Abstract
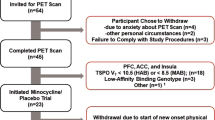
Basic studies exploring the importance of the cyclic adenosine monophosphate (cAMP) cascade in major depressive disorder (MDD) have noted that the cAMP cascade is downregulated in MDD and upregulated by antidepressant treatment. We investigated cAMP cascade activity by using 11C-(R)-rolipram to image phosphodiesterase-4 (PDE4) in unmedicated MDD patients and after ~8 weeks of treatment with a selective serotonin reuptake inhibitor (SSRI). 11C-(R)-rolipram positron emission tomographic (PET) scans were performed in 44 unmedicated patients during a major depressive episode and 35 healthy controls. Twenty-three of the 44 patients had a follow-up 11C-(R)-rolipram PET scan ~8 weeks after treatment with an SSRI. Patients were moderately depressed (Montgomery–Åsberg Depression Rating Scale=30±6) and about half were treatment naïve. 11C-(R)-rolipram binding was measured using arterial sampling to correct for individual differences in radioligand metabolism. We found in unmedicated MDD patients widespread, ~20% reductions in 11C-(R)-rolipram binding compared with controls (P=0.001). SSRI treatment significantly increased rolipram binding (12%, P<0.001), with significantly greater increases observed in older patients (P<0.001). Rolipram binding did not correlate with severity of baseline symptoms, and increased rolipram binding during treatment did not correlate with symptom improvement. In brief, consistent with the results of basic studies, PDE4 was decreased in unmedicated MDD patients and increased after SSRI treatment. The lack of correlation between PDE4 binding and depressive symptoms could reflect the heterogeneity of the disease and/or the heterogeneity of the target, given that PDE4 has four subtypes. These results suggest that PDE4 inhibitors, which increase cAMP cascade activity, may have antidepressant effects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Dwivedi Y, Rizavi HS, Conley RR, Roberts RC, Tamminga CA, Pandey GN . Altered gene expression of brain-derived neurotrophic factor and receptor tyrosine kinase B in postmortem brain of suicide subjects. Arch Gen Psychiatry 2003; 60: 804–815.
Dowlatshahi D, MacQueen GM, Wang JF, Young LT . Increased temporal cortex CREB concentrations and antidepressant treatment in major depression. Lancet 1998; 352: 1754–1755.
Reiach JS, Li PP, Warsh JJ, Kish SJ, Young LT . Reduced adenylyl cyclase immunolabeling and activity in postmortem temporal cortex of depressed suicide victims. J Affect Disord 1999; 56: 141–151.
Duman RS . Synaptic plasticity and mood disorders. Mol Psychiatry 2002; 7 (Suppl 1): S29–S34.
Houslay MD, Sullivan M, Bolger GB . The multienzyme PDE4 cyclic adenosine monophosphate-specific phosphodiesterase family: intracellular targeting, regulation, and selective inhibition by compounds exerting anti-inflammatory and antidepressant actions. In: August TJ, Murad F, Anders MW, Coyle JT (eds). Advances in Pharmacology, vol. 44. Academic Press: London, UK, 1998, pp 225–342.
Hoffmann R, Wilkinson IR, McCallum JF, Engels P, Houslay MD . cAMP-specific phosphodiesterase HSPDE4D3 mutants which mimic activation and changes in rolipram inhibition triggered by protein kinase A phosphorylation of Ser-54: generation of a molecular model. Biochem J 1998; 333 (Part 1): 139–149.
Itoh T, Abe K, Hong J, Inoue O, Pike VW, Innis RB et al. Effects of cAMP-dependent protein kinase activator and inhibitor on in vivo rolipram binding to phosphodiesterase 4 in conscious rats. Synapse 2010; 64: 172–176.
Fujita M, Hines CS, Zoghbi SS, Mallinger AG, Dickstein LP, Liow JS et al. Downregulation of brain phosphodiesterase type IV measured with 11C-(R-rolipram positron emission tomography in major depressive disorder. Biol Psychiatry 2012; 72: 548–554.
First MB, Spitzer RL, Williams JBW, MG . Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). Biometrics Research Department, New York State Psychiatric Institute: New York, NY, USA, 2001.
Montgomery SA, Asberg M . A new depression scale designed to be sensitive to change. Br J Psychiatry 1979; 134: 382–389.
Hamilton M . A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23: 56–62.
Hamilton M . The assessment of anxiety states by rating. Br J Med Psychol 1959; 32: 50–55.
Innis RB, Cunningham VJ, Delforge J, Fujita M, Gjedde A, Gunn RN et al. Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J Cereb Blood Flow Metab 2007; 27: 1533–1539.
Logan J, Fowler JS, Volkow ND, Wolf AP, Dewey SL, Schlyer DJ et al. Graphical analysis of reversible radioligand binding from time-activity measurements applied to [N-11C-methyl]-(-)cocaine PET studies in human subjects. J Cereb Blood Flow Metab 1990; 10: 740–747.
Müller-Gätner HW, Links JM, Prince JL, Bryan RN, McVeigh E, Leal JP et al. Measurement of radiotracer concentration in brain gray matter using positron emission tomography: MRI-based correction for partial volume effects. J Cereb Blood Flow Metab 1992; 12: 571–583.
Koolschijn PC, van Haren NE, Lensvelt-Mulders GJ, Hulshoff Pol HE, Kahn RS . Brain volume abnormalities in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Hum Brain Mapp 2009; 30: 3719–3735.
Dwivedi Y, Conley RR, Roberts RC, Tamminga CA, Pandey GN . [3H]cAMP binding sites and protein kinase a activity in the prefrontal cortex of suicide victims. Am J Psychiatry 2002; 159: 66–73.
Dwivedi Y, Rao JS, Rizavi HS, Kotowski J, Conley RR, Roberts RC et al. Abnormal expression and functional characteristics of cyclic adenosine monophosphate response element binding protein in postmortem brain of suicide subjects. Arch Gen Psychiatry 2003; 60: 273–282.
Yamada S, Yamamoto M, Ozawa H, Riederer P, Saito T . Reduced phosphorylation of cyclic AMP-responsive element binding protein in the postmortem orbitofrontal cortex of patients with major depressive disorder. J Neural Transm 2003; 110: 671–680.
Lowther S, Katona CL, Crompton MR, Horton RW . Brain [3H]cAMP binding sites are unaltered in depressed suicides, but decreased by antidepressants. Brain Res 1997; 758: 223–228.
Itoh T, Abe K, Zoghbi SS, Inoue O, Hong J, Imaizumi M et al. Positron emission tomographic measurement of the in vivo affinity of 11C-(R)-rolipram and the density of its target, phosphodiesterase-4, in brain of conscious and anesthetized rats. J Nucl Med 2009; 50: 749–756.
Hansen RT 3rd, Zhang HT . Phosphodiesterase-4 modulation as a potential therapeutic for cognitive loss in pathological and non-pathological aging: possibilities and pitfalls. Curr Pharm Des 2015; 21: 291–302.
Sierksma AS, van den Hove DL, Pfau F, Philippens M, Bruno O, Fedele E et al. Improvement of spatial memory function in APPswe/PS1dE9 mice after chronic inhibition of phosphodiesterase type 4D. Neuropharmacology 2014; 77: 120–130.
Millar JK, Pickard BS, Mackie S, James R, Christie S, Buchanan SR et al. DISC1 and PDE4B are interacting genetic factors in schizophrenia that regulate cAMP signaling. Science 2005; 310: 1187–1191.
Hikida T, Gamo NJ, Sawa A . DISC1 as a therapeutic target for mental illnesses. Expert Opin Ther Targets 2012; 16: 1151–1160.
Zhang HT, Huang Y, Masood A, Stolinski LR, Li Y, Zhang L et al. Anxiogenic-like behavioral phenotype of mice deficient in phosphodiesterase 4B (PDE4B). Neuropsychopharmacology 2008; 33: 1611–1623.
Numata S, Iga J, Nakataki M, Tayoshi S, Taniguchi K, Sumitani S et al. Gene expression and association analyses of the phosphodiesterase 4B (PDE4B) gene in major depressive disorder in the Japanese population. Am J Med Genet B 2009; 150B: 527–534.
Zhang HT, Huang Y, Jin SL, Frith SA, Suvarna N, Conti M et al. Antidepressant-like profile and reduced sensitivity to rolipram in mice deficient in the PDE4D phosphodiesterase enzyme. Neuropsychopharmacology 2002; 27: 587–595.
Li YF, Cheng YF, Huang Y, Conti M, Wilson SP, O'Donnell JM et al. Phosphodiesterase-4D knock-out and RNA interference-mediated knock-down enhance memory and increase hippocampal neurogenesis via increased cAMP signaling. J Neurosci 2011; 31: 172–183.
Zeller E, Stief HJ, Pflug B, Sastre-y-Hernandez M . Results of a phase II study of the antidepressant effect of rolipram. Pharmacopsychiatry 1984; 17: 188–190.
Laux G, Becker T, Kuhne G, Lesch KP, Riederer P, Beckmann H . Clinical and biochemical effects of the selective phosphodiesterase inhibitor rolipram in depressed inpatients controlled by determination of plasma level. Pharmacopsychiatry 1988; 21: 378–379.
Bobon D, Breulet M, Gerard-Vandenhove MA, Guiot-Goffioul F, Plomteux G, Sastre-y-Hernandez M et al. Is phosphodiesterase inhibition a new mechanism of antidepressant action? A double blind double-dummy study between rolipram and desipramine in hospitalized major and/or endogenous depressives. Eur Arch Psychiatr Neurol Sci 1988; 238: 2–6.
Bertolino A, Crippa D, di Dio S, Fichte K, Musmeci G, Porro V et al. Rolipram versus imipramine in inpatients with major, 'minor' or atypical depressive disorder: a double-blind double-dummy study aimed at testing a novel therapeutic approach. Int Clin Psychopharmacol 1988; 3: 245–253.
Scott AI, Perini AF, Shering PA, Whalley LJ . In-patient major depression: is rolipram as effective as amitriptyline? Eur J Clin Pharmacol 1991; 40: 127–129.
Robichaud A, Stamatiou PB, Jin SL, Lachance N, MacDonald D, Laliberte F et al. Deletion of phosphodiesterase 4D in mice shortens alpha(2)-adrenoceptor-mediated anesthesia, a behavioral correlate of emesis. J Clin Invest 2002; 110: 1045–1052.
Acknowledgements
This study was funded by the Intramural Research Program of the National Institute Mental Health, NIH: projects ZIAMH002852, ZIAMH002793 and ZIAMH002927 under clinical protocol NCT00369798 (06-M-0215). We thank the staff of the Experimental Therapeutics and Pathophysiology Branch for recruitment and clinical care of patients with MDD; the staff of Molecular Imaging Branch for recruitment of healthy control subjects and for performing the PET scans; the staff of NIH’s PET Department (Chief: Peter Herscovitch, MD) for scanning; Wayne C Drevets, MD, for guidance on the design and execution of the study, Dave Luckenbaugh, MA, for assistance for statistical analysis, Ioline Henter, MA, for editorial assistance and PMOD Technologies (Zurich, Switzerland) for providing its image analysis and modeling software.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Zarate is listed as a coinventor on a patent for the use of ketamine and its metabolites in major depression. Dr Zarate has assigned his rights in the patent to the US government but will share a percentage of any royalties that may be received by the government. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Molecular Psychiatry website
Supplementary information
PowerPoint slides
Rights and permissions
About this article
Cite this article
Fujita, M., Richards, E., Niciu, M. et al. cAMP signaling in brain is decreased in unmedicated depressed patients and increased by treatment with a selective serotonin reuptake inhibitor. Mol Psychiatry 22, 754–759 (2017). https://doi.org/10.1038/mp.2016.171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mp.2016.171
This article is cited by
-
Application of positron emission tomography in psychiatry—methodological developments and future directions
Translational Psychiatry (2022)
-
A novel peripheral biomarker for depression and antidepressant response
Molecular Psychiatry (2022)
-
Potential depression and antidepressant-response biomarkers in human lymphoblast cell lines from treatment-responsive and treatment-resistant subjects: roles of SSRIs and omega-3 polyunsaturated fatty acids
Molecular Psychiatry (2021)
-
Astrocytes with TDP-43 inclusions exhibit reduced noradrenergic cAMP and Ca2+ signaling and dysregulated cell metabolism
Scientific Reports (2020)
-
Astroglial Mechanisms of Ketamine Action Include Reduced Mobility of Kir4.1-Carrying Vesicles
Neurochemical Research (2020)