefits and limitations of animal models for translational research in neurodegenerative diseases. Nature Med. 16, 1210–1214 (2010)
Kane, M. D. et al. Evidence for seeding of β-amyloid by intracerebral infusion of Alzheimer brain extracts in β-amyloid precursor protein-transgenic mice. J. Neurosci. 20, 3606–3611 (2000)
Meyer-Luehmann, M. et al. Exogenous induction of cerebral β-amyloidogenesis is governed by agent and host. Science 313, 1781–1784 (2006)The first conclusive demonstration that an aggregated form of Aβ is the β-amyloid-inducing agent in donor brain extracts, and that the transmission of cerebral β-amyloidosis is dependent on the nature of both the seed and the host.
Morales, R., Duran-Aniotz, C., Castilla, J., Estrada, L. D. & Soto, C. De novo induction of amyloid-β deposition in vivo. Mol. Psychiatry 17, 1347–1353 (2012)
Rosen, R. F. et al. Exogenous seeding of cerebral β-amyloid deposition in βAPP-transgenic rats. J. Neurochem. 120, 660–666 (2012)
Langer, F. et al. Soluble amyloid-β seeds are potent inducers of cerebral β-amyloid deposition. J. Neurosci. 31, 14488–14495 (2011)
Stöhr, J. et al. Purified and synthetic Alzheimer's amyloid beta (amyloid-β) prions. Proc. Natl Acad. Sci. USA 109, 11025–11030 (2012)Demonstration that Aβ deposition can be seeded in the brain by synthetic Aβ seeds.
Legname, G. et al. Synthetic mammalian prions. Science 305, 673–676 (2004)
Wang, F., Wang, X., Yuan, C. G. & Ma, J. Generating a prion with bacterially expressed recombinant prion protein. Science 327, 1132–1135 (2010)
LeVine III, H. & Walker, L. C. Molecular polymorphism of amyloid-β in Alzheimer's disease. Neurobiol. Aging 31, 542–548 (2010)
Heilbronner, G. et al. Seeded strain-like transmission of β-amyloid morphotypes in APP transgenic mice. EMBO Rep. http://dx.doi.org/10.1038/embor.2013.137 (3 September 2013)
Jucker, M. & Walker, L. C. Pathogenic protein seeding in Alzheimer disease and other neurodegenerative disorders. Ann. Neurol. 70, 532–540 (2011)
Hamaguchi, T. et al. The presence of amyloid-β seeds, and not age per se, is critical to the initiation of amyloid-β deposition in the brain. Acta Neuropathol. 123, 31–37 (2012)
Eisele, Y. S. et al. Peripherally applied amyloid-β-containing inoculates induce cerebral β-amyloidosis. Science 330, 980–982 (2010)Demonstration that cerebral Aβ deposition can be induced by the introduction of Aβ seeds into the peritoneal cavity (a site outside the brain).
Lee, V. M., Goedert, M. & Trojanowski, J. Q. Neurodegenerative tauopathies. Annu. Rev. Neurosci. 24, 1121–1159 (2001)
Goldstein, L. E. et al. Chronic traumatic encephalopathy in blast-exposed military veterans and a blast neurotrauma mouse model. Science Transl. Med. 4, 134ra160 (2012)
Clavaguera, F. et al. Transmission and spreading of tauopathy in transgenic mouse brain. Nature Cell Biol. 11, 909–913 (2009)The first report that tau lesions can be instigated in tau-transgenic mice by the intracerebral infusion of brain extracts containing aggregated tau.
Lasagna-Reeves, C. A. et al. Alzheimer brain-derived tau oligomers propagate pathology from endogenous tau. Scientific Rep. 2, 700 (2012)
Clavaguera, F. et al. Brain homogenates from human tauopathies induce tau inclusions in mouse brain. Proc. Natl Acad. Sci. USA 110, 9535–9540 (2013)
Guo, J. L. & Lee, V. M. Neurofibrillary tangle-like tau pathology induced by synthetic tau fibrils in primary neurons over-expressing mutant tau. FEBS Lett. 587, 717–723 (2013)
Iba, M. et al. Synthetic tau fibrils mediate transmission of neurofibrillary tangles in a transgenic mouse model of Alzheimer’s-like tauopathy. J. Neurosci. 33, 1024–1037 (2013)
Goedert, M., Spillantini, M. G., Del Tredici, K. & Braak, H. 100 years of Lewy pathology. Nature Rev. Neurology 9, 13–24 (2013)
Kordower, J. H., Chu, Y., Hauser, R. A., Freeman, T. B. & Olanow, C. W. Lewy body-like pathology in long-term embryonic nigral transplants in Parkinson's disease. Nature Med. 14, 504–506 (2008)
Li, J. Y. et al. Lewy bodies in grafted neurons in subjects with Parkinson's disease suggest host-to-graft disease propagation. Nature Med. 14, 501–503 (2008)These two reports (refs 72, 73) suggest that endogenous α-synuclein seeds in the brains of humans with Parkinson's disease can induce the aggregation of α-synuclein in grafted neurons.
Hansen, C. et al. α-Synuclein propagates from mouse brain to grafted dopaminergic neurons and seeds aggregation in cultured human cells. J. Clin. Invest. 121, 715–725 (2011)
Kordower, J. H. et al. Transfer of host-derived α synuclein to grafted dopaminergic neurons in rat. Neurobiol. Dis. 43, 552–557 (2011)
Volpicelli-Daley, L. A. et al. Exogenous α-synuclein fibrils induce Lewy body pathology leading to synaptic dysfunction and neuron death. Neuron 72, 57–71 (2011)
Desplats, P. et al. Inclusion formation and neuronal cell death through neuron-to-neuron transmission of α-synuclein. Proc. Natl Acad. Sci. USA 106, 13010–13015 (2009)
Mougenot, A. L. et al. Prion-like acceleration of a synucleinopathy in a transgenic mouse model. Neurobiol. Aging 33, 2225–2228 (2012)
Luk, K. C. et al. Intracerebral inoculation of pathological α-synuclein initiates a rapidly progressive neurodegenerative α-synucleinopathy in mice. J. Exp. Med. 209, 975–986 (2012)These two studies (refs 78, 79) first showed that α-synuclein lesions can be induced in α-synuclein-transgenic mice by the intracerebral inoculation of brain extracts rich in aggregated α-synuclein.
Luk, K. C. et al. Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science 338, 949–953 (2012)Describes the instigation of α-synucleinopathy by the intracerebral injection of synthetic α-synuclein fibrils into non-transgenic mice.
Masuda-Suzukake, M. et al. Prion-like spreading of pathological α-synuclein in brain. Brain 136, 1178–1138 (2013)
Guo, J. L. et al. Distinct α-synuclein strains differentially promote tau inclusions in neurons. Cell 154, 103–117 (2013)This study describes the strain-dependent induction of tau aggregation by aggregated α-synuclein in vitro and in vivo.
Van Langenhove, T., van der Zee, J. & Van Broeckhoven, C. The molecular basis of the frontotemporal lobar degeneration-amyotrophic lateral sclerosis spectrum. Ann. Med. 44, 817–828 (2012)
Rademakers, R., Neumann, M. & Mackenzie, I. R. Advances in understanding the molecular basis of frontotemporal dementia. Nature Rev. Neurol. 8, 423–434 (2012)
Cruts, M., Gijselinck, I., Van Langenhove, T., van der Zee, J. & Van Broeckhoven, C. Current insights into the C9orf72 repeat expansion diseases of the FTLD/ALS spectrum. Trends Neurosci. 36, 450–459 (2013)
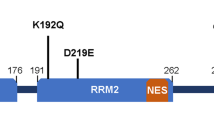
Kim, H. J. et al. Mutations in prion-like domains in hnRNPA2B1 and hnRNPA1 cause multisystem proteinopathy and ALS. Nature 495, 467–473 (2013)
King, O. D., Gitler, A. D. & Shorter, J. The tip of the iceberg: RNA-binding proteins with prion-like domains in neurodegenerative disease. Brain Res. 1462, 61–80 (2012)
Li, Y. R., King, O. D., Shorter, J. & Gitler, A. D. Stress granules as crucibles of ALS pathogenesis. J. Cell Biol. 201, 361–372 (2013)
Olzscha, H. et al. Amyloid-like aggregates sequester numerous metastable proteins with essential cellular functions. Cell 144, 67–78 (2011)
Furukawa, Y., Kaneko, K., Watanabe, S., Yamanaka, K. & Nukina, N. A seeding reaction recapitulates intracellular formation of Sarkosyl-insoluble transactivation response element (TAR) DNA-binding protein-43 inclusions. J. Biol. Chem. 286, 18664–18672 (2011)
Münch, C., O'Brien, J. & Bertolotti, A. Prion-like propagation of mutant superoxide dismutase-1 misfolding in neuronal cells. Proc. Natl Acad. Sci. USA 108, 3548–3553 (2011)
Grad, L. I. et al. Intermolecular transmission of superoxide dismutase 1 misfolding in living cells. Proc. Natl Acad. Sci. USA 108, 16398–16403 (2011)
Polymenidou, M. & Cleveland, D. W. The seeds of neurodegeneration: prion-like spreading in ALS. Cell 147, 498–508 (2011)
Hollstein, M., Sidransky, D., Vogelstein, B. & Harris, C. C. p53 mutations in human cancers. Science 253, 49–53 (1991)
Xu, J. et al. Gain of function of mutant p53 by coaggregation with multiple tumor suppressors. Nature Chem. Biol. 7, 285–295 (2011)
Ano Bom, A. P. et al. Mutant p53 aggregates into prion-like amyloid oligomers and fibrils: implications for cancer. J. Biol. Chem. 287, 28152–28162 (2012)These two studies (refs 95, 96) demonstrate the aggregation and prion-like characteristics of p53, a protein that normally regulates the cell-cycle and acts to inhibit tumour formation.
Sigurdson, C. J. & Aguzzi, A. Chronic wasting disease. Biochim. Biophys. Acta 1772, 610–618 (2007)
Hoinville, L. J. A review of the epidemiology of scrapie in sheep. Rev. Sci. Tech. 15, 827–852 (1996)
Collinge, J. et al. Kuru in the 21st century—an acquired human prion disease with very long incubation periods. Lancet 367, 2068–2074 (2006)
Brown, P. et al. Iatrogenic Creutzfeldt–Jakob disease, final assessment. Emerg. Infect. Dis. 18, 901–907 (2012)
Irwin, D. J. et al. Evaluation of potential infectivity of Alzheimer and Parkinson disease proteins in recipients of cadaver-derived human growth hormone. JAMA Neurol. 70, 462–468 (2013)
Johnson, S. M., Connelly, S., Fearns, C., Powers, E. T. & Kelly, J. W. The transthyretin amyloidoses: from delineating the molecular mechanism of aggregation linked to pathology to a regulatory-agency-approved drug. J. Mol. Biol. 421, 185–203 (2012)
Sievers, S. A. et al. Structure-based design of non-natural amino-acid inhibitors of amyloid fibril formation. Nature 475, 96–100 (2011)
Saper, C. B., Wainer, B. H. & German, D. C. Axonal and transneuronal transport in the transmission of neurological disease: potential role in system degenerations, including Alzheimer's disease. Neuroscience 23, 389–398 (1987)
Ravits, J. M. & La Spada, A. R. ALS motor phenotype heterogeneity, focality, and spread: deconstructing motor neuron degeneration. Neurology 73, 805–811 (2009)
Eidelberg, D. & Surmeier, D. J. Brain networks in Huntington disease. J. Clin. Invest. 121, 484–492 (2011)
Zhou, J., Gennatas, E. D., Kramer, J. H., Miller, B. L. & Seeley, W. W. Predicting regional neurodegeneration from the healthy brain functional connectome. Neuron 73, 1216–1227 (2012)
Raj, A., Kuceyeski, A. & Weiner, M. A network diffusion model of disease progression in dementia. Neuron 73, 1204–1215 (2012)
Gardner, R. C. et al. Intrinsic connectivity network disruption in progressive supranuclear palsy. Ann. Neurol. 73, 603–616 (2013)
Bero, A. W. et al. Neuronal activity regulates the regional vulnerability to amyloid-β deposition. Nature Neurosci. 14, 750–756 (2011)
Dolev, I. et al. Spike bursts increase amyloid-β 40/42 ratio by inducing a presenilin-1 conformational change. Nature Neurosci. 16, 587–595 (2013)
Pooler, A. M., Phillips, E. C., Lau, D. H., Noble, W. & Hanger, D. P. Physiological release of endogenous tau is stimulated by neuronal activity. EMBO Rep. 14, 389–394 (2013)
Bae, E. J. et al. Antibody-aided clearance of extracellular α-synuclein prevents cell-to-cell aggregate transmission. J. Neurosci. 32, 13454–13469 (2012)
Polymenidou, M. & Cleveland, D. W. Prion-like spread of protein aggregates in neurodegeneration. J. Exp. Med. 209, 889–893 (2012)
Holmes, B. B. & Diamond, M. I. Cellular mechanisms of protein aggregate propagation. Curr. Opin. Neurol. 25, 721–726 (2012)
Wu, J. W. et al. Small misfolded Tau species are internalized via bulk endocytosis and anterogradely and retrogradely transported in neurons. J. Biol. Chem. 288, 1856–1870 (2013)
Aguzzi, A. & Rajendran, L. The transcellular spread of cytosolic amyloids, prions, and prionoids. Neuron 64, 1856–790 (2009)
Nath, S. et al. Spreading of neurodegenerative pathology via neuron-to-neuron transmission of β-amyloid. J. Neurosci. 32, 8767–8777 (2012)
Kfoury, N., Holmes, B. B., Jiang, H., Holtzman, D. M. & Diamond, M. I. Trans-cellular propagation of Tau aggregation by fibrillar species. J. Biol. Chem. 287, 19440–19451 (2012)
Freundt, E. C. et al. Neuron-to-neuron transmission of α-synuclein fibrils through axonal transport. Ann. Neurol. 72, 517–524 (2012)
Ren, P. H. et al. Cytoplasmic penetration and persistent infection of mammalian cells by polyglutamine aggregates. Nature Cell Biol. 11, 219–225 (2009)
Selkoe, D. J. Resolving controversies on the path to Alzheimer's therapeutics. Nature Med. 17, 1060–1065 (2011)
Gajdusek, D. C. Spontaneous generation of infectious nucleating amyloids in the transmissible and nontransmissible cerebral amyloidoses. Mol. Neurobiol. 8, 1–13 (1994)
Lee, J., Culyba, E. K., Powers, E. T. & Kelly, J. W. Amyloid-β forms fibrils by nucleated conformational conversion of oligomers. Nature Chem. Biol. 7, 602–609 (2011)
Knowles, T. P. & Buehler, M. J. Nanomechanics of functional and pathological amyloid materials. Nature Nanotechnol. 6, 469–479 (2011)
Acknowledgements
We thank D. Eisenberg, H. LeVine, A. Aguzzi, J. Collinge, R. Rosen, Y. Eisele, A. Mehta, M. Gearing, J. Manson, M. Neumann, and the members of our laboratories for critical discussions and comments. The help of H. Braak with Fig. 1, and the help of S. Eberle with the manuscript and figures is gratefully acknowledged. This work was supported by grants from the Competence Network on Degenerative Dementias (BMBF-01GI0705), ALZKULT (BMBF-031A198A), NGFN2 (BMBF-01GS08131), and anonymous foundations (to M.J.), and by National Institutes of Health grants R21AG040589, P51RR165, P51OD11132, and the CART Foundation (to L.C.W.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
M.J. and L.C.W. contributed to the writing of the review
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Jucker, M., Walker, L. Self-propagation of pathogenic protein aggregates in neurodegenerative diseases. Nature 501, 45–51 (2013). https://doi.org/10.1038/nature12481
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature12481
This article is cited by
-
Data-driven modelling of neurodegenerative disease progression: thinking outside the black box
Nature Reviews Neuroscience (2024)
-
Iatrogenic Alzheimer’s disease in recipients of cadaveric pituitary-derived growth hormone
Nature Medicine (2024)
-
Cryo-EM structures of lipidic fibrils of amyloid-β (1-40)
Nature Communications (2024)
-
Neuropathogenesis-on-chips for neurodegenerative diseases
Nature Communications (2024)
-
Endoplasmic reticulum stress and the unfolded protein response: emerging regulators in progression of traumatic brain injury
Cell Death & Disease (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.