Abstract
Serous endometrial intraepithelial carcinoma has been proposed to be a potential precursor lesion of pelvic high-grade serous carcinoma. If true, an increased incidence of uterine papillary serous carcinomas would be expected in BRCA1 and BRCA2 mutation carriers, who are at high-risk of developing pelvic high-grade serous carcinoma. This study explored particularly the occurrence of uterine papillary serous carcinoma, as well as other endometrial cancers, following risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 germline mutation attending a tertiary multidisciplinary clinic. A consecutive series of women with a BRCA1 or BRCA2 mutation who had undergone risk-reducing salpingo-oophorectomy without hysterectomy at the University Medical Center Groningen from January 1996 until March 2012 were followed prospectively. They were crossed with the histopathology list of endometrial cancer diagnoses reported by the Dutch nationwide pathology database PALGA. To assess the risk of endometrial cancer, a standardized incidence ratio was calculated comparing the observed with the expected number of endometrial cancer cases. Overall, 201 BRCA1 and 144 BRCA2 mutation carriers at a median age of 50 years (range, 32–78) were analyzed. After a median follow-up period of 6 years, after risk-reducing salpingo-oophorectomy, two cases of endometrial cancer were diagnosed, whereas the expected number was 0.94 cases (standardized incidence ratio 2.13; 95% confidence interval 0.24–7.69; P=0.27). Both endometrial cancer cases were of the endometrioid histological subtype. We showed that the incidence of endometrial cancer following risk-reducing salpingo-oophorectomy, especially uterine papillary serous carcinoma, in women at high-risk of developing pelvic high-grade serous carcinoma is not increased. On the basis of our data, the hypothesis of serous endometrial intraepithelial carcinoma being an important precursor lesion of pelvic high-grade serous carcinoma seems unlikely. There is no need to add a prophylactic hysterectomy to risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers.
Similar content being viewed by others
Main
Epithelial ovarian cancer is the fifth leading cause of cancer-related death in women in developed countries.1 Although there are many subtypes of ovarian cancer, serous carcinoma is the most frequently diagnosed histological type, which corresponds to 75% of all cases and 90% of all deaths due to ovarian cancer.2, 3 Serous carcinomas are even more common in female BRCA1 and BRCA2 mutation carriers, who are at an increased risk of developing ovarian cancer, currently known as pelvic high-grade serous carcinoma4, 5, 6 Although low-grade serous carcinomas (‘type I tumors’) are known to develop in a stepwise fashion, often associated with a serous borderline component,7, 8, 9 the cell of origin of pelvic high-grade serous carcinoma (‘type II tumors’) remains the subject of debate, despite extensive clinical, histopathological and fundamental research. One of the major aspects of this uncertainty is the precursor lesion responsible for this disease, as a precursor was never identified in the ovary itself.10
The first described precursor lesion of pelvic high-grade serous carcinoma in women with a genetic predisposition to ovarian cancer is the tubal intraepithelial carcinoma, later designated as noninvasive serous tubal intraepithelial carcinomas.11, 12 Recently, an alternative lesion was proposed to be a candidate precursor of pelvic high-grade serous carcinoma: serous endometrial intraepithelial carcinoma, an already established precursor lesion or early phase of uterine papillary serous carcinoma.13, 14 Serous endometrial intraepithelial carcinoma can be found near or adjacent to uterine papillary serous carcinoma in 50–90% of the cases.15, 16 If serous endometrial intraepithelial carcinoma indeed is an important precursor of pelvic high-grade serous carcinoma as well, one would expect an increased frequency of uterine papillary serous carcinoma in women at increased risk of developing pelvic high-grade serous carcinoma. Furthermore, uterine papillary serous carcinoma shares histopathologic, genetic and clinical features with pelvic high-grade serous carcinoma, which raised the hypothesis that uterine papillary serous carcinoma is a malignancy that might be associated with BRCA1 and BRCA2 mutations.
This study was undertaken to examine and report particularly the occurrence of uterine papillary serous carcinoma, as well as other endometrial cancers, following risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 germ line mutation in a tertiary referral medical center. The expected number of endometrial cancer cases was calculated, given the duration of follow-up and compared with the observed number of endometrial cancer cases.
Materials and methods
Context of Care
From 1996, clinical and genetic data of women with a BRCA1 or BRCA2 mutation have been prospectively registered at the Family Cancer Clinic of the University Medical Center Groningen, in a combined setting by a clinical geneticist, a gynecologic oncologist and a surgical oncologist.17 Genetic testing for BRCA mutations is available to women from hereditary breast and/or ovarian cancer families.18 Since 2009, annual gynecologic screening is not offered anymore because of the proven ineffectiveness19, 20, 21 and high-risk women are being counseled to undergo risk-reducing salpingo-oophorectomy after childbearing age, from the age of 35 in BRCA1 and from the age of 40–45 in BRCA2 mutation carriers. In the Netherlands, hysterectomy is not a part of the surgical protocol of risk-reducing salpingo-oophorectomy. Follow-up after risk-reducing salpingo-oophorectomy is performed by a surgical oncologist at the outpatient department of the Family Cancer Clinic of the University Medical Center Groningen.22, 23, 24
Study Design
Initially, a consecutive series of female BRCA1 and BRCA2 mutation carriers were enrolled, who underwent risk-reducing salpingo-oophorectomy (ICD 9-CM code 65.6) at the Department of Gynecology of the University Medical Center Groningen from 1 January 1996 to 1 March 2012. Excluded were women who had undergone a hysterectomy before or at risk-reducing salpingo-oophorectomy. The outcome of interest was particularly the occurrence of uterine papillary serous carcinoma, as well as other endometrial cancers, following risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. A password-protected database was used to enter the data. According to the Dutch clinical practice, no further Institutional Review Board approval was needed for this study.
Data Collection
Data of the BRCA1 and BRCA2 mutation carriers who underwent risk-reducing salpingo-oophorectomy were retrieved from the registration database of the Family Cancer Clinic. In addition, genetic, clinical, histopathological and follow-up data were obtained from medical records, surgical reports and pathology reports. To detect women who developed endometrial cancer, the nationwide pathology database ‘PALGA’ of The Netherlands was used, which is a national archive containing the abstracts of all pathology reports in the Netherlands since 1991.25 PALGA is a Dutch acronym and abbreviation for Pathologisch Anatomisch Landelijk Geautomatiseerd Archief, the Netherlands Nationwide Computer Network for Registry of cyto- and histopathology. Every record in the PALGA database contains date of diagnosis, and a summary of the report and diagnostic codes similar to the Systematized Nomenclature of Medicine (SNOMED)26 classification of the College of American Pathologists. From all BRCA1 and BRCA2 mutation carriers who underwent risk-reducing salpingo-oophorectomy, follow-up was checked using the PALGA database on the presence of any malignancy of the endometrium. The histological subtype of the endometrial cancer cases (endometrioid, uterine papillary serous or uterine clear-cell carcinoma) was recorded.
Statistical Analysis
SPSS 18.0 for Windows (SPSS, Chicago, IL, USA) was used to perform statistical analysis. Descriptive values of variables were expressed as frequencies and percentages for discrete data, and as median and range for continuous data. Follow-up time was calculated from the date of risk-reducing salpingo-oophorectomy to the date of hysterectomy, histopathological diagnosis of endometrial cancer or date of death, whichever occurred first; the data for women who were alive without endometrial cancer or hysterectomy were censored as the date of their last assessment at the Family Cancer Clinic, plus 1 year. The risk of endometrial cancer was quantified using the standardized incidence ratio, in which the observed number of endometrial cancers in our high-risk population was contrasted to the expected number. The expected number of endometrial cancer cases was calculated on the basis of the incidence of cancer in the general Dutch population from the 5-year age-specific rates at large with adjustment for age and calendar year. Incidence rates were obtained from the Dutch Cancer Registries. The number of observed cases was assumed to be Poisson-distributed and 95% confidence intervals were calculated according to the method of Byar.27 Tests were performed with a two-sided confidence interval and P values of <0.05 was considered statistically significant.
Results
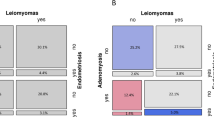
From 1 January 1996 until 1 March 2012, 315 women with BRCA1 or BRCA2 mutations underwent risk-reducing salpingo-oophorectomy (without hysterectomy), and were included in this study: 201 BRCA1 (64%) and 114 BRCA2 mutation carriers (36%) (Table 1, Figure 1). The median age at which risk-reducing salpingo-oophorectomy was carried out was 43 years (range, 30–71): BRCA1 mutation carriers at the age of 42 years (range, 30–71 years) and BRCA2 carriers at 45 (range, 33–66; P<0.001). risk-reducing salpingo-oophorectomy was performed following the diagnosis of primary breast cancer in 38% (N=118) of the women and tamoxifen was ever used by 6% (N=19) of the women; this concerned 16% of women who previously had breast cancer.
Flow-chart of study participants. Abbreviations: FCC=Family Cancer Clinic; UMCG=University Medical Center Groningen; RRSO=risk-reducing salpingo-oophorectomy; HBOC=hereditary breast and/or ovarian cancer family. *Indications for a hysterectomy before risk-reducing salpingo-oophorectomy: cervical intraepithelial neoplasia (N=2, both BRCA1); endometriosis (N=1, BRCA1); prolapse surgery (N=2, BRCA1 and BRCA2); metrorrhagia because of myomatous uterus (N=1, BRCA2); cervical cancer stage IA1 (N=1, BRCA1); cervical cancer stage IB1 (N=1, BRCA2); unknown (N=1, BRCA2). The case of hysterectomy at risk-reducing salpingo-oophorectomy was cervical cancer stage IAI (BRCA1). #Specification of both endometrial cancers: see Table 3. ¶Indications for a hysterectomy after risk-reducing salpingo-oophorectomy (N=4): cervical cancer stage IBI (radical hysterectomy), tubal carcinoma, ovarian carcinoma, primary peritoneal carcinoma. None of these patients had endometrial cancer or cancer in utero. †Causes of death after risk-reducing salpingo-oophorectomy (N=11): peritoneal cancer (N=1, BRCA1); ovarian cancer (N=1, BRCA1); non-hodgekin lymphoma (N=1, BRCA1); metastasized breast cancer (N=4, BRCA1; N=1, BRCA2); pancreatic cancer (N=1, BRCA2); unknown (N=2, BRCA2).
The current median age of the women who were alive without hysterectomy or endometrial cancer at the date of their last assessment at the Family Cancer Clinic was 50 years (range, 32–78; N=298). The total follow-up time after risk-reducing salpingo-oophorectomy of all subjects was 2 062 woman years, with a median follow-up of 6 years per woman (range, 0–27) (Table 2). Two women (1%) developed endometrial cancer during the follow-up period vs 0.94 endometrial cancers expected (standardized incidence ratio 2.13; 95% confidence interval 0.24–7.69; P=0.27) (Table 3). Both endometrial cancer cases were endometrioid adenocarcinomas. The first endometrial cancer case was in a 44-year-old BRCA1 mutation carrier who, also carried Lynch syndrome (MSH-2) and, developed a FIGO stage IA endometrioid cancer 7 months following risk-reducing salpingo-oophorectomy. Although she had been offered a hysterectomy together with risk-reducing salpingo-oophorectomy (because of Lynch syndrome), she preferred to wait until the age of 50. The second case was in a 39-year-old BRCA2 mutation carrier who developed a FIGO stage IA endometrioid cancer 66 months following risk-reducing salpingo-oophorectomy. Her family was positive for colon and endometrial cancer, and the tumor showed loss of MSH-6 expression; however, mutation analysis was negative for Lynch syndrome. Both women did not use tamoxifen in the past. After risk-reducing salpingo-oophorectomy, 4 women (all BRCA1 carriers) underwent a hysterectomy (1%) and 11 women were deceased at the end of the follow-up (4%). Indications for hysterectomy and causes of death are noted below Figure 1. None of the BRCA1 or BRCA2 mutation carriers developed uterine papillary serous carcinoma after risk-reducing salpingo-oophorectomy. Moreover, no cases of interval pelvic serous cancers, also known as primary peritoneal cancer, were diagnosed after risk-reducing salpingo-oophorectomy.
Discussion
In this prospectively collected series of women with a BRCA1 or BRCA2 mutation after risk-reducing salpingo-oophorectomy, the endometrial cancer incidence was not increased (standardized incidence ratio 2.13; 95% confidence interval 0.24–7.69; P=0.27). Strengths of this study are the consecutive and uniform series of high-risk women that were evaluated, availability of genetic, clinical and follow-up data and long duration of follow-up. Limitations of our study are the small sample size and the relatively young age at the end of follow-up.
Data are limited on whether or not women with a BRCA1 or BRCA2 mutation are at increased risk for endometrial cancer, especially uterine papillary serous carcinoma, besides pelvic high-grade serous carcinoma and breast cancer. Previous studies show conflicting results. In a series of 199 BRCA1 and BRCA2 mutation carriers, Levine et al28 showed that the lifetime risk of endometrial carcinoma is not increased in BRCA1 or BRCA2 carriers (odds ratio 0.75; 95% confidence interval 0.24–2.34; P=0.6). In contrast, the Breast Cancer Linkage Consortium reported an elevated risk of endometrial cancer in BRCA1 mutation carriers from North America and Western Europe (relative risk 2.65; 95% confidence interval 1.69–4.16; P<0.001), but not in BRCA2 carriers (odds ratio 1.25; 95% confidence interval 0.46–3.37).29, 30 Yet, the consortium did not provide information on previous tamoxifen treatment, and the histopathological subtype of the endometrial cancer remained unspecified. Also Beiner et al31 found an increased risk of endometrial cancer in a prospective series of 857 BRCA mutation carriers (standardized incidence ratio 5.3; P<0.001); however, the increased risk was contributed to previous tamoxifen treatment (26% of study participants) by the authors and not to BRCA mutations. Furthermore, all endometrial cancers were consequently of the endometrioid subtype, which can be related to tamoxifen use.31, 32 Lavie et al33 studied 51 women with uterine papillary serous carcinoma and found 8 (16%) women to be BRCA1 or BRCA2 mutation carriers. However, all patients were Asheknazi Jews and the high incidence of BRCA carriers among USPC patients in their series may be related to population bias Goshen et al34 specifically studied 56 unselected cases of uterine papillary serous carcinoma, and found that BRCA mutations do not appear to predispose to uterine papillary serous carcinoma.
In our study of 315 women with a BRCA1 or BRCA2 mutation, no cases of uterine papillary serous carcinoma occurred after risk-reducing salpingo-oophorectomy during a median follow-up of 6 years per woman (total of 2 062 women years). Two cases of endometrioid type endometrial cancer were diagnosed of which one occurred in a woman with Lynch syndrome (MSH-2), and the other one in a woman with a positive family history of endometrial cancer and MSH-6 loss in the tumor. We conclude that both endometrial cancer cases were attributable to loss of function of MSH2 and MSH6, and not to the BRCA mutations.
Given the age distribution of endometrial cancers, the women in our study population were relatively young (median, 50 years). However, the age distribution of the subject population was wide (range, 31–77) and 19% of the subjects were 60 years older at the time of last follow-up.
Four theories about the possible origin of both sporadic and hereditary pelvic high-grade serous carcinoma have been put forth. The first and conventional theory suggests the ovarian surface epithelium as the tissue of origin.35, 36 However, an ovarian precursor lesion was never identified.10
Second, the pelvic high-grade serous carcinoma may also develop from the secondary Müllarian system, which concerns metaplasia from the peritoneum; however, the rate of peritoneal cancer after risk-reducing salpingo-oophorectomy is low (∼1%).37, 38, 39, 40, 41
The third and currently most supported theory appoints the fallopian tube as the tissue of origin of pelvic high-grade serous carcinoma, least because a possible precursor lesion has been identified for the first time.12 Serous tubal intraepithelial carcinomas have been detected in the fallopian tube as the earliest morphological manifestation of high-grade serous carcinoma discovered so far, and are thought to subsequently spread to the ovary.11, 42 Examination of prophylactically removed ovaries and fallopian tubes of BRCA mutation carriers has been associated with serous tubal intraepithelial carcinoma in 3–12%43, 44, 45 and with occult carcinomas in 2–20%, which involve the distal fimbrial fallopian tube in majority of the cases.46, 47 Moreover, identical TP53 mutations in both serous tubal intraepithelial carcinomas and concomitant pelvic high-grade serous carcinoma indicate a clonal relationship between both, suggesting that the fimbrial end of the tube may be the ultimate origin for many pelvic high-grade serous carcinomas.48, 49
Recently, a fourth primary site was proposed, suggesting serous endometrial intraepithelial carcinoma to be a candidate precursor of pelvic high-grade serous carcinoma 13. In a case series of nine women, pelvic serous carcinoma and concurrent serous endometrial intraepithelial carcinomas were identified and identical TP53 mutations were found in six of the cases 50. Originally, serous endometrial intraepithelial carcinoma has been presumed to be an early phase of uterine papillary serous carcinoma that is capable of spreading beyond the uterus.15, 16 If serous endometrial intraepithelial carcinoma indeed is an important precursor of pelvic high-grade serous carcinoma as well as of uterine papillary serous carcinoma, an increased frequency of uterine papillary serous carcinoma would be expected in women at an increased risk of developing pelvic high-grade serous carcinoma. However, no increased incidence of uterine papillary serous carcinoma was found in our series and therefore, the hypothesis of serous endometrial intraepithelial carcinoma being an important precursor lesion of pelvic high-grade serous carcinoma in BRCA1 or BRCA2 mutation carriers seems unlikely. Nonetheless, if this hypothesis holds true, a hysterectomy should consequently be added to risk-reducing salpingo-oophorectomy for women carrying a BRCA1 or BRCA2 mutation.
Prophylactic hysterectomy does not appear to be generally indicated in BRCA1 and BRCA2 mutation carriers, as there is no convincing evidence that there is an increased risk of endometrial cancer in this population. Still, in some institutions a hysterectomy is added to risk-reducing salpingo-oophorectomy in order to entirely remove the proximal, intramural portion of the fallopian tube. Tubal cancer is typically located in the distal part of the fallopian tube. A large clinicopathological study of 105 tubal cancers showed that 92% of the tumor was situated within the fallopian tube, most often in its distal two-thirds.51 Furthermore, researchers from the University of Miami studied 2 632 ovarian cancer cases and reported that 4.5–14.1% of women developed ovarian cancer after prior hysterectomy for non-ovarian conditions.52 Similarly, the American College of Surgeons studied a larger series of 12 316 ovarian cancer cases and reported that 18.2% of these women had a previous hysterectomy for benign disease, with ovarian preservation.53 No clinical trials have yet been performed to study additional risk-reduction of tubal cancer by adding a hysterectomy to risk-reducing salpingo-oophorectomy. Furthermore, the relatively simple laparoscopic risk-reducing salpingo-oophorectomy would be more extended and expensive, and might be accompanied by a higher surgical morbidity, a higher risk of complications and a longer patient recovery time.54 According to our data, there is no clinical indication to add a hysterectomy to risk-reducing salpingo-oophorectomy in women at high-risk of developing pelvic high-grade serous carcinoma.
In conclusion, over a 16-year period, we did not find an increased risk of endometrial cancer in BRCA1 or BRCA2 mutation carriers at high risk for developing pelvic high-grade serous carcinoma, attending our tertiary multidisciplinary center. Taken together, these data do not support the hypothesis of serous endometrial intraepithelial carcinoma being an important precursor lesion of pelvic high-grade serous carcinoma in BRCA1 or BRCA2 mutation carriers and there is no clinical indication to add hysterectomy to risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers.
References
Jemal A, Siegel R, Xu J et al. Cancer statistics. 2010 CA Cancer J Clin 2010;60:277–300.
Cho KR, Shih IeM . Ovarian cancer. Annu Rev Pathol 2009;4:287–313.
Seidman JD, Horkayne-Szakaly I, Haiba M et al. The histologic type and stage distribution of ovarian carcinomas of surface epithelial origin. Int J Gynecol Pathol 2004;23:41–44.
Boyd J, Sonoda Y, Federici MG et al. Clinicopathologic features of BRCA-linked and sporadic ovarian cancer. JAMA 2000;283:2260–2265.
Risch HA, McLaughlin JR, Cole DE et al. Prevalence and penetrance of germline BRCA1 and BRCA2 mutations in a population series of 649 women with ovarian cancer. Am J Hum Genet 2001;68:700–710.
Shaw PA, McLaughlin JR, Zweemer RP et al. Histopathologic features of genetically determined ovarian cancer. Int J Gynecol Pathol 2002;21:407–411.
Shih Ie M, Kurman RJ . Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Am J Pathol 2004;164:1511–1518.
Singer G, Oldt R, Cohen Y et al. Mutations in BRAF and KRAS characterize the development of low-grade ovarian serous carcinoma. J Natl Cancer Inst 2003;95:484–486.
Singer G, Stohr R, Cope L et al. Patterns of p53 mutations separate ovarian serous borderline tumors and low- and high-grade carcinomas and provide support for a new model of ovarian carcinogenesis: a mutational analysis with immunohistochemical correlation. Am J Surg Pathol 2005;29:218–224.
Reitsma W, Hollema H, Mourits MJ. . Letter commenting on ‘Risk-Reducing Salpingo-Oophorectomy (RRSO) in BRCA mutation carriers: experience with a consecutive series of 111 patients using a standardized surgical-pathological protocol. Int J Gynecol Cancer 2011;21:846–851 by C. Bethan Powell et al. Int J Gynecol Cancer ‘2011.
Jarboe E, Folkins A, Nucci MR et al. Serous carcinogenesis in the fallopian tube: a descriptive classification. Int J Gynecol Pathol 2008;27:1–9.
Piek JM, van Diest PJ, Zweemer RP et al. Dysplastic changes in prophylactically removed Fallopian tubes of women predisposed to developing ovarian cancer. J Pathol 2001;195:451–456.
Massuger L, Roelofsen T, Ham M, Bulten J . The origin of serous ovarian cancer may be found in the uterus: a novel hypothesis. Med Hypotheses 2010;74:859–861.
Sherman ME, Bitterman P, Rosenshein NB, Delgado G, Kurman RJ . Uterine serous carcinoma. A morphologically diverse neoplasm with unifying clinicopathologic features. Am J Surg Pathol 1992;16:600–610.
Ambros RA, Sherman ME, Zahn CM, Bitterman P, Kurman RJ . Endometrial intraepithelial carcinoma: a distinctive lesion specifically associated with tumors displaying serous differentiation. Hum Pathol 1995;26:1260–1267.
Hendrickson M, Ross J, Eifel P, Martinez A, Kempson R . Uterine papillary serous carcinoma: a highly malignant form of endometrial adenocarcinoma. Am J Surg Pathol 1982;6:93–108.
De Bock GH, Hesselink JW, Roorda C et al. Model of care for women at increased risk of breast and ovarian cancer. Maturitas 2012;71:3–5.
The Netherlands Foundation for the Detection of Hereditary Tumours (STOET). Guideline for diagnosis and prevention. Available athttp://www.stoet.nl/uploads/richtlijnenboekje.pdf (viewed on 1 November 2011).
Oei AL, Massuger LF, Bulten J et al. Surveillance of women at high risk for hereditary ovarian cancer is inefficient. Br J Cancer 2006;94:814–819.
Hermsen BB, Olivier RI, Verheijen RH et al. No efficacy of annual gynaecological screening in BRCA1/2 mutation carriers; an observational follow-up study. Br J Cancer 2007;96:1335–1342.
van der Velde NM, Mourits MJ, Arts HJ et al. Time to stop ovarian cancer screening in BRCA1/2 mutation carriers? Int J Cancer 2009;124:919–923.
Madalinska JB, Hollenstein J, Bleiker E et al. Quality-of-life effects of prophylactic salpingo-oophorectomy versus gynecologic screening among women at increased risk of hereditary ovarian cancer. J Clin Oncol 2005;23:6890–6898.
Madalinska JB, van Beurden M, Bleiker EM et al. The impact of hormone replacement therapy on menopausal symptoms in younger high-risk women after prophylactic salpingo-oophorectomy. J Clin Oncol 2006;24:3576–3582.
Fakkert IE, Jansen L, Meijer K et al. Breast cancer screening in BRCA1 and BRCA2 mutation carriers after risk reducing salpingo-oophorectomy. Breast Cancer Res Treat 2011;129:157–164.
van Niekerk CC, Vooijs GP, Bulten J . Increased risk of concurrent primary malignancies in patients diagnosed with a primary malignant epithelial ovarian tumor. Mod Pathol 2007;20:384–388.
Hemminki K, Aaltonen L, Li X . Subsequent primary malignancies after endometrial carcinoma and ovarian carcinoma. Cancer 2003;97:2432–2439.
Byar D . Rates and standardization, In: Breslow NE, Day NE, (eds). Statistical Methods in Cancer Research. Vol II, The Design and Analysis of Cohort Studies. p69, International Agency for Research on Cancer: Lyon, France, 1987.
Levine DA, Lin O, Barakat RR et al. Risk of endometrial carcinoma associated with BRCA mutation. Gynecol Oncol 2001;80:395–398.
Thompson D, Easton DF . Cancer Incidence in BRCA1 mutation carriers. J Natl Cancer Inst 2002;94:1358–1365.
Cancer risks in BRCA2 mutation carriers. The breast cancer linkage consortium. J Natl Cancer Inst 1999;91:1310–1316.
Beiner ME, Finch A, Rosen B et al. The risk of endometrial cancer in women with BRCA1 and BRCA2 mutations. A prospective study. Gynecol Oncol 2007;104:7–10.
Bland AE, Calingaert B, Secord AA et al. Relationship between tamoxifen use and high risk endometrial cancer histologic types. Gynecol Oncol 2009;112:150–154.
Lavie O, Ben-Arie A, Segev Y et al. BRCA germline mutations in women with uterine serous carcinoma—still a debate. Int J Gynecol Cancer 2010;20:1531–1534.
Goshen R, Chu W, Elit L et al. Is uterine papillary serous adenocarcinoma a manifestation of the hereditary breast-ovarian cancer syndrome? Gynecol Oncol 2000;79:477–481.
Fathalla MF . Incessant ovulation—a factor in ovarian neoplasia? Lancet 1971;2:163.
Scully RE . Early de novo ovarian cancer and cancer developing in benign ovarian lesions. Int J Gynaecol Obstet 1995;49 (Suppl):S9–S15.
Rebbeck TR, Lynch HT, Neuhausen SL et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med 2002;346:1616–1622.
Domchek SM, Friebel TM, Garber JE et al. Occult ovarian cancers identified at risk-reducing salpingo-oophorectomy in a prospective cohort of BRCA1/2 mutation carriers. Breast Cancer Res Treat 2010;124:195–203.
Powell CB, Chen LM, McLennan J et al. Risk-reducing salpingo-oophorectomy (RRSO) in BRCA mutation carriers: experience with a consecutive series of 111 patients using a standardized surgical-pathological protocol. Int J Gynecol Cancer 2011;21:846–851.
Meeuwissen PA, Seynaeve C, Brekelmans CT et al. Outcome of surveillance and prophylactic salpingo-oophorectomy in asymptomatic women at high risk for ovarian cancer. Gynecol Oncol 2005;97:476–482.
Rhiem K, Foth D, Wappenschmidt B et al. Risk-reducing salpingo-oophorectomy in BRCA1 and BRCA2 mutation carriers. Arch Gynecol Obstet 2011;283:623–627.
Kindelberger DW, Lee Y, Miron A et al. Intraepithelial carcinoma of the fimbria and pelvic serous carcinoma: evidence for a causal relationship. Am J Surg Pathol 2007;31:161–169.
Callahan MJ, Crum CP, Medeiros F et al. Primary fallopian tube malignancies in BRCA-positive women undergoing surgery for ovarian cancer risk reduction. J Clin Oncol 2007;25:3985–3190.
Leeper K, Garcia R, Swisher E et al. Pathologic findings in prophylactic oophorectomy specimens in high-risk women. Gynecol Oncol 2002;87:52–56.
Lamb JD, Garcia RL, Goff BA, Paley PJ, Swisher EM . Predictors of occult neoplasia in women undergoing risk-reducing salpingo-oophorectomy. Am J Obstet Gynecol 2006;194:1702–1709.
Evans DG, Clayton R, Donnai P, Shenton A, Lalloo F . Risk-reducing surgery for ovarian cancer: outcomes in 300 surgeries suggest a low peritoneal primary risk. Eur J Hum Genet 2009;17:1381–1385.
Hirst JE, Gard GB, McIllroy K, Nevell D, Field M . High rates of occult fallopian tube cancer diagnosed at prophylactic bilateral salpingo-oophorectomy. Int J Gynecol Cancer 2009;19:826–829.
Kuhn E, Kurman RJ, Vang R et al. TP53 mutations in serous tubal intraepithelial carcinoma and concurrent pelvic high-grade serous carcinoma—evidence supporting the clonal relationship of the two lesions. J Pathol 2012;226:421–426.
Lee Y, Miron A, Drapkin R et al. A candidate precursor to serous carcinoma that originates in the distal fallopian tube. J Pathol 2007;211:26–35.
Roelofsen T, van Kempen LC, van der Laak JA et al. concurrent endometrial intraepithelial carcinoma (EIC) and serous ovarian cancer: can EIC be seen as the precursor lesion? Int J Gynecol Cancer 2012;22:457–464.
Alvarado-Cabrero I, Young RH, Vamvakas EC, Scully RE . Carcinoma of the fallopian tube: a clinicopathological study of 105 cases with observations on staging and prognostic factors. Gynecol Oncol 1999;72:367–379.
Piver MS. . Prophylactic oophorectomy: reducing the US death rate from epithelial ovarian cancer. a continuing debate. Oncologist 1996;1:326–330.
Averette HE, Hoskins W, Nguyen HN et al. National survey of ovarian carcinoma. I. A patient care evaluation study of the American College of Surgeons. Cancer 1993;71:1629–1638.
Mourits MJ, De Hullu JA, Van Der Zee AG, Hollema H . Letter commenting on ‘Pathologic finding in prophylactic oophorectomy specimens in high-risk women’ (87:52–6) by Pamela Paley, et al. (fax: +31-206-685-9607). Gynecol Oncol 2004;93:571.
Acknowledgements
We wish to express our appreciation to Ms Trea Tjoelker for performing the PALGA search. Also we want to acknowledge Ms Ingrid E Fakkert for updating part of the database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Reitsma, W., Mourits, M., de Bock, G. et al. Endometrium is not the primary site of origin of pelvic high-grade serous carcinoma in BRCA1 or BRCA2 mutation carriers. Mod Pathol 26, 572–578 (2013). https://doi.org/10.1038/modpathol.2012.169
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.169
Keywords
This article is cited by
-
Risk of endometrial cancer after RRSO in BRCA 1/2 carriers: a multicentre cohort study
Clinical and Translational Oncology (2023)
-
Association between BRCA mutations and endometrial carcinoma: a systematic review with meta-analysis
Archives of Gynecology and Obstetrics (2021)
-
Endometrial cancer gene panels: clinical diagnostic vs research germline DNA testing
Modern Pathology (2017)
-
Early salpingectomy (TUbectomy) with delayed oophorectomy to improve quality of life as alternative for risk-reducing salpingo-oophorectomy in BRCA1/2 mutation carriers (TUBA study): a prospective non-randomised multicentre study
BMC Cancer (2015)