Abstract
Estrogen receptor (ER) status is a strong predictor of response to hormonal therapy in breast cancer patients. Presence of ER and level of expression have been shown to correlate with time to recurrence in patients undergoing therapy with tamoxifen or aromatase inhibitors. Risk reduction is also known to occur in ER-negative, progesterone receptor (PR)-positive patients treated with hormonal therapy. Since the 1990s, immunohistochemistry has been the primary method for assessing hormone receptor status. Recently, as a component of its oncotype DX® assay, Genomic Health began reporting quantitative estrogen and PR results determined by quantitative reverse transcription polymerase chain reaction (qRT-PCR). As part of an ongoing quality assurance program at our institution, we reviewed 464 breast cancer cases evaluated by both immunohistochemistry and oncotype DX® assay for estrogen and PR. We found good correlation for ER status between both assays (98.9% concordance), with immunohistochemistry being slightly more sensitive. Concordance for PR was 94.2% between immunohistochemistry and qRT-PCR with immunohistochemistry again more sensitive than RT-PCR. The results also showed linear correlation between immunohistochemistry H-scores and qRT-PCR expression values for ER (correlation coefficient of 0.579), and PR (correlation coefficient of 0.685). Due to the higher sensitivity of hormone receptor immunohistochemistry and additional advantages (ie preservation of morphology, less expensive, faster, more convenient), we conclude immunohistochemistry is preferable to qRT-PCR for determination of estrogen and PR expression.
Similar content being viewed by others
Main
Estrogen receptor (ER) status is a proven prognostic marker in breast cancer; however, its main clinical value is its ability to predict response to hormonal therapy. Most laboratories in the United States use immunohistochemistry to determine ER and progesterone receptor (PR) results on primary breast carcinomas. However, the method of reporting hormone receptor immunohistochemical results has been quite controversial over the years. The recent American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) guideline recommendations for hormonal immunohistochemistry testing have suggested that although the likelihood of response to hormonal therapy appears to be directly related to the amount of hormone receptor expressed in tumor cells, patients with as little as 1% hormone receptor expression may still benefit from hormonal therapy.1 This suggests potential benefit for reporting even very low levels of hormone receptor positivity, and the ASCO/CAP guidelines further recommend reporting both the proportion and intensity of hormone receptor protein expression in a semiquantitative manner.1
Oncotype DX® (Genomic Health, Redwood City, CA, USA) is a commercial assay designed to assess tumor recurrence probability in node-negative ER-positive breast cancers. It utilizes quantitative reverse transcription-polymerase chain reaction (qRT-PCR) to analyze the expression of 21 genes (16 cancer-related and 5 control genes) to provide an estimated distant disease recurrence score ranging from 0 to 100.2 The recurrence score was determined on the basis of national surgical adjuvant breast and bowel project training set data and proprietary analytic methods. Currently the test is widely used by oncologists for the optimization of clinical management. Recently, Genomic Health began reporting separate ER and PR expression units (compared with reference genes) to provide a qRT-PCR measurement of hormone receptor status.
As part of an ongoing quality assurance program at our institution, we previously reported pilot data comparing hormone receptor expression between immunohistochemistry and qRT-PCR.3 The objective of the current study was to expand on this comparison utilizing a much larger dataset.
Materials and methods
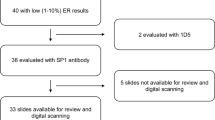
We identified 464 breast cancer cases at Magee-Womens Hospital (from the year 2008 and 2009), which were analyzed by Oncotype DX® by qRT-PCR with supplemental reporting of ER/PR expression units. The Oncotype DX® assay was performed on one tissue block from an appropriately fixed (8–72 h) resection specimen in each case. On all cases a tumor tissue block was sent for Oncotype DX® testing to Genomic Health on clinician's request. Subsequent analysis including qRT-PCR for hormone receptors was performed at Genomic Health. According to the company's reporting criteria, a tumor is considered ER positive with expression units of ≥6.5 and PR positive with expression units of ≥5.5.
Immunohistochemical hormone receptor analysis was performed on corresponding core-needle biopsies at the time of initial diagnosis. ER expression was assessed using the antibody clone SP1 and PR using clone 1E2. Immunohistochemical staining for both antibodies was performed using iVIEW detection on the Benchmark XT system (Ventana, Tuscon, AZ). The cases with discordant immunohistochemistry and RT-PCR results were re-examined by immunohistochemistry on the same tissue block that was sent for oncotype DX® testing to exclude any possibility of tissue heterogeneity accounting for the discordance.
Hormone receptor immunohistochemical semi-quantitation was determined using the modified H-score. The score consists of the sum of the percent of tumor cells staining multiplied by an ordinal value corresponding to the intensity level (0=none, 1=weak, 2=moderate, and 3=strong). With four intensity levels, the resulting score ranges from 0 (no staining in the tumor) to 300 (diffuse intense staining of the tumor).4, 5 Examples of ER and PR immunohistochemical stains, and corresponding H-score calculations are shown in Figures 1a–d. In accordance to ASCO/CAP guidelines, an H-score of ≥1 was considered a positive result for both ER and PR.
Modified H-score examples (range: 0 to 300). Case (a) (strong ER positive; H-score 300), 0: 0%, 1+: 0%, 2+: 0%, 3+: 100%. ER H-score=(0 × 0)+(1 × 0)+(2 × 0)+(3 × 100)=300. Case (b) (heterogeneous but still strong PR positive; H-score 205), 0: 25%, 1+: 5%, 2+: 10%, 3+: 60%. PR H-score=(0 × 25)+(1 × 5)+(2 × 10)+(3 × 60)=205. Case (c) (moderate ER positive; H-score 135), 0: 10%, 1+: 50%, 2+: 35%, 3+: 5%. ER H-score=(0 × 10)+(1 × 50)+(2 × 35)+(3 × 5)=135. Case (d) (weak PR positive; H-score 30), 0: 85%, 1+: 5%, 2+: 5%, 3+: 5%. PR H-score=(0 × 85)+(1 × 5)+(2 × 5)+(3 × 5)=30.
RT-PCR and immunohistochemistry results were compared qualitatively (positive/negative), and quantitatively using Pearson correlation.
Results
All cases sent for oncotype DX® testing were positive for ER on core biopsy except one. The exact reason for the test order on ER-negative case is unknown. Of the total 464 cases, the ER results were concordant on 457 cases (98.5%) between immunohistochemistry and Genomic Health qRT-PCR assay (Table 1). All ER discordant cases were positive by immunohistochemistry and negative by qRT-PCR with a mean H-score of 82 (median 25; range 10–225). In order to exclude the possibility of tissue heterogeneity, ER immunohistochemistry was repeated on all discordant cases on the same tissue block that was sent for oncotype DX® testing (see results after repeat testing in Table 2). Of these six discordant cases, five remained unequivocally ER positive on repeat immunohistochemistry testing with a mean H-score of 105.4 (median 40; range: 2 to 240). The one negative case on repeat testing showed occasional positive cells but was judged to be less than 1% of the entire tumor and therefore interpreted as negative. After repeat immunohistochemistry testing, the sensitivity of qRT-PCR in comparison to ER immunohistochemistry was 98.9% (457/462), specificity (based on 2 cases only) was 100%, positive predictive value of 100% (457/457), and negative predictive value of 28.6% (2/7).
The overall concordance between immunohistochemistry and qRT-PCR for PR was 91.2% (423/464). Of the 41 discordant cases, 7 cases were immunohistochemistry negative- but qRT-PCR positive- and 34 cases were immunohistochemistry positive but negative by Genomic Health qRT-PCR assay (Table 3). Of the 34 immunohistochemistry-positive/qRT-PCR-negative cases, 20 had H-scores of 10 or higher. In order to exclude the possibility of tissue heterogeneity accounting for the discordance, PR immunohistochemistry was repeated on all 41 discordant cases on the same tissue block that was sent for oncotype DX® testing (see results after repeat testing in Table 4). On repeat immunohistochemistry testing, the seven immunohistochemistry-negative/qRT-PCR-positive cases, six showed immunoreactivity with a mean PR H-score of 51 (median: 40.5; range: 2 to 150). The one negative case on repeat testing showed occasional positive cells but was judged to be less than 1% of the entire tumor and therefore interpreted as negative. However, the intermixed in-situ carcinoma and normal ducts showed unequivocal reactivity for PR (Figure 2).
This case of invasive carcinoma was interpreted as PR positive by oncotype qRT-PCR assay (expression units of 6.7) but remained negative by immunohistochemistry even on repeat testing. Note that the ductal carcinoma in situ (a) is positive for PR (b). The intermixed normal duct (c) also shows unequivocal reactivity for PR (d).
On repeat immunohistochemistry testing of 34 PR immunohistochemistry-positive/qRT-PCR-negative cases, 26 remained unequivocally positive by immunohistochemistry with a mean PR H-score of 24.2 (median: 9.5; range: 1–110). These 26 cases were slightly more intensely positive on initial core biopsy testing with a mean H-score of 56.2 (median: 30; range 1–270). No tumor tissue was available on one case for repeat testing. The remaining seven initially immunohistochemistry-positive cases that tested negative on repeat testing, five showed occasional positive cells but were judged to be less than 1% of the entire tumor and therefore interpreted as negative. These seven cases were weakly positive on initial core biopsy testing with a mean H-score of 17.9 (median: 6; range: 2–90). After repeat immunohistochemistry testing, the sensitivity of qRT-PCR in comparison to PR immunohistochemistry was 93.9% (401/427), specificity was 97.2% (35/36), positive predictive value of 99.8% (401/402), and negative predictive value of 57.4% (35/61).
The data was also examined for semi-quantitative immunohistochemistry and qRT-PCR results (expression units) using Pearson correlation. A linear correlation was obtained between immunohistochemistry and qRT-PCR results for both ER and PR (Figures 3 and 4). Regarding ER, H-scores ranged from 0 to 300, RT-PCR units ranged from <3.7 to 12, and the correlation coefficient was 0.579. For PR, H-scores ranged from 0 to 300, RT-PCR units ranged from <3 to >10, and the correlation coefficient was 0.685.
Discussion
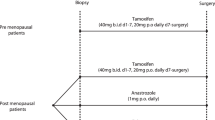
ER and PR status is an important factor in determining whether a patient will be treated with hormonal therapy. A meta-analysis of randomized trials evaluating the relative risk of relapse in patients who did or did not receive tamoxifen demonstrated the benefit of hormonal therapy as adjuvant treatment.6 In two randomized controlled trials of tamoxifen therapy versus no treatment supported the use of tamoxifen as adjuvant therapy.7 As it has been demonstrated that time to recurrence varies inversely with hormone receptor expression,8 each patients’ likelihood of benefiting from hormonal therapy depends significantly on the degree of ER and PR expression.9, 10, 11, 12, 13, 14, 15 As tamoxifen has been associated with increased incidence of thromboembolic events and endometrial cancer, it is necessary to evaluate risk versus benefit for each patient.16 As there is a correlation between level of ER expression and response to hormonal therapy, as well as a potential benefit for therapy in patients with as little as 1% ER expression, accurate quantitative or semiquantitative determination of ER expression is crucial for patient management.
Although it is well known that ER status has value in predicting which patients are most likely to benefit from hormonal therapy, it has also been suggested that ER analysis by itself is in some cases insufficient, and assessment of PR provides additional value.14, 15, 17, 18, 19 Dowsett et al,7 reported that ER-negative PR-positive patients may also derive benefit from tamoxifen. These findings support the significance of accurately determining not only ER but also PR status.
ER and PR expression are generally determined by semiquantitative immunohistochemistry, as recently outlined by the ASCO/CAP recommendations.1 Factors such as warm and cold ischemic time, fixation type and duration, antibody clones, control samples, assay interpretation and reporting, and internal quality control and validation render immunohistochemistry testing subject to variability. At our institution, tissue handling and fixation protocol have been standardized since 2007, and all resection specimens included in this study were fixed for time periods between 8 and 72 h. In all cases, we used the food and drug administration cleared antibody, SP1 ER clone which recent studies have suggested is at least as sensitive, if not more than other clones such as 1D5 and 6F11.20, 21 PR was also evaluated using the food and drug administration cleared rabbit monoclonal antibody clone 1E2, which also has similar or better performance than other clones such as clone 16, and PGR636.22 In addition, each case was evaluated using standardized controls, assay interpretation, scoring (modified H-score), quality control and validation. Such measures taken in our study are expected to reduce variability among our specimens and increase sensitivity of hormone receptor detection.
In the oncotype DX® assay, quantification of ER and PR expression is performed by RT-PCR of RNA extracted from paraffin-embedded tissues. These values are reported as a supplement to the overall assay score used to estimate recurrence risk in node-negative, ER-positive breast carcinomas. Similar to immunohistochemistry, hormone receptor results determined by qRT-PCR are also subject to variation in analytical variables. These include differences in fixation, RNA extraction technique, RT-PCR protocols, machines, primer/probe selection, and reagents. Perhaps more significantly, qRT-PCR requires accurate microdissection of the invasive tumor from intact tissue specimens as well as subsequent grinding of the tissue. As such, the qRT-PCR assay is a non-morphologic technique, and contamination of tumor mRNA with either normal breast tissue or in-situ carcinoma can significantly affect quantitative ER and PR results.
Our series demonstrates that semiquantitative ER immunohistochemistry provides results similar to quantitative RT-PCR (98.9% concordance), although immunohistochemistry had a higher sensitivity. A linear correlation with a correlation coefficient of 0.579 was achieved when immunohistochemistry and RT-PCR were compared quantitatively. As all discordant cases were positive for ER expression by immunohistochemistry and negative by RT-PCR and these cases were relatively weak to moderate positive immunohistochemically (mean H-score of 105.4), the immunohistochemistry methodology appears to be superior to qRT-PCR in detecting hormonal positivity in tumors with low intensity or heterogeneous ER expression.
There was slightly less qualitative concordance rate (94.2%) for PR in comparison to ER. However, similar to ER, quantitative analysis resulted in linear correlation with a correlation coefficient of 0.685. Approximately 6% of cases were positive by immunohistochemistry but negative by RT-PCR compared with <1% of cases positive by RT-PCR and negative by immunohistochemistry, suggesting that immunohistochemistry is more sensitive in detecting PR expression. The cases that tested positive for PR by immunohistochemistry (on repeat testing) and negative by RT-PCR were relatively weak positive immunohistochemically (mean H-score of 53.2), suggesting immunohistochemistry is superior to RT-PCR in detecting hormonal positivity in tumors with low intensity or heterogeneous expression. Only one case (0.2%) tested negative for PR by immunohistochemistry (on repeat testing) and positive by RT-PCR. The issue of contamination of tumor mRNA with non-invasive tumor tissue in RT-PCR could potentially account for discrepancy in this case as the surrounding and intermixed normal breast tissue and in-situ carcinoma showed patchy moderate to strong staining for PR (Figure 2).
In a similar study but using tissue microarray and different antibody clones, Badve et al23 (in concert with Genomic Health) compared central immunohistochemistry for ER and PR with oncotype DX® qRT-pCR assay on 776 cases. For ER, the concordance between central immunohistochemistry and central RT-PCR was 93%. For PR, the concordance between central immunohistochemistry and central RT-PCR was 90%. In this study immunohistochemistry ER-negative cases that were RT-PCR positive were more common than immunohistochemistry ER-positive cases that were RT-PCR negative (unlike our study). However, in regards to PR, immunohistochemistry PR-negative cases that were RT-PCR positive were less common than immunohistochemistry PR-positive cases that were RT-PCR negative (similar to our study). The reasons for the difference between Badve et al study and our study include immunohistochemistry analysis on very small samples (ie tissue microarray), and possibly using less optimally fixed tissue and less sensitive antibodies by Badve et al.23
In our study, initial immunohistochemistry was performed on core biopsies, whereas resection specimens were used for the RT-PCR assay. Studies suggest high concordance between qualitative ER expression in core biopsies versus resection specimens.24 However, there may be some variation in the level of expression between the two,24 and this may have contributed to some initial discordance and less than perfect correlation coefficients. However, it must be noted that for all qualitatively discordant cases, immunohistochemistry for ER and/or PR was repeated on the same tissue block of the resection specimen that was sent for oncotype DX®. In this way, we were able to exclude tumor heterogeneity as the cause for discordance between immunohistochemistry and qRT-PCR assays. Therefore, the slight discordance between immunohistochemistry and qRT-pCR seen is this study is real and indicates that immunohistochemistry is more sensitive than qRT-PCR for evaluation of ER and PR.
Although the inability of Genomic Health qRT-PCR assay to recognize low to moderate hormone receptor expressing tumors does not appear to be very significant when the data is statistically analyzed, but these results are clinically significant for individual patients and oncologists. In our clinical experience with these cases, we have been contacted by clinicians who are unsure about which test result to use for making clinical decisions. The additional reporting of qRT-PCR ER and PR results on oncotype report confuses clinicians and unnecessarily creates doubt about validated immunohistochemistry assays. For the benefit of the patients and clinicians, we believe it is imperative for the laboratory medical director to issue an addendum report to reconcile the false negative hormone receptor results on oncotype DX® reports, so that patients are treated appropriately.
Finally it should be noted that we have recently reported our results on HER2 immunohistochemistry/fluorescence in-situ hybridization concordance with GHI qRT-pCR results and found excellent percent negative agreement but sub-optimal percent positive agreement.25 Our analysis pointed towards dilution of tumor mRNA with non-tumoral tissues as one of the prominent explanation for sub-optimal positive agreement. However, this ‘dilution artifact’ does not seem to affect qualitative hormone receptor results significantly as the surrounding and intermixed normal breast tissue is often ER/PR positive. Therefore, in cases contaminated by excessive normal tissue, a qRT-PCR assay (a non-morphologic technique) may give a false negative result for a gene not expressed by normal tissues (such as HER2) but may still give a positive result for hormone receptors on low ER/PR expressing tumor or a false positive result on an ER/PR negative tumor. Although qualitative hormone receptor results appears to be less commonly affected, this variation in quantification has the potential to impact the overall recurrence score, which according to published literature is heavily affected by tumor hormone receptor content, HER2 status, and proliferation.2, 4, 26, 27
In summary, our study demonstrates good overall concordance for qualitative ER and PR results when comparing immunohistochemistry to qRT-PCR. However, our results suggest immunohistochemistry is more sensitive for both ER and PR detection. Immunohistochemistry offers additional advantages such as lower expense, ease of use, and faster turnaround time. Moreover, morphology is preserved in the immunohistochemistry procedure, allowing for recognition of immunostain heterogeneity and confirmation that the identified positivity is localized to the nuclei of invasive tumor cells. Finally, as qRT-PCR requires tissue microdissection and grinding for analysis, samples are inherently at risk for contamination with normal ductal breast tissue, fibroadipose tissue, inflammatory cells, biopsy cavities, and in-situ carcinoma. For all of these practical reasons, we conclude immunohistochemistry assays are superior to qRT-PCR for analysis of ER and PR status in the management of breast cancer patients.
References
Hammond ME, Hayes DF, Wolff AC, et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract 2010;6:195–197.
Paik S, Shak S, Tang G, et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 2004;351:2817–2826.
O’Connor SM, Beriwal S, Dabbs DJ, et al. Concordance between semiquantitative immunohistochemical assay and oncotype DX RT-PCR assay for estrogen and progesterone receptors. Appl Immunohistochem Mol Morphol 2010;18:268–272.
Flanagan MB, Dabbs DJ, Brufsky AM, et al. Histopathologic variables predict Oncotype DX recurrence score. Mod Pathol 2008;21:1255–1261.
McCarty Jr KS, Miller LS, Cox EB, et al., McCarty Sr. KS Estrogen receptor analyses. Correlation of biochemical and immunohistochemical methods using monoclonal antireceptor antibodies. Arch Pathol Lab Med 1985;109:716–721.
Early Breast Cancer Trialists’ Collaborative Group.. Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet 1998;351:1451–1467.
Dowsett M, Houghton J, Iden C, et al. Benefit from adjuvant tamoxifen therapy in primary breast cancer patients according oestrogen receptor, progesterone receptor, EGF receptor and HER2 status. Ann Oncol 2006;17:818–826.
Dowsett M, Allred C, Knox J, et al. Relationship between quantitative estrogen and progesterone receptor expression and human epidermal growth factor receptor 2 (HER-2) status with recurrence in the arimidex, tamoxifen, alone or in combination trial. J Clin Oncol 2008;26:1059–1065.
Harvey JM, Clark GM, Osborne CK, et al. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol 1999;17:1474–1481.
Cowen PN, Teasdale J, Jackson P, et al. Oestrogen receptor in breast cancer: prognostic studies using a new immunohistochemical assay. Histopathology 1990;17:319–325.
Elledge RM, Green S, Pugh R, et al. Estrogen receptor (ER) and progesterone receptor (PgR), by ligand-binding assay compared with ER, PgR and pS2, by immuno-histochemistry in predicting response to tamoxifen in metastatic breast cancer: a Southwest Oncology Group Study. International J Cancer 2000;89:111–117.
Esteban JM, Ahn C, Battifora H, et al. Quantitative immunohistochemical assay for hormonal receptors: technical aspects and biological significance. J Cell Biochem Suppl 1994;19:138–145.
Lockwood CA, Ricciardelli C, Raymond WA, et al. A simple index using video image analysis to predict disease outcome in primary breast cancer. Int J Cancer 1999;84:203–208.
Stendahl M, Ryden L, Nordenskjold B, et al. High progesterone receptor expression correlates to the effect of adjuvant tamoxifen in premenopausal breast cancer patients. Clin Cancer Res 2006;12:4614–4618.
Yamashita H, Yando Y, Nishio M, et al. Immunohistochemical evaluation of hormone receptor status for predicting response to endocrine therapy in metastatic breast cancer. Breast cancer 2006;13:74–83.
Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst 1998;90:1371–1388.
Mohsin SK, Weiss H, Havighurst T, et al. Progesterone receptor by immunohistochemistry and clinical outcome in breast cancer: a validation study. Mod Pathol 2004;17:1545–1554.
Ogawa Y, Moriya T, Kato Y, et al. Immunohistochemical assessment for estrogen receptor and progesterone receptor status in breast cancer: analysis for a cut-off point as the predictor for endocrine therapy. Breast cancer 2004;11:267–275.
Regan MM, Viale G, Mastropasqua MG, et al. Re-evaluating adjuvant breast cancer trials: assessing hormone receptor status by immunohistochemical versus extraction assays. J Natl Cancer Inst 2006;98:1571–1581.
Brock JE, Hornick JL, Richardson AL, et al. A comparison of estrogen receptor SP1 and 1D5 monoclonal antibodies in routine clinical use reveals similar staining results. Am J Clin Pathol 2009;132:396–401.
Cheang MC, Treaba DO, Speers CH, et al. Immunohistochemical detection using the new rabbit monoclonal antibody SP1 of estrogen receptor in breast cancer is superior to mouse monoclonal antibody 1D5 in predicting survival. J Clin Oncol 2006;24:5637–5644.
Qiu J, Kulkarni S, Chandrasekhar R, et al. Effect of delayed formalin fixation on estrogen and progesterone receptors in breast cancer: a study of three different clones. Am J Clin Pathol 2010;134:813–819.
Badve SS, Baehner FL, Gray RP, et al. Estrogen- and progesterone-receptor status in ECOG 2197: comparison of immunohistochemistry by local and central laboratories and quantitative reverse transcription polymerase chain reaction by central laboratory. J Clin Oncol 2008;26:2473–2481.
Douglas-Jones AG, Collett N, Morgan JM, et al. Comparison of core oestrogen receptor (ER) assay with excised tumour: intratumoral distribution of ER in breast carcinoma. J Clin Pathol 2001;54:951–955.
Dabbs DJ, Klein ME, Mohsin SK, et al. High false-negative rate of HER2 qRT-PCR of the Oncotype DX test: an independent quality assurance study. J Clin Oncol 2011;29:4279–4285.
Allison KH, Kandalaft PL, Sitlani CM, et al. Routine pathologic parameters can predict Oncotype DX(TM) recurrence scores in subsets of ER positive patients: who does not always need testing? Breast Cancer Res Treat 2011;131:413–424.
Tang P, Wang J, Hicks DG, et al. A lower Allred score for progesterone receptor is strongly associated with a higher recurrence score of 21-gene assay in breast cancer. Cancer Invest 2010;28:978–982.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kraus, J., Dabbs, D., Beriwal, S. et al. Semi-quantitative immunohistochemical assay versus oncotype DX® qRT-PCR assay for estrogen and progesterone receptors: an independent quality assurance study. Mod Pathol 25, 869–876 (2012). https://doi.org/10.1038/modpathol.2011.219
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2011.219
Keywords
This article is cited by
-
Impact of immunohistochemical expression of kinesin family member 18A (Kif18A) and β-catenin in infiltrating breast carcinoma of no special type
World Journal of Surgical Oncology (2024)
-
Concordance of the 21-gene assay between core needle biopsy and resection specimens in early breast cancer patients
Breast Cancer Research and Treatment (2021)
-
Prognostic significance of branched-chain amino acid transferase 1 and CD133 in triple-negative breast cancer
BMC Cancer (2020)
-
Principles and approaches for reproducible scoring of tissue stains in research
Laboratory Investigation (2018)
-
Prognostic significance of mucin expression profiles in breast carcinoma with signet ring cells: a clinicopathological study
Diagnostic Pathology (2016)