Abstract
The biology of breast carcinoma shows a great variation, reflected by the recent classification of phenotypes based on DNA microarrays or immunohistochemistry. The aim of this study was to determine the prevalence of insulin-like growth factor-1 receptor (IGF1R) in breast carcinoma subtypes and the impact on the outcome. We studied 197 consecutive breast carcinoma patients in stage I–II treated conservatively. Phenotypes were assessed on the basis of the expressions of ER/PR, HER2, Ki67, p53, Bcl2, CK5/6 and EGFR. Moreover, IGF1R expression (α-subunit and β-phosphorylated/active form) was evaluated by immunohistochemistry, IGF1R mRNA levels by quantitative RT-PCR and IGF1R mutations by direct DNA sequencing. Overall, 40% (78/197) of tumors were luminal A, 24% (48/197) luminal B, 19% (37/197) HER2-positive and 17% (34/197) basal/triple-negative. Luminal A tumors were predominantly of low grade, without necrosis, presenting in older patients as a ≤2-cm unilateral mass (all P≤0.046). α-IGF1R overexpression was observed more frequently in luminal A (49%) cases, followed by luminal B (20%), HER2-positive area under the curve (22%) and basal/triple-negative cases (9%) (P=0.01) with similar results for mRNA levels (53, 24, 13 and 10%, respectively) (P=0.038), but without differences for mutations (P=NS). High IGF1R mRNA correlated with poor patient survival among subtypes (P=0.004) (Kaplan–Meier; log-rank test). For overall survival, only histological grade and IGF1R mRNA emerged as significant predictors (P≤0.034; Cox regression). Increased IGF1R mRNA implies poorer patient prognosis among the different subtypes, and that may be associated with the lack of responsiveness to tamoxifen in cases with a positive hormone receptor status. Our results highlight the biological and clinical relevance of IGF1R in early breast carcinoma subtypes, and provide knowledge to assist in treatment decision.
Similar content being viewed by others
Main
The clinical classification of breast carcinoma mainly on the basis of morphology is limited at present. In fact, patients with the same diagnosis can have different clinical outcomes, and this has been recently highlighted by several gene-expression studies. The classification in four main molecular subtypes supports their distinct biology. Furthermore, this information enables clinicians to tailor individual treatments.1, 2 Nevertheless, there is a need to redefine their molecular characteristics as they are heterogeneous.3
In patients with early breast carcinoma treated conservatively, local recurrence occurs between 6 and 20%, which correlates with increased distant metastasis and shorter survival.4, 5, 6, 7, 8 Therefore, research of new factors to identify patients at higher risk is necessary. Besides, the impact of breast carcinoma subtypes on local or distant control has not been evaluated extensively.9, 10, 11, 12
Recent epidemiological and clinico-pathological data have supported the role of the insulin-like growth factor-1 (IGF1R) signaling system on tumor development and progression.13, 14, 15, 16, 17 In breast carcinoma, high levels of IGF1R have been detected in 30–82%,18, 19 but its prognostic value is controversial.20, 21, 22, 23, 24, 25, 26, 27 Emerging experimental and clinical data suggest that the IGF1R and ER/PR pathways are interactive.24 About two-third of breast carcinomas have an ER-positive status, but >50% of patients respond to anti-estrogen treatment that is related to PI3K/Akt signaling upregulation by ERα. The sustained activation/inactivation of the IGF1R, PI3K/Akt and ERK signaling pathways in which Bcl2 levels are relevant might also be responsible for the response.28 Furthermore, some studies suggest that IGF1R is an emerging therapeutic target in cancer.13, 29 The aim of our study was to determine the influence of IGF1R expression and gene status in immunophenotypes of early breast carcinoma.
Materials and methods
Case Retrieval
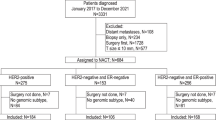
Patient characteristics have been described previously.30 Table 1 shows the distribution of tumors in relation to clinico-pathological features and immunophenotypes. In brief, a series of 197 lymph-node-negative breast carcinoma patients in the early stage (ie, stage I–II) treated with conserving surgery and radiation therapy were retrieved from the archives of the Department of Pathology at the University General Hospital of Alicante (January 1990–December 2001). All patients had undergone a complete gross excision of the primary tumor and axillary lymph-node dissection, with a minimum of five nodes removed. Our Institutional Review Board approved the study.
After surgery, radiation therapy of a total dose of 50 Gy to the tumor bed was given, including a boost (median 10 Gy). Patients with ER- and/or PR-positive tumors received tamoxifen for 2–5 years and those with high risk factors (such as young age, high grade or ER/PR-negative) were additionally treated with six cycles of cyclophosphamide, methotrexate and 5-fluoroucil chemotherapy or with four cycles of doxorubicin plus cyclophosphamide. None of the patients received taxanes, trastuzumab or aromatase inhibitors. Patients’ average age was 52 years (range 23–88 years) and the median follow-up was 124 months. There have been 33 (17%) in-breast relapses, including 7 with distant relapses as well, 20 (10%) with only distant relapses, 17 (9%) with contralateral breast carcinoma (1 synchronous and 16 metachronous) and 29 (15%) deaths.
Immunohistochemistry
Immunohistochemical staining was performed on paraffin-embedded tissues obtained from tissue microarrays using standard techniques, with antibodies and conditions detailed in Table 2. The staining was scored positive as follows: ER/PR ≥10%, Bcl2 ≥50%, p53 and Ki67 ≥20%, any degree for CK5/6 (cytoplasmic) or EGFR (membranous) and HER2 according to the scoring guidelines (>30% 3+). Both α- and β-phospho/active-IGF1R subunits (membrane and/or cytoplasm) were semi-quantitatively scored according to the percentage of positive cells and intensity (from 0 to 3+) (score 0–300).
In Situ Hybridization Analysis
HER2 gene status was confirmed by fluorescence in situ hybridization (FISH) (Dako pharmaDxTM) or chromogenic in situ hybridization (CISH) (Spot light; Zymed) in nondefinitive cases (2+ and <30% 3+ cells).31
Quantitative RT-PCR and DNA Sequencing
DNA isolation method, PCR conditions, primers, as well as mutational and quantitative analyses of IGF1R have been described previously.30 In brief, we extracted genomic DNA using the QIAmp DNA mini-kit, and isolated total RNA by handling the RNeasy formalin-fixed paraffin-embedded kit (Qiagen, Hilden, Germany) from 2–3 paraffin-embedded cylinders (1-mm thick) from preselected tumor areas with at least 30% tumor cell content. Areas of necrosis and hemorrhage were excluded. A total of 150 primary breast carcinomas had sufficient formalin-fixed paraffin-embedded tissue available for RNA extraction, with sufficient quantity and quality. These included 30 with local recurrence, 14 with distant metastasis and 106 without recurrence. RT-PCR was performed in 20 μl reaction volumes with random hexamer priming, 10 μl of extracted RNA using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems Inc., Santa Clara, CA, USA). TaqMan Gene-Expression Assays of IGF1R hCG1640727, β-glucuronidase (GUSB) hCG18478 and glyceraldehyde-3-phosphate dehydrogenase hCG2005673 were performed in the ABI Prism 7500 System (Applied Biosystems) in triplicate. RT minus controls and two commercial positive controls (total human and breast carcinoma RNA) were included. IGF1R quantification was normalized to GUSB, and the relative changes in gene expression were calculated by the ΔΔCT method.
Primer sets for exons 19 and 21 were obtained from RefSec DNA NM000875.2, designed using Primer3 (TIB Molbiol Syntheselabor, Berlin). PCR amplicons were double-strand sequenced using the ABI Prism BigDye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems) and the ABI Prism 310 automated sequencer.
Statistical Analysis
The χ2 or Fisher tests were used to determine the distribution of characteristics among the immunophenotypes; the nonparametric Spearman's correlation test was used to determine the relationship between the IGF1R protein and mRNA; and the Mann–Whitney or Kruskal–Wallis tests were used to determine the expressions’ differences between pathological features. Receiver operating characteristic curves and area under the curve were generated to determine a cutoff value of the IGF1R gene expression and the potential clinical utility to predict prognosis (recurrence and death). Kaplan–Meier survival plots and log-rank tests were performed for comparison of survival curves, and for multivariate analysis, the Cox proportional hazards model was applied. P-values <0.05 were considered statistically significant.
Results
Tumors were classified as luminal A (ER/PR ≥50% and Bcl2 ≥50%, p53 <20% or Ki67 <20%) in 40% (78/197) cases, as luminal B (ER and/or PR <50% and Bcl2 <50%, p53 ≥20% or Ki67 ≥20%) in 24% (48/197), as HER2-positive (≥30% 3+ or amplified by FISH or CISH) in 19% (37/197) and as basal/triple-negative (ER/PR/HER2-negative±CK5/6±EGFR) in 17% (34/197) cases. The luminal A subtype was more frequently present in older patients (43%) as a unilateral mass (42%) of ≤2 cm in size (44%), low grade (67%), without tumor necrosis (50%) and negative vascular invasion (40%) (Table 1). However, there were no statistically differences regarding immunophenotypes and local recurrence (13% for luminal A, 23% for luminal B, 22% for HER2 and 12% for basal/triple-negative tumors) or distant metastases (8% of luminal A, 8% of luminal B, 11% of HER2 and 18% of basal/triple-negative; P=NS). Interestingly, among HER2-positive patients, local recurrence was developed in none with PR-positive tumors, but in 60% of ER-positive/PR-negative tumors and in 40% of ER/PR-negative tumors (P=0.004).
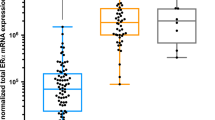
Table 1 summarizes the clinico-pathological features and IGF1R data in relation to immunophenotypes. Total IGF1R correlated with pospho-IGF1R (active) and IGF1R mRNA (Spearman's correlation coefficient: r=0.289, P=0.001; r=0.204, P=0.013, respectively). The median with percentiles 25 and 75 (P25–P75) for each analyzed factor is given in Table 3. For the purpose of the study, primary tumors were classified as having α- or pospho-IGF1R low vs high expression, defined using the median scores as cutoffs.24 A high expression of α-IGF1R (Figure 1a) was more frequently seen in luminal A (49%) cases, followed by HER2-positive (22%), luminal B (20%) and basal/triple-negative cases (9%) (P=0.01). Similarly, pospho-IGF1R (Figure 1b) was predominantly detected in luminal A (49%) cases, and to a lesser extent among HER2-positive (27%), luminal B (15%) and basal/triple-negative cases (9%) (P=0.047). The median relative IGF1R mRNA for all analyzed primary tumors (n=150) was 2.32 (P25–P75=1.23–3.91). Overall, 50% of tumors showed a ≥2-fold gene expression relative to the calibrator. Higher median levels were detected in luminal A, followed by luminal B and HER2 and basal/triple-negative (P<0.000; Kruskal–Wallis test). The cutoff points with the highest sensibility and specificity for defining high and low IGF1R mRNA were set at 2.50 and 2.61, respectively, derived from receiver operating characteristic curves to predict recurrence or death. The receiver operating characteristic curve to predict disease-free survival had an area under the curve (95% CI) of 0.58 (0.47–0.68) (P=0.14). The receiver operating characteristic curve to predict death had an area under the curve of 0.63 (0.52–0.75) (P=0.043). A direct correlation was found between the HR-positive status (77%) and increased expression of α-IGF1R (63%; P<0.001), mRNA (47%; P=0.001) or active IGF1R (64%; P=0.07).
Among the 85 tumors analyzed for IGF1R mutations in the β-subunit (TK domain at positions Tyr1131, Tyr1135 and Tyr1136; and C-terminal domain at positions Tyr1250 and Tyr1251), we only detected mutations in Tyr1131 (A3532G) in six primary tumors: three with local recurrence (one luminal B, one HER2 and one basal/triple-negative) and in three that did not recur (one luminal A, one HER2 and one basal/triple-negative).
Survival analyses showed shorter disease-free survival in patients with high-grade tumors (70 vs 90%; P=0.003) or vascular invasion present (70 vs 78%; P=0.056). Similarly, poorer overall survival was observed in patients with high-grade tumors (82 vs 100%; P=0.001) with vascular invasion (75 vs 91%; P=0.001), necrosis (74 vs 92%; P=0.001) or high content (cutoff ≥2.61) of IGF1R mRNA (90 vs 78%; P=0.048). However, no differences, neither for the IGF1R protein (total or active) nor for the mutation status, were found for disease-free and overall survival (P=NS) (Kaplan–Meier; log-rank test).
With regard to immunophenotypes, patients with luminal A tumors had a trend toward a better disease-free survival (81%) than did those with luminal B (69%), HER2-positive (68%) or basal/triple-negative tumors (71%) (P=0.06). Similarly, this was observed for overall survival, with 94% of patients with luminal A alive, 83% for luminal B, 78% for HER2-positive and 76% for those with basal/triple-negative tumors (P=0.05). Stratification of data according to IGF1R expression results, showed no significant correlation for disease-free survival neither with protein levels (total and active) nor with mRNA levels (P=NS). Nevertheless, patients whose tumors expressed ≥2.61-fold IGF1R mRNA had poorer overall survival among luminal A (100 vs 85%), luminal B (100 vs 72%) and basal/triple-negative groups (80 vs 50%), and similar for HER2 (73 vs 78%) (P=0.004). However, only a trend was found for active IGF1R results: luminal A (100 vs 88%), luminal B (100 vs 84%), basal/triple-negative groups (75 vs 50%) and HER2 (60 vs 82%) (P=0.12); and no significant associations were detected for α-IGF1R levels or mutation status (P=NS).
By multivariate analyses for disease-free survival, only histological grade (P=0.01) emerged as a significant predictor of relapse, with a trend for the presence of vascular invasion (P=0.12). With regard to overall survival, histological grade (P=0.03) and levels of IGF1R mRNA (P=0.01) showed an independent value, with a trend for vascular invasion (P=0.06) and subtype (P=0.15; Cox regression) (Table 4).
Discussion
The current research is focused on the comprehensive analysis of IGF1R, a potential therapeutic target gene that may help to identify patients at different risk of recurrence among early breast carcinoma subtypes. In these series, luminal A was the most frequent subtype, associated with good prognostic factors and patients’ outcome. In contrast, patients with basal/triple-negative tumors developed distant metastasis and therefore, poor prognosis, more frequently compared with previous reports.9 Nguyen et al10 in a series of breast carcinoma patients with similar characteristics also showed a low proportion of local recurrence in luminal A subtype (0.8%), but increased distant metastases in luminal B and basal subtypes. It is noteworthy that the high proportion of our patients with local failure (17%) might be attributed to longer follow-up (median 124 months). However, results of the more recently published series might not be comparable as several factors might have influenced the outcome, such as better preoperative breast imaging or more effective adjuvant local or systemic treatments. Moreover, it is unknown whether the differences seen in the recurrence rate of the HER2 group would have been observed if those patients had received trastuzumab.
IGF1R expression was detected in a higher proportion of luminal A tumors, followed by luminal B and HER2-positive tumors, with the lowest rate in basal/triple-negative, in line with previous investigators who reported co-expression of IGF1R and ER signaling systems.19, 24, 25, 32 The presence of IGF1R in tumors with higher content of ER/PR support the development of a subset of breast carcinoma subtypes along these two distinct pathways, mainly luminal A and B. It is plausible that together with microenvironment interactions and/or additional gene alterations, it might contribute to tumor heterogeneity.3 IGF1R overexpression is not a requirement for cellular transformation, but its presence even at low levels, is required for the activation of the main substrate IRS1, which in turn activates the PI3K and Shc/Ras/ERKs pathways.29
Our results partially agree with a recent immunohistochemical study.27 Their analysis of 226 breast carcinomas (181 luminal, 31 triple-negative and 14 HER2-positive) showed activated IGF1R regardless of the subtypes (luminal in 48.1%, triple-negative in 41.9% and HER2-positive in 64.3%), no correlation with ER status or activated Akt, but associated with poor prognosis, whereas total IGF1R was not. However, the clinical characteristics and treatment of their patients were not specified, which is difficult for comparison with our data as we included only lymph-node-negative breast carcinomas with conservative local treatment. It is interesting that our further analysis according to systemic therapy groups showed no differences regarding the total recurrence rate.30
Despite the significant correlations between the IGF1R protein and gene expression, we found that only increased IGF1R mRNA levels predicted poor survival. More interesting, however, were the survival results after stratification according to tumor subtypes and IGF1R mRNA expression, which showed ≥2.5-fold change in the different poor prognostic groups.
An association of IGF1R with less aggressive tumors and HR-positive status has been reported previously.20, 21, 22, 25, 32, 33 Anti-estrogens are clinically useful in the treatment of ER-positive breast carcinomas, and they have major effects on the IGF signaling pathways. On the other hand, IGFs exert powerful mitogenic effects in tamoxifen-responsive cells and act to support estrogen/ER-promoted growth. Owing to this close cross-talk, tamoxifen reduces IGF1R signaling at various levels as part of its response mechanisms.34 Nonetheless, emerging data suggest the role of the IGF1R network in resistance to endocrine therapy, but with contradictory results. Chan et al35 demonstrated in the rat mammary glands that tamoxifen-induced growth inhibition was associated with decreased basal phosphorylation of IGF1R, IRS1 and p85 subunit of PI3K. A novel experimental study in breast carcinoma cell lines has shown that the growth-inhibitory effect of anti-estrogens is due to the additional functional interactions with the PI3K/Akt and ERK pathways, as well as Bcl2.28 In contrast, Brockdorff et al36 found an association between anti-estrogen resistance and reduced α-IGF1R expression. Gee et al24 reported in a small (n=64) series of breast carcinomas that the α-IGF1R expression was higher in ER/PR-positive tumors and that those patients showed tamoxifen response (increased time to progression). In contrast, only our subgroup of patients with high IGF1R mRNA content tumors exhibit shorter survival, suggesting the potential relevance of increased IGF1R signaling in tamoxifen-resistance disease. Nevertheless, IGF1R may have some relevance in a subgroup of aggressive basal/triple-negative tumors.2, 37, 38
It is noteworthy that in this study, phenotypes have been only stratified according to immunohistochemical and in situ hybridization (for HER2 tumors) results. In addition, besides the HR-positive status, Bcl2, p53 and Ki67 data were taken into consideration for classifying tumors into luminal A or luminal B, based on the important role of apoptosis and proliferation-related genes emphasized in previous studies,39, 40, 41 and also supported by our study. Our approach to classify all positive cases independently of the ER/PR status as HER2 subtype has been reinforced by recent reports.12, 42
IGF1R mutations, present only in Tyr1131 (A3532G), were associated with neither tumors that recurred nor immunophenotypes, suggesting an unrelated gene event with a specific phenotype. Previous mutational analysis studies have shown that signals derived from both regions of the IGF1R cooperate to enhance tumor metastasis.15 Moreover, a relationship between local recurrence and radioresistance due to mutations at the C-terminal domain43 could not be confirmed in our former study.30 So far, no other previous investigators have analyzed the importance of IGF1R mRNA levels or IGF1R mutation status on breast carcinoma subtypes for a comparison with our data.
Histological grade and vascular invasion were associated with recurrence, with a trend for the breast carcinoma subtype. Our patients with longer survival also had low-grade tumors, absence of vascular invasion and necrosis, luminal A phenotype and low content of IGF1R mRNA. Nevertheless, only histological grade and IGF1R mRNA revealed an independent prognostic value. In contrast to previous studies, we found no negative impact of local recurrence on outcome.4, 6 Interestingly, Smid et al11 have evidenced the preference of breast carcinoma to relapse to specific organs, sharing biological features and pathways with their distant metastatic site.
The gene-expression signature has been suggested to be more powerful to predict local recurrence after conservative treatment,44 metastasis45 and tamoxifen response40 than standard clinical-pathological criteria. However, this technology is still impractical for the routine because of the time and expense required. As shown by previous investigators and us, biomarker expression by immunohistochemistry such as ER/PR, HER2, including Bcl2, Ki67 and p53, is a valid and readily available approach to stratify breast carcinoma in subtypes, which in turn proportion useful clinical information.10 Moreover, our study suggests that analysis of IGF1R may add predictive information regarding hormone therapy response and prognostic value among patients with breast carcinoma subtypes with a HR-positive status. This is of great interest as inhibition of IGF1R signaling using antibodies and small molecules is an emerging therapeutic strategy,27 also in combination with conventional chemotherapy, radiation therapy or co-targeting multiple pathways.13, 29
Finally, results from the Nurses’ Health Study suggest that increased expression of IGF1R in the cytoplasm of the benign ductal epithelium is correlated with the risk of breast carcinoma development.46 If this was supported in further studies, new clinical trials would eventually determine whether IGF1R inhibitors have a role not only in the treatment of breast carcinoma but also in its prevention.
In conclusion, luminal A is the most frequent subtype of breast carcinoma in patients in early stage, in association with low risk factors. The involvement of IGF1R in luminal A and B tumors, as well as in a subgroup of HER2/HR-positive tumors might be related on the one hand to a positive ER/PR cross-talk. On the other hand, its association with the lack of responsiveness to tamoxifen is supported by a poor patient outcome.
Our study highlights the clinical relevance of breast carcinoma subtype classification obtained using routine immunohistochemical methods, and IGF1R as a biomarker that adds prognostic information, which serves as a potential therapeutic target.
References
Perou CM, Sorlie T, Eisen MB, et al Molecular portraits of human breast tumours. Nature 2000;406:747–752.
Sorlie T, Tibshirani R, Parker J, et al Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 2003;100:8418–8423.
Stingl J, Caldas C . Molecular heterogeneity of breast carcinomas and the cancer stem cell hypothesis. Nat Rev Cancer 2007;7:791–799.
Clarke M, Collins R, Darby S, et al Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;366:2087–2106.
Early Breast Cancer Trialists’ Collaborative Group (EBCTCG). Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;365:1687–1717.
Livi L, Paiar F, Saieva C, et al Survival and breast relapse in 3834 patients with T1-T2 breast cancer after conserving surgery and adjuvant treatment. Radiother Oncol 2007;82:287–293.
Zhou P, Gautam S, Recht A . Factors affecting outcome for young women with early stage invasive breast cancer treated with breast-conserving therapy. Breast Cancer Res Treat 2007;101:51–57.
Punglia RS, Morrow M, Winer EP, et al Local therapy and survival in breast cancer. N Engl J Med 2007;356:2399–2405.
Haffty BG, Yang Q, Reiss M, et al Locoregional relapse and distant metastasis in conservatively managed triple negative early-stage breast cancer. J Clin Oncol 2006;24:5652–5657.
Nguyen PL, Taghian AG, Katz MS, et al Breast cancer subtype approximated by estrogen receptor, progesterone receptor, and HER-2 is associated with local and distant recurrence after breast-conserving therapy. J Clin Oncol 2008;26:2373–2378.
Smid M, Wang Y, Zhang Y, et al Subtypes of breast cancer show preferential site of relapse. Cancer Res 2008;68:3108–3114.
Parker JS, Mullins M, Cheang MC, et al Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol 2009;27:1160–1167.
Hewish M, Chau I, Cunningham D . Insulin-like growth factor 1 receptor targeted therapeutics: novel compounds and novel treatment strategies for cancer medicine. Recent Pat Anticancer Drug Discov 2009;4:54–72.
Brooks PC, Klemke RL, Schon S, et al Insulin-like growth factor receptor cooperates with integrin alpha v beta 5 to promote tumor cell dissemination in vivo. J Clin Invest 1997;99:1390–1398.
Brodt P, Fallavollita L, Khatib AM, et al Cooperative regulation of the invasive and metastatic phenotypes by different domains of the type I insulin-like growth factor receptor beta subunit. J Biol Chem 2001;276:33608–33615.
Chakravarti A, Loeffler JS, Dyson NJ . Insulin-like growth factor receptor I mediates resistance to anti-epidermal growth factor receptor therapy in primary human glioblastoma cells through continued activation of phosphoinositide 3-kinase signaling. Cancer Res 2002;62:200–207.
Ouban A, Muraca P, Yeatman T, et al Expression and distribution of insulin-like growth factor-1 receptor in human carcinomas. Hum Pathol 2003;34:803–808.
Al Sarakbi W, Chong Y, Williams S, et al The mRNA expression of IGF-1 and IGF-1R in human breast cancer: association with clinico-pathological parameters. J Carcinog 2006;5:16.
Chong YM, Colston K, Jiang WG, et al The relationship between the insulin-like growth factor-1 system and the oestrogen metabolising enzymes in breast cancer tissue and its adjacent non-cancerous tissue. Breast Cancer Res Treat 2006;99:275–288.
Papa V, Gliozzo B, Clark GM, et al Insulin-like growth factor-I receptors are overexpressed and predict a low risk in human breast cancer. Cancer Res 1993;53:3736–3740.
Schnarr B, Strunz K, Ohsam J, et al Down-regulation of insulin-like growth factor-I receptor and insulin receptor substrate-1 expression in advanced human breast cancer. Int J Cancer 2000;89:506–513.
Helle SI . The insulin-like growth factor system in advanced breast cancer. Best Pract Res Clin Endocrinol Metab 2004;18:67–79.
Shimizu C, Hasegawa T, Tani Y, et al Expression of insulin-like growth factor 1 receptor in primary breast cancer: immunohistochemical analysis. Hum Pathol 2004;35:1537–1542.
Gee JM, Robertson JF, Gutteridge E, et al Epidermal growth factor receptor/HER2/insulin-like growth factor receptor signalling and oestrogen receptor activity in clinical breast cancer. Endocr Relat Cancer 2005;12:S99–S111.
Ueda S, Tsuda H, Sato K, et al Alternative tyrosine phosphorylation of signaling kinases according to hormone receptor status in breast cancer overexpressing the insulin-like growth factor receptor type 1. Cancer Sci 2006;97:597–604.
Creighton CJ, Casa A, Lazard Z, et al Insulin-like growth factor-I activates gene transcription programs strongly associated with poor breast cancer prognosis. J Clin Oncol 2008;26:4078–4085.
Law JH, Habibi G, Hu K, et al Phosphorylated insulin-like growth factor-i/insulin receptor is present in all breast cancer subtypes and is related to poor survival. Cancer Res 2008;68:10238–10246.
Lam L, Hu X, Aktary Z, et al Tamoxifen and ICI 182,780 increase Bcl-2 levels and inhibit growth of breast carcinoma cells by modulating PI3K/AKT, ERK and IGF-1R pathways independent of ERalpha. Breast Cancer Res Treat 2009;118:605–621.
Baserga R . Customizing the targeting of IGF-1 receptor. Future Oncol 2009;5:43–50.
Peiro G, Benlloch S, Sanchez-Tejada L, et al Low activation of insulin-like growth factor 1-receptor (IGF1R) is associated with local recurrence in early breast carcinoma. Breast Cancer Res Treat 2009;117:433–441.
Peiro G, Aranda FI, Adrover E, et al Analysis of HER2 by chromogenic in situ hybridization and immunohistochemistry in lymph node-negative breast carcinoma: prognostic relevance. Hum Pathol 2007;38:26–34.
Surmacz E, Bartucci M . Role of estrogen receptor alpha in modulating IGF-I receptor signaling and function in breast cancer. J Exp Clin Cancer Res 2004;23:385–394.
Happerfield LC, Miles DW, Barnes DM, et al The localization of the insulin-like growth factor receptor 1 (IGFR-1) in benign and malignant breast tissue. J Pathol 1997;183:412–417.
Guvakova MA, Surmacz E . Tamoxifen interferes with the insulin-like growth factor I receptor (IGF-IR) signaling pathway in breast cancer cells. Cancer Res 1997;57:2606–2610.
Chan TW, Pollak M, Huynh H . Inhibition of insulin-like growth factor signaling pathways in mammary gland by pure antiestrogen ICI 182 780. Clin Cancer Res 2001;7:2545–2554.
Brockdorff BL, Heiberg I, Lykkesfeldt AE . Resistance to different antiestrogens is caused by different multi-factorial changes and is associated with reduced expression of IGF receptor Ialpha. Endocr Relat Cancer 2003;10:579–590.
Lerma E, Peiro G, Ramon T, et al Immunohistochemical heterogeneity of breast carcinomas negative for estrogen receptors, progesterone receptors and Her2/neu (basal-like breast carcinomas). Mod Pathol 2007;20:1200–1207.
Adelaide J, Finetti P, Bekhouche I, et al Integrated profiling of basal and luminal breast cancers. Cancer Res 2007;67:11565–11575.
van’t Veer LJ, Paik S, Hayes DF . Gene expression profiling of breast cancer: a new tumor marker. J Clin Oncol 2005;23:1631–1635.
Paik S, Tang G, Shak S, et al Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol 2006;24:3726–3734.
Loi S, Haibe-Kains B, Desmedt C, et al Definition of clinically distinct molecular subtypes in estrogen receptor-positive breast carcinomas through genomic grade. J Clin Oncol 2007;25:1239–1246.
Peiro G, Adrover E, Aranda FI, et al Prognostic implications of HER-2 status in steroid receptor-positive, lymph node-negative breast carcinoma. Am J Clin Pathol 2007;127:780–786.
Turner BC, Haffty BG, Narayanan L, et al Insulin-like growth factor-I receptor overexpression mediates cellular radioresistance and local breast cancer recurrence after lumpectomy and radiation. Cancer Res 1997;57:3079–3083.
Nuyten DS, Kreike B, Hart AA, et al Predicting a local recurrence after breast-conserving therapy by gene expression profiling. Breast Cancer Res 2006;8:R62.
Wang Y, Klijn JG, Zhang Y, et al Gene-expression profiles to predict distant metastasis of lymph-node-negative primary breast cancer. Lancet 2005;365:671–679.
Wang Y, Connolly JL, Hu R, et al Expression of insulin-like growth factor-i receptor (IGF-IR) in normal breast tissue and breast cancer risk: results from the Nurses’ Health Study. Mod Pathol 2009;22:73A.
Acknowledgements
We thank Patricia Picó and María D. Durán for their technical assistance; and Doreen Denecker for the preparation of this manuscript. This study was supported by the Fondo de Investigación Sanitaria (FIS 03/1411), Ministry of Health (Spain) and by the Fundación de la Comunidad Valenciana para la Investigación en el Hospital General Universitario de Alicante (FCVI-HGUA/2006). This study was presented in part at the 99th USCAP Meeting in Washington, March 2010.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Peiró, G., Adrover, E., Sánchez-Tejada, L. et al. Increased insulin-like growth factor-1 receptor mRNA expression predicts poor survival in immunophenotypes of early breast carcinoma. Mod Pathol 24, 201–208 (2011). https://doi.org/10.1038/modpathol.2010.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.191
Keywords
This article is cited by
-
Insulin-like growth factor receptor and sphingosine kinase are prognostic and therapeutic targets in breast cancer
BMC Cancer (2017)
-
CD44 induces FOXP3 expression and is related with favorable outcome in breast carcinoma
Virchows Archiv (2017)
-
The role of the insulin-like growth factor-1 system in breast cancer
Molecular Cancer (2015)
-
The dog as a naturally-occurring model for insulin-like growth factor type 1 receptor-overexpressing breast cancer: an observational cohort study
BMC Cancer (2015)
-
FOXA2 mRNA expression is associated with relapse in patients with Triple-Negative/Basal-like breast carcinoma
Breast Cancer Research and Treatment (2015)