Abstract
We herein describe three cases of pigmented villonodular synovitis with chondroid metaplasia. Two cases involved the temporomandibular joint, whereas the remaining one case occurred in the hip joint. Histologically, the tumors showed a villous pattern and were mainly composed of histiocyte-like cells and scattered osteoclast-like multinucleated giant cells, accompanied by chondroid areas with occasional lace-like calcification. These features resembled those of chondroblastoma of the bone, with the exception of the villous pattern. The histiocyte-like cells showed positive immunoreactivity for CD68, whereas they were negative for S-100 protein. Some of the previously reported cases of chondroblastoma in the temporal bone may have actually been cases of pigmented villonodular synovitis with chondroid metaplasia. When histologically chondroblastoma-like lesions involve the temporal bone or temporomandibular joint, the possibility of pigmented villonodular synovitis with chondroid metaplasia should also be considered, in addition to chondroblastoma of the bone. The correlation between this lesion and synovial chondromatosis remains uncertain.
Similar content being viewed by others
Main
Pigmented villonodular synovitis usually arises from the joint spaces in large joints, such as the knee or hip.1 Histologically, the lesion is characterized of the presence of a villous pattern, or a pseudoglandular or pseudoalveolar pattern.1, 2 The tumor is mainly composed of small or large histiocyte-like cells and osteoclast-like multinucleated giant cells. Recently, molecular genetic study demonstrated that only a minority of cells in pigmented villonodular synovitis are actually neoplastic cells and overexpress CFS1, which attract a secondary non-neoplastic population of histiocytes.3 Cartilaginous and osseous metaplasia is considered to be a rare phenomenon in pigmented villonodular synovitis. Only a single case report has been documented in detail concerning this rare type of tumor.4 Here, we report three cases of pigmented villonodular synovitis with extensive cartilaginous metaplasia and focal areas superficially resembling chondroblastoma of the bone. Two out of the three cases involved the temporomandibular joint and temporal bone, which is the most common site of skull chondroblastoma.
Materials and methods
The surgical specimens of all three cases were fixed in neutral buffered formalin. Hematoxylin and eosin staining and iron staining were performed in six (case 1), two (case 2) and six (case 3) formalin-fixed paraffin-embedded blocks. Immunohistochemical staining was performed in sections from a representative paraffin block from each case, using a streptavidin–biotin–peroxidase method (Histofine, Nichirei, Tokyo, Japan). The antibodies employed in this study are listed in Table 1. The Ki-67-labeling index (LI) was estimated by counting the number of positive cells per 1000 tumor cells.
Case Reports
Case 1
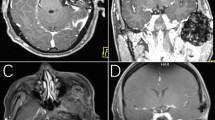
A 52-year-old man suffered from a 10-month history of tightness in his right ear. A mass lesion that protruded from the external auditory canal was discerned. CT scan revealed bone destruction of the right mandibular condyle and a soft-tissue mass measuring 2.0 × 1.8 cm with calcification, which had invaded the temporal bone and temporomandibular joint (Figure 1). After open biopsy, tumor resection was carried out. Follow-up magnetic resonance imaging (MRI) 11 months after surgery revealed no tumor recurrence.
Case 2
A 67-year-old man suffered from a 3-month history of pain in the left ear and swelling of the left cheek. MRI demonstrated a mass lesion, which was destroying the left temporal bone, involving the middle fossa and the temporomandibular joint. Angiography revealed a hypervascular mass. Following open biopsy, tumor resection was performed. Currently, the patient remains free of tumor recurrence 7 years and 3 months after the surgery.
Case 3
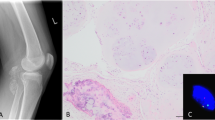
A 52-year-old woman complained of a 3-year history of right coxalgia. She had also noticed a mass lesion in her right groin about 6 months earlier. Plain radiography showed bone erosion in the right femoral neck. MRI revealed a tumor measuring 3.0 × 2.0 cm with fluid beneath the femoral neck, which showed low intensity on T1-weighted images (WI) and low intensity on T2-WI (Figure 2). The preoperative clinical diagnosis was pigmented villonodular synovitis and the patient underwent tumor resection. Postoperative imaging 2 years after the surgery revealed no recurrence.
Results
Macroscopic Findings
The tumors were resected piece by piece in cases 1 and 2. These lesions were described by the operating surgeons as comprising solid brownish or reddish-brown material. The periphery of the lesion was firm, whereas the central areas were friable. In case 3, the joint cavity was filled with bloody joint fluid and a tan to grayish tumor was observed. The cut surface of the resected tumor showed solid and whitish-gray cartilaginous areas with a gritty sensation, accompanied by villous configuration in part (Figure 2b).
Histopathological Findings
All the three cases had similar microscopic features and showed a characteristic villous pattern on low-power view (Figure 3a). In case 1, pseudoalveolar spaces were also encountered within the solid areas (Figure 3b). The tumor was mainly composed of a proliferation of rounded or polygonal mononuclear histiocyte-like cells with pale eosinophilic cytoplasm (Figure 3c). Some mononuclear cells had prominent eosinophilic cytoplasm and grooved nuclei, which mimicked chondroblasts. Mitotic figures were occasionally seen; however, no abnormal forms were detected. Aggregates of osteoclast-like multinucleated giant cells (Figure 3b) and hemosiderin deposits (Figure 3d) were also evident in all the three cases. Iron stain also confirmed the presence of abundant hemosiderin in all cases (Figure 3e). Another characteristic feature was the presence of hyaline chondroid nodules or lobules (Figure 3f and g). The cartilaginous component occupied approximately 20% of whole area in case 1, 30% in case 2 and 30% in case 3, respectively. Moreover, there were focal areas superficially resembling chondroblastoma. Dystrophic lace-like calcification, resembling so-called ‘chickenwire calcification’ of chondroblastoma, was focally observed in the chondroid areas in all three cases (Figure 3h). Enchondral ossification was also apparent in case 3 (Figure 3i). Secondary changes including reactive bone formation and a florid fibrohistiocytic proliferation were evident in case 1.
(a) Typical villous pattern (case 3). (b) Pseudoalveolar spaces with scattered osteoclast-like multinucleated giant cells (case 1). (c) Rounded or polygonal histiocyte-like mononuclear cells with eosinophilic cytoplasm (case 1). (d) Large-sized mononuclear histiocyte-like cells contain a peripheral rim of hemosiderin granules (case 2). (e) Iron stain discloses abundant hemosiderin (case 2). (f) Nodules of pink chondroid matrix are present between a proliferation of mononuclear histiocyte-like cells (case 1). (g) Lobular arrangement of hyaline cartilaginous tissue with mildly atypical chondrocytes (case 3). (h) Lace-like calcification between the mononuclear cells in the chondroid area (case 1). (i) Prominent enchondral ossification (case 3).
Immunohistochemical Findings
The immunohistochemical findings are summarized in Table 2. The histiocyte-like cells were positive for CD68 as well as osteoclast-like multinucleated giant cells in all cases (Figure 4a). The histiocyte-like cells also showed immunoreactivity for Factor XIIIa in cases 1 and 2. The mononuclear cells in the chondroid areas were uniformly positive for S-100 protein (Figure 4b), whereas none of the histiocyte-like cells showed any positive reaction. A minority of the histiocyte-like cells was positive for desmin in all cases, and positive for muscle-specific actin in cases 1 and 3. The mononuclear cells in both the histiocyte-like and chondroid areas were uniformly positive for vimentin. Concerning the proliferative activities, Ki-67-LIs in the histiocyte-like areas were between 5.7 and 8.7%, whereas those in the chondroid areas were less than 1%.
Discussion
Chondroid metaplasia is a rare phenomenon in tenosynovial giant cell tumors of both localized (giant cell tumor of tendon sheath) and diffused type (pigmented villonodular synovitis). Weiss and Goldblum2 stated that cartilaginous and osseous metaplasia is a rare focal finding in giant cell tumor of tendon sheath; however, no such description was observed in pigmented villonodular synovitis. In our three cases, cartilaginous metaplasia was extensively observed, in addition to the typical histological findings of pigmented villonodular synovitis. Until now, only a single such case report has been documented, and that concerned the elbow joint of a 54-year-old man. The tumor was classified as pigmented villonodular synovitis with a cartilaginous component by Pignatti et al.4
Histopathologically, our cases superficially mimicked chondroblastoma. Two of our three cases involved the temporomandibular joint and the temporal bone. The temporal bone or temporal fossa is one of the most common sites of chondroblastoma,5, 6 whereas pigmented villonodular synovitis of temporomandibular joint is not common.7 According to the large series of Kurt et al,5 23 out of 499 chondroblastomas (4.6%) arose in the temporal bone. Actually, our initial diagnosis of one case (case 1) was chondroblastoma. Brien et al8 described about their own 15 cases of giant cell tumor of tendon sheath or pigmented villonodular synovitis with extensive areas of chondroid and/or cartilage differentiation could not be distinguished from chondroblastoma of the bone by histologic or electron microscopic features alone. However, unfortunately they stated these comments in only discussion and their details have not been further documented.8 Reviewing the previously reported cases of temporal bone chondroblastoma, large tumors involved the surrounding soft tissue as well as the temporomandibular joint, suggesting pigmented villonodular synovitis by CT scan9 or MRI10 and these tumors histologically were found to contain prominent brown pigments in the mononuclear cells.9, 10, 11 Interestingly, the AFIP textbook states that some chondroblasts in the skull more commonly contain brown granular pigment in the cytoplasm, compared with other long bone cases.12 Moreover, histiocyte-like cells in pigmented villonodular synovitis also frequently display eosinophilic cytoplasm and longitudinal nuclear grooves,1 which are also the characteristic features of chondroblasts.6 Considering these reports, there is the possibility that some reported cases of temporal bone chondroblastoma may have actually been cases of pigmented villonodular synovitis with chondroid metaplasia.
Synovial chondromatosis is the other important differential diagnosis of the current cases. One of our cases (case 3) involved the hip joint, wherein synovial chondromatosis often occurs. Janssens et al13 found three cases of free osteochondroma with well-defined foci of metaplastic cartilage beneath the synovial lining cells, among their own seven cases of pigmented villonodular synovitis in the hip joint. They speculated that pigmented villonodular synovitis and synovial osteochondromatosis may occur simultaneously and may possibly be related entities reacting to a common etiologic factor. Furthermore, Pignatti et al4 also considered that their case of elbow pigmented villonodular synovitis with chondroid metaplasia had the possibility of being an intermediate form of pigmented villonodular synovitis associated with synovial chondromatosis. In our cases, no free osteochondral or cartilaginous nodules, as seen in typical synovial chondromatosis, were observed in the lesion. Therefore, we considered that the presence of cartilaginous tissue in the current cases was caused by chondroid metaplasia within the pigmented villonodular synovitis. However, the possibility that pigmented villonodular synovitis is actually a reactive synovial lesion to the primary synovial chondromatosis cannot be completely denied (Figure 5).
Tumoral calcium pyrophosphate dihydrate crystal deposition disease (tophaceous pseudogout) is also differential diagnosis of the current cases. It can also affects temporomandibular joint14, 15 and other atypical location.14 Tumoral calcium pyrophosphate dihydrate crystal deposition disease may be confused with pigmented villonodular synovitis with chondroid metaplasia, because it commonly shows foreign body granuloma reaction and metaplastic chondroid tissue.14 Tumoral calcium pyrophosphate dihydrate crystal deposition disease is characterized by the presence of small to large islands of intensely basophilic calcified crystalline material, which exhibit positive birefringence. In our cases, no such crystalloid material could be detected throughout the lesions.
Immunohistochemical studies were helpful to distinguish pigmented villonodular synovitis from chondroblastoma. Mononuclear histiocyte-like cells in all three cases showed immunoreactivity for CD68 and were negative for S-100 protein. In contrast, mononuclear cells in chondroblastoma are positive for S-100 protein,6, 12 whereas they are negative for CD68. In the current cases, mononuclear cells in morphologically distinct chondroid nodules were positive for S-100 protein.
In summary, we have described three cases of pigmented villonodular synovitis with chondroid metaplasia. Histologically, these lesions mimicked chondroblastoma. When similar lesions involve the temporal bone or temporomandibular joint, the possibility of pigmented villonodular synovitis with chondroid metaplasia, as well as chondroblastoma, should also be considered. As regards their relationship with synovial chondromatosis, further studies enabling the analysis of more cases are needed.
Conflict of interest
There are no conflicts on interest to disclose by any of the authors.
References
Somerhausen NS, Dal Cin P . Diffuse-type giant cell tumor. In: Fletcher CDM, Unni KK, Mertens F (eds). World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. International Agency for Research on Cancer Press: Lyon, 2002, pp 112–114.
Weiss SW, Goldblum JR . Tenosynovial giant cell tumor, localized type. In: Weiss SW, Goldblum JR (eds). Enzinger and Weiss's Soft Tissue Tumors, 4th edn. Mosby: St Louis, 2001, pp 1038–1047.
West RB, Rubin BP, Miller MA, et al. A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells. Proc Natl Acad Sci USA 2006;103:690–695.
Pignatti G, Mignani G, Bacchini P, et al. Case report 590: diffuse pigmented villonodular synovitis with a cartilaginous component. Skeletal Radiol 1990;19:65–67.
Kurt A-M, Unni KK, Sim FH, et al. Chondroblastoma of bone. Hum Pathol 1989;20:965–976.
Kilpatrick SE, Parisien M, Bridge JA . Chondroblastoma. In: Fletcher CDM, Unni KK, Mertens F (eds). World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. International Agency for Research on Cancer Press: Lyon, 2002, pp 241–242.
Aoyama S, Iwaki H, Amagasa T, et al. Pigmented villonodular synovitis of the temporomandibular joint: differential diagnosis and case report. Br J Oral Maxillofac Surg 2004;42:51–54.
Brien EW, Mirra JM, Ippolito V . Chondroblastoma arising from a nonepiphyseal site. Skeletal Radiol 1995;24:220–222.
Pontius A, Reder P, Ducic Y . Temporal bone chondroblastomas. Am J Otolaryngol 2003;24:370–373.
Cabrera RA, Almeida M, Mendonca ME, et al. Diagnostic pitfalls in fine needle aspiration cytology of temporomandibular chondroblastoma: report of two cases. Diagn Cytopathol 2006;34:424–429.
Bian LG, Sun QF, Zhao WG, et al. Temporal bone chondroblastoma; a review. Neuropathology 2005;25:159–164.
Unni KK, Inwards CY, Bridge JA, et al. AFIP Atlas of Tumor Pathology. Tumors of the Bones and Joint. American Registry of Pathology: Washington, DC, 2005, pp 61–67.
Janssens X, Veys EM, Cuvelier C . Pigmented villonodular synovitis of the hip—association with osteochondromatosis. Clin Exp Rheumatol 1987;5:329–334.
Ishida T, Dorfman HD, Bullough PG . Tophaceous pseudogout (tumoral calcium pyrophosphate dihydrate crystal deposition disease). Hum Pathol 1995;26:587–593.
Aoyama S, Kino K, Amagasa T, et al. Differential diagnosis of calcium pyrophosphate dihydrate deposition of the temporomandibular joint. Br J Oral maxillofac Surg 2000;38:550–553.
Acknowledgements
This study was supported in part by a Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (18590332), Tokyo, Japan. The English used in this manuscript was revised by Miss K Miller (Royal English Language Centre, Fukuoka, Japan).
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was presented in part at the Closed Meeting of the International Skeletal Society 2006, Vancouver, Canada, 11 September, 2006
Rights and permissions
About this article
Cite this article
Oda, Y., Izumi, T., Harimaya, K. et al. Pigmented villonodular synovitis with chondroid metaplasia, resembling chondroblastoma of the bone: a report of three cases. Mod Pathol 20, 545–551 (2007). https://doi.org/10.1038/modpathol.3800770
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800770
Keywords
This article is cited by
-
Pathology of intra-articular tumours and tumour-like lesions: pearls, pitfalls and rarities from a general surgical pathology practice
Skeletal Radiology (2024)
-
Calcified chondroid mesenchymal neoplasms with FN1-receptor tyrosine kinase gene fusions including FGFR2, FGFR1, MERTK, NTRK1, and TEK: a molecular and clinicopathologic analysis
Modern Pathology (2021)
-
Clinicopathologic characterization of malignant chondroblastoma: a neoplasm with locally aggressive behavior and metastatic potential that closely mimics chondroblastoma-like osteosarcoma
Modern Pathology (2020)
-
Soft Tissue Special Issue: Giant Cell-Rich Lesions of the Head and Neck Region
Head and Neck Pathology (2020)
-
Selected Giant Cell Rich Lesions of the Temporal Bone
Head and Neck Pathology (2018)