Abstract
Conflicting results on the prevalence of cyclin D1 ovexpression and its correlation with CCND1 amplification and outcome of breast cancer patients have been reported. Owing to limited sensitivity and specificity of most antibodies against cyclin D1, evaluation of cyclin D1 immunoexpression is reported to be problematic. The aims of this study were to assess the prevalence of cyclin D1 expression in breast carcinomas using the SP4 rabbit monoclonal antibody; to correlate cyclin D1 expression with amplification, assessed using chromogenic in situ hybridisation (CISH); and to analyse the relationship between CCND1 amplification and overexpression with clinicopathological parameters and outcome in a tissue microarray containing replicate tumour samples from 245 breast cancer patients. Immunohistochemistry for cyclin D1 was performed using the SP4 and the results were scored according to the Allred scoring system. CISH was carried out using the Zymed CCND1 SpotLight probe. CISH signals were counted in 60 morphologically unequivocal neoplastic cells. Amplification was defined as >5 signals per nucleus in more than 50% of cancer cells, or when large gene copy clusters were seen. Strong cyclin D1 expression and CCND1 amplification were found in 67.4 and 14.5% of the cases, respectively. A strong correlation between cyclin D1 overexpression and CCND1 amplification was demonstrated (P<0.0001). Cyclin D1 expression showed a positive correlation with hormone receptor expression (both ER and PgR, P<0.0001). An inverse correlation was observed between an immunohistochemical panel of ‘basal-like’ markers and both cyclin D1 overexpression (P<0.0001) and CCND1 amplification (P<0.0001). On univariate analysis cyclin D1 expression showed a correlation with longer overall survival (OS). Neither cyclin D1 nor CCND1 were independent prognostic factors for disease-free survival or OS. The results of this study confirm the association between cyclin D1 overexpression and positivity for hormone receptors and the lack of CCND1 amplification in basal-like breast carcinomas.
Similar content being viewed by others
Main
The CCND1 gene maps to 11q13 and encodes cyclin D1, the regulatory subunit of a holoenzyme that inactivates the retinoblastoma protein and promotes progression through the G1–S phase of the cell cycle.1, 2, 3, 4 Genetic abnormalities mapping to 11q13 are remarkably frequent in human neoplasms and particularly in breast cancer,5 where this region is predominantly gained/amplified in grade II breast carcinomas.6 CCND1 amplification has been extensively investigated in breast cancer by Southern blotting,7, 8, 9, 10 fluorescent in situ hybridisation (FISH)11, 12, 13, 14, 15 and real-time polymerase chain reaction-based methods,16 with the prevalence ranging from 9 to 24%.7, 8, 9, 10, 13, 14, 16, 17 Conflicting data on the associations between CCND1 amplification and clinicopathological variables and clinical outcome have been reported: while some have found an association between CCND1 amplification and positivity for oestrogen receptor (ER),7, 12, 17 lobular histology7 and poor outcome,7, 8, 16 others have failed to find some of these.10, 12, 18
Cyclin D1 overexpression is reported to be more prevalent than amplification, with the reported frequency ranging from 28 to 83%.1, 2, 11, 13, 14, 16, 19, 20, 21, 22, 23 This variation has been linked with different antibodies, techniques and thresholds (cutoff points). Cyclin D1 overexpression, with or without CCND1 amplification, has received great attention in the literature in the last three years due to results of in vitro studies and data from clinical trials implicating cyclin D1 overexpression in resistance to tamoxifen treatment.13, 14, 23
Given the crucial prognostic and predictive information that can be obtained by the analysis of CCND1 amplification and overexpression, reliable methods for quantification are required. Ideally, these should be applicable to a high throughput methodology such as tissue microarrays (TMAs). In a recent study, it was reported that 44% of TMA cores did not produce interpretable results when FISH probes for CCND1 were used.13 Chromogenic in situ hybridisation (CISH) is a suitable alternative for FISH and has proven reliable in the assessment of gene copy numbers in TMAs;24, 25, 26, 27 however, this technique has not been employed for the study of CCND1 amplification.
Immunohistochemical analysis of cyclin D1 expression is fraught with difficulties.28 Several authorities have reported that immunohistochemical assessment of cyclin D1 in pathology practice is difficult,28 erratic,28 ‘technically challenging’29 and ‘not routinely used because of the frequent demonstration of equivocal results’.30 However, recently, a new rabbit monoclonal antibody against cyclin D1 has been developed and provides results that are more consistent than those obtained with other antibodies.28
The aims of this study are fourfold: (i) to analyse the expression of cyclin D1 in breast carcinomas using the new rabbit monoclonal antibody anticyclin D1; (ii) to correlate cyclin D1 expression with gene amplification as defined by CISH; (iii) to analyse the correlations between CCND1 amplification and overexpression and the clinicopathological features and patients' outcome in a cohort of 245 patients with invasive breast carcinomas treated with surgery followed by anthracycline-based chemotherapy; and (iv) to define the prevalence of cyclin D1 overexpression and CCND1 amplification in ‘basal-like’ breast carcinomas.
Materials and methods
Tissue Microarrays
The TMA contained replicate 0.6 mm cores of 245 invasive breast carcinomas (185 invasive ductal carcinoma, 27 invasive lobular carcinomas, 25 invasive mixed carcinomas and eight invasive breast carcinomas of other special types). All patients were primarily treated with surgery (69 mastectomy and 155 wide local excision), anthracycline-based adjuvant chemotherapy, and hormone therapy for patients with ER-positive tumours. Follow-up was available for 244 patients, ranging from 0.5 to 125 months (median—67 months, mean—67 months). Full details of the characterisation of the TMA and the cohort of patients is described elsewhere.31 Tumours were graded according to a modified Bloom–Richardson scoring system32 and size was categorised according to the TNM staging criteria.33 This study was approved by the Royal Marsden Hospital Ethics Committee.
Immunohistochemistry
Immunohistochemistry for cyclin D1 was performed according to a previously described method,28 with the SP4 antibody (Neomarkers, Suffolk, UK) at a dilution of 1:50 and developed with the Envision kit (Dako, Glostrup, Denmark). The SP4 antibody is a rabbit monoclonal antibody raised against a synthetic peptide from C-terminus of human cyclin D1, which is deemed to be specific to cyclin D1, identifying a single 36 kDa band on Western blot analysis (http://www.neomarkers.com/AB.CFM?First=AntiBody&Second=9104). In addition, the SP4 clone is reported to be at least as specific as other monoclonal antibodies against cyclin D1, but is reported to be more sensitive than other clones.28, 34 Antigen retrieval was carried out by pressure cooking the sections for 2 min in EDTA solution, pH 8. Positive control (a translocation confirmed mantle cell lymphoma) and negative controls (omission of the primary antibody and IgG-matched immune serum) were included in each slide run. Cyclin D1 immunohistochemical intensity and distribution were semiquantitatively scored by two of the authors (KS and JSR-F) on a multiheaded microscope using the Allred score method.35 With this method, the intensity of the immunohistochemical reaction as viewed under the light microscope was recorded as 0, negative (no staining of any nuclei even at high magnification); 1, weak (only visible at high magnification); 2, moderate (readily visible at low magnification); or 3, strong (strikingly positive even at low power magnification). The proportion of tumour nuclei showing positive staining was also recorded as either: 0, none; 1, <1/100; 2, 1/100 to 1/10; 3, 1/10 to 1/3; 4, 1/3 to 2/3 and 5, >2/3. The proportion and intensity scores were then added to obtain a total score, which ranged from 0 to 8.35 Tumours were then categorised into four groups: negative/weak expression (total scores 0–2), intermediate expression (total scores 3–5) and strong expression (total scores 6–8). Only nuclear staining was considered specific. The analysis was performed blinded to the results of the CISH results and patients' outcome.
Ki-67 antigen (MIB1, 1:300, Dako, Glostrup, Denmark) and P53 (DO7, Dako, 1:200, Glostrup, Denmark) immunohistochemical detection was performed under the same conditions.31 MIB-1 staining was scored low if less than 10% of the nuclei of neoplastic cells were positive, intermediate if 10–30% of the nuclei of neoplastic cells were positive and high if more than 30% of the nuclei of neoplastic cells were positive. Tumours were scored positive for p53 if >10% of the nuclei of neoplastic cells showed definitive staining. The details of the immunohistochemical methods and scoring systems for ER, PgR, HER2, EGFR, Ck 14, Ck 5/6 and Ck 17 detection are described elsewhere.31 Based upon the expression of HER2, ER, Ck 5/6 and EGFR, tumours were classified according to the immunohistochemical panel proposed by Nielsen et al.36
Chromogenic In Situ Hybridisation
CISH for CCND1 was performed as previously described using the ready-to-use digoxigenin-labelled SpotLight cyclin D1 amplification probe (Zymed, South San Francisco, CA). Heat pretreatment of deparaffinised sections consisted of incubation for 15 min at 98°C in CISH pretreatment buffer (SPOT-light tissue pretreatment kit, Zymed) and digested with pepsin for 7 min at room temperature according to the manufacturer's instructions. An appropriate CCND1 gene-amplified breast tumour control was included in the slide run. CISH experiments were analysed by two of the authors (KS and JSR-F) on a multiheaded microscope. Only unequivocal signals were counted. Signals were evaluated at × 400 and × 630 magnification and 60 morphologically unequivocal neoplastic cells were counted for the presence of the gene probe signals. Amplification was defined as >5 signals per nucleus in more than 50% of cancer cells, or when large gene copy clusters were seen.25, 26, 27 The scoring was evaluated with observers blinded to the results of the immunohistochemical analysis and patients' outcome.
Statistical Analysis
The Statview software package was used for all calculations. Correlations between categorical variables were performed using the χ2-test and Fisher's exact test. Correlations between continuous and categorical variables were performed with analysis of variance (ANOVA). Disease-free survival (DFS) and overall survival (OS) were expressed as the number of months from diagnosis to the occurrence of an event (local recurrence/metastasis and disease-related death, respectively). Cumulative survival probabilities were calculated using the Kaplan–Meier method. Differences between survival rates were tested with the log-rank test. All tests were two-tailed, with a confidence interval of 95%.
Multivariate analysis was performed using the Cox multiple hazards model. A P-value of 0.05 in the univariate survival analysis was adopted as the limit for inclusion in the multivariate model, and cases with missing values were excluded from this analysis.
Results
Immunohistochemistry
The correlations between cyclin D1 expression and clinicopathological features and immunohistochemical findings in 245 breast carcinomas are summarised in Table 1. Briefly, 23 cores were either lost/fragmented in the immunohistochemical procedure or did not have invasive tumour. Out of the 224 remaining cores, 13 were scored as 0, 1 as 2, 12 as 3, 16 as 4, 31 as 5, 57 as 6, 59 as 7 and 35 as 8. When classified into negative/low, moderate or strong cyclin D1 expression groups, 26 were classified as low, 47 as intermediate and 151 as strong expressers (Figure 1). Cyclin D1 expression showed a strong direct correlation with expression of ER and PgR (both, P<0.0001) and an inverse correlation with the expression of basal markers (P<0.0001), including EGFR (P<0.0001), Ck 14 (P=0.0014), Ck 5/6 (P<0.0001) and Ck 17 (P<0.0001). Tumours with high levels of cyclin D1 expression less frequently showed p53 immunohistochemical expression (P<0.0001) and showed lower proliferation rates when compared to cyclin D1 low and moderate tumours (P<0.0001). When tumours were classified according to the immunohistochemical panel proposed by Nielsen et al,36 an inverse correlation between basal-like immunophenotype and cyclin D1 overexpression was found (P<0.0001).
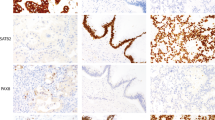
Grade III invasive ductal carcinoma (a) lacking cyclin D1 expression (b) and CCND1 gene amplification (c). Note the expression of cyclin D1 in inflammatory cells percolating the tumour. Grade I invasive ductal carcinoma (d) showing intermediate cyclin D1 expression (e) and no CCND1 amplification (f). Grade III invasive ductal carcinoma (g) displaying strong cyclin D1 (h) expression and lack of CCND1 gene amplification (i). EGFR- and basal keratin-negative grade II invasive ductal carcinoma (j) displaying strong cyclin D1 (k) expression and CCND1 gene amplification (l) in the form of multiple discrete signals and small clusters in the nuclei of neoplastic cells. EGFR- and basal keratin-negative grade II invasive mixed ductal-lobular carcinoma (m) showing strong cyclin D1 (n) expression and CCND1 gene amplification (o) in the form of large signal clusters in >50% of the neoplastic cells. In j and m, note the absence of morphological features of ‘basal-like carcinomas’ (ie, pushing borders, brisk lymphocytic infiltrate, geographic/central necrosis, spindle and squamous and/or cells) (a, b, d, e, g, h, j, k, m and n—original magnification × 200; c, f, i, l and o—original magnification × 400).
Chromogenic In Situ Hybridisation
The correlations between CCND1 amplification and clinicopathological features and immunohistochemical findings in 245 breast carcinomas are summarised in Table 2. Briefly, 39 cores were either lost/fragmented in the CISH procedure, did not have invasive tumour or showed suboptimal CCND1 signals. Out of the 206 remaining tumours, 30 showed either large clusters of CCND1 signals (Figure 1) or >5 individual signals/nucleus (Figure 1) in >50% of neoplastic cells. CCND1 amplification showed an inverse correlation with expression of EGFR (P=0.0488) and Ck 5/6 (P=0.0450). A trend for an inverse association with HER2 positivity (P=0.0578) and expression of Ck 14 (P=0.0813) was also observed. When tumours were classified according to the immunohistochemical panel proposed by Nielsen et al,36 an inverse correlation between basal-like immunophenotype and CCND1 amplification was found (P<0.0001). In fact, all basal-like carcinomas did not show CCND1 amplification.
Correlation between CCND1 Gene Amplification and Protein Overexpression
Data on CCND1 amplification and overexpression were available in 197 cases. A good correlation between CCND1 amplification and cyclin D1 overexpression was found (Table 3, P<0.0001). In fact, 29/30 tumours with CCND1 amplification showed strong cyclin D1 expression, whereas 1/30 showed moderate expression.
When data on the replicate cores of each tumour were treated independently, the agreement for cyclin D1 expression considering the categories negative/weak, intermediate and strong expression was good (unweighted kappa score=0.5787 (0.4678–0.6896)) and for CCND1 copy numbers (amplification vs no amplification) was excellent (unweighted kappa score=0.9351 (0.8618–1.0084)).
Survival Analysis
In this cohort, size, grade, lymph node metastasis, ER, PgR, Ck 17 and proliferation index assessed by MIB1 were statistically significant prognostic factors for DFS on univariate analysis (Table 4). Cyclin D1 overexpression showed a trend for a longer DFS in tumours with moderate and strong expression when compared to negative/low expression (Figure 2a, Table 4), whereas CCND1 amplification showed no correlation with DFS (Figure 2b, Table 4). On multivariate analysis, only size, grade and presence of lymph node metastasis were independent prognostic factors (data not shown).
Univariate survival analysis revealed lymph node metastasis, ER, PgR, Ck 14, Ck 5/6, Ck 17, p53, proliferation index as defined by MIB1, the immunophenotypic groups defined by the immunohistochemical panel described by Nielsen et al36 and cyclin D1 overexpression as prognostic factors for OS (Figure 2c, Table 4). CCND1 amplification failed to show any correlation with OS (Figure 2d, Table 4). Multivariate analysis revealed only the presence of lymph node metastasis, Ck 17 expression and p53 expression as independent prognostic factors for OS (data not shown).
Discussion
In order to develop immunohistochemical markers that can be utilised as prognostic and predictive factors in breast cancer, it is essential that reagents capable of producing reproducible results are used. Conflicting results on the prognostic impact of cyclin D1 overexpression and clinical outcome in breast cancer patients have been reported.1, 11, 16, 17, 18, 19, 20, 21, 37, 38, 39 Despite the known problems with commercially available anticyclin D1 antibodies, a considerable amount of data linking cyclin D1 overexpression with lack of response to tamoxifen have been published.13, 14
After several attempts at optimising mouse monoclonal and rabbit polyclonal antibodies to cyclin D1, we have attained reproducible results with the rabbit monoclonal antibody employing the protocol described by Cheuk et al.28 In contrast to other antibodies, the new rabbit anticyclin D1 monoclonal antibody shows a strong correlation with CCND1 gene amplification. However, in accordance with previous studies,1, 11, 13, 14, 16, 19, 20, 21 cyclin D1 overexpression was still more pervasive than gene amplification. In the present study, 67.4% of the cases showed strong cyclin D1 expression, whereas only 11.6% showed very low levels or no expression of this cell cycle regulator. This is not surprising, given that this protein plays a pivotal role in the progression from G1 to S phase2 and can be upregulated through several different pathways, including the ER, c-myc and fibroblast growth factor receptor pathways2, 3, 4, 40 (and references therein). In fact, the cell cycle effects of oestrogen are directly linked with upregulation of cyclin D1 overexpression.2 Although it is clear that ER-induced cyclin D1 expression is pivotal to induce cell cycle progression in oestrogen stimulated cells,2 CCND1 gene regulation by oestrogens appears complex, involving both primary and secondary events that have not yet been fully elucidated.41 CCND1 is a transcriptional target of ER41, 42, 43 and this process appears to be directly mediated through coordinate recruitment of specific ER coactivators2 and activation of IKKα44 and MAPK pathways.44 On the other hand, antioestrogens are reported to induce an acute downregulation of cyclin D1.2, 42 Cell line models have demonstrated that when cyclin D1 is inhibited by anticyclin D1 antibodies or by upregulation of p16INK4A oestrogen cannot induce G1–S phase progression.2, 45 Interestingly, cyclin D1 may also regulate ER pathway activity by physically interacting with ER and promoting ER pathway activation in a hormone-independent fashion.
The frequency of CCND1 amplifications as defined by CISH in the present study (14.6%) is similar to that reported in breast cancer using Southern blot7, 8, 9 or FISH.1, 10, 12, 13, 15, 19, 39 CISH has several major advantages,24 which are illustrated in this study; the whole analysis of the 245 replicate cores took less than a week, the neoplastic cells were easily recognisable and only 16% of the cores were not interpretable.
We have confirmed the strong association between cyclin D1 overexpression and positivity for hormone receptors1, 9, 10, 19, 21, 39 and have also found a strong inverse correlation with the expression of ‘basal-like’ markers (ie, EGFR, Ck 14, Ck 5/6 and Ck 17). Although we did not find a statistically significant association between CCND1 amplification and positivity for hormone receptors, CCND1 amplification showed an inverse correlation with tumours with basal-like immunophenotype (all cases with basal-like phenotype did not harbour CCND1 amplification). Therefore, our findings corroborate the results of Vaziri et al,46 who did not find CCND1 amplifications in BRCA1 mutation carriers; these tumours frequently harbour a basal-like phenotype40, 41 Taken together, these findings suggest that cyclin D1 is unlikely to play a role in the biology of ‘basal-like’ carcinomas. In fact, there are several lines of evidence to suggest that cyclin E rather than cyclin D1 would be more biologically significant for this aggressive subgroup of breast carcinomas.39, 47
In the present study, cyclin D1 overexpression as defined by the SP4 antibody was significantly correlated with OS. Patients whose tumours displayed strong and moderate cyclin D1 expression showed significantly longer OS than those with no or weak expression, which is in agreement with previous studies.1, 19, 37 However, others have found an association between cyclin D1 overexpression and poorer clinical outcome.23, 48 This discrepancy may stem from the use of different antibodies, different thresholds for Cyclin D1 positivity and different methods for the analysis of Cyclin D1 expression (Western blotting vs imunohistochemistry in the present study and others). Adopting thresholds of ≤10 and >90% as described by Stendahl et al,14 we observed that tumours with Cyclin D1 overexpression still showed a better OS compared to those devoid Cyclin D1 expression (Figures 2e). These differences in the prognostic impact of cyclin D1 may also be explained by the fact that all patients received anthracycline-based adjuvant chemotherapy in the present study. As for the prognostic impact of CCND1 amplification, our data are in agreement with the results of previous studies showing that CCND1 amplification is not associated with poor prognosis in a consecutive series of ER-positive and ER-negative breast cancers.12, 17
Based upon real-time polymerase chain reaction assessment of CCND1 gene copy numbers and cyclin D1 expression levels performed with nucleic acids obtained from nonmicrodissected breast tissue, Bieche et al16 have called into question the role of CCND1 as the amplicon driver on 11q13.16 Moreover, when Jirstrom et al13 compared CCND1 amplification and overexpression, these authors observed that approx 20% of the cases expressed low levels cyclin D1. One might argue that these results could be interpreted as evidence to suggest that CCND1 would not be the only amplicon driver of amplifications of 11q.16 Although up to four distinct amplicon cores have been described on 11q,49, 50 the probes used by Jirstrom et al13 specifically map to CCND1. Using an equally specific probe, we observed Cyclin D1 expression, either moderate or strong, in all cases with gene amplification. Given that the methods used by Bieche et al16 cannot differentiate between the expression of cyclin D1 in normal breast tissue and breast cancer cells and that the antibody used by Jirstrom et al13 is reported to have a limited sensitivity (approx 75%),28, 51, 52 our results would argue that CCND1 remains the likeliest candidate of the 11q13 amplicon core mapping to the 69 Mb region.38
In conclusion, this study confirms that the cyclin D1 SP4 rabbit monoclonal antibody is capable of producing reliable and reproducible results and that CISH is a remarkably reproducible and easily applied technique for assessing gene amplification. In addition, a strong correlation between cyclin D1 and CCND1 amplification has been demonstrated in this series of patients. Our data have shown a strong inverse correlation between immunohistochemical ‘basal-like’ markers and both cyclin D1 overexpression and CCND1 amplification. Furthermore, all ‘basal-like’ carcinomas as defined by the immunohistochemical panel proposed by Nielsen et al36 lacked CCND1 amplification, suggesting that this cell cycle regulator plays a limited role in the biology of ‘basal-like’ breast cancer.
References
Barnes DM . Cyclin D1 in mammary carcinoma. J Pathol 1997;181:267–269.
Butt AJ, McNeil CM, Musgrove EA, et al. Downstream targets of growth factor and oestrogen signalling and endocrine resistance: the potential roles of c-Myc, cyclin D1 and cyclin E. Endocr Relat Cancer 2005;12:S47–S59.
Arnold A, Papanikolaou A . Cyclin D1 in breast cancer pathogenesis. J Clin Oncol 2005;23:4215–4224.
Fu M, Wang C, Li Z, et al. Minireview: cyclin D1: normal and abnormal functions. Endocrinology 2004;145:5439–5447.
Reis-Filho JS, Simpson PT, Gale T, et al. The molecular genetics of breast cancer: the contribution of comparative genomic hybridization. Pathol Res Pract 2005;201:713–725.
Buerger H, Otterbach F, Simon R, et al. Different genetic pathways in the evolution of invasive breast cancer are associated with distinct morphological subtypes. J Pathol 1999;189:521–526.
Courjal F, Cuny M, Simony-Lafontaine J, et al. Mapping of DNA amplifications at 15 chromosomal localizations in 1875 breast tumors: definition of phenotypic groups. Cancer Res 1997;57:4360–4367.
Cuny M, Kramar A, Courjal F, et al. Relating genotype and phenotype in breast cancer: an analysis of the prognostic significance of amplification at eight different genes or loci and of p53 mutations. Cancer Res 2000;60:1077–1083.
Zukerberg LR, Yang WI, Gadd M, et al. Cyclin D1 (PRAD1) protein expression in breast cancer: approximately one-third of infiltrating mammary carcinomas show overexpression of the cyclin D1 oncogene. Mod Pathol 1995;8:560–567.
Barbareschi M, Pelosio P, Caffo O, et al. Cyclin-D1-gene amplification and expression in breast carcinoma: relation with clinicopathologic characteristics and with retinoblastoma gene product, p53 and p21WAF1 immunohistochemical expression. Int J Cancer 1997;74:171–174.
Gillett C, Fantl V, Smith R, et al. Amplification and overexpression of cyclin D1 in breast cancer detected by immunohistochemical staining. Cancer Res 1994;54:1812–1817.
Al-Kuraya K, Schraml P, Torhorst J, et al. Prognostic relevance of gene amplifications and coamplifications in breast cancer. Cancer Res 2004;64:8534–8540.
Jirstrom K, Stendahl M, Ryden L, et al. Adverse effect of adjuvant tamoxifen in premenopausal breast cancer with cyclin D1 gene amplification. Cancer Res 2005;65:8009–8016.
Stendahl M, Kronblad A, Ryden L, et al. Cyclin D1 overexpression is a negative predictive factor for tamoxifen response in postmenopausal breast cancer patients. Br J Cancer 2004;90:1942–1948.
Schraml P, Kononen J, Bubendorf L, et al. Tissue microarrays for gene amplification surveys in many different tumor types. Clin Cancer Res 1999;5:1966–1975.
Bieche I, Olivi M, Nogues C, et al. Prognostic value of CCND1 gene status in sporadic breast tumours, as determined by real-time quantitative PCR assays. Br J Cancer 2002;86:580–586.
Seshadri R, Lee CS, Hui R, et al. Cyclin DI amplification is not associated with reduced overall survival in primary breast cancer but may predict early relapse in patients with features of good prognosis. Clin Cancer Res 1996;2:1177–1184.
Naidu R, Wahab NA, Yadav MM, et al. Expression and amplification of cyclin D1 in primary breast carcinomas: relationship with histopathological types and clinico-pathological parameters. Oncol Rep 2002;9:409–416.
Pelosio P, Barbareschi M, Bonoldi E, et al. Clinical significance of cyclin D1 expression in patients with node-positive breast carcinoma treated with adjuvant therapy. Ann Oncol 1996;7:695–703.
McIntosh GG, Anderson JJ, Milton I, et al. Determination of the prognostic value of cyclin D1 overexpression in breast cancer. Oncogene 1995;11:885–891.
Takano Y, Takenaka H, Kato Y, et al. Cyclin D1 overexpression in invasive breast cancers: correlation with cyclin-dependent kinase 4 and oestrogen receptor overexpression, and lack of correlation with mitotic activity. J Cancer Res Clin Oncol 1999;125:505–512.
Geradts J, Ingram CD . Abnormal expression of cell cycle regulatory proteins in ductal and lobular carcinomas of the breast. Mod Pathol 2000;13:945–953.
Ahnstrom M, Nordenskjold B, Rutqvist LE, et al. Role of cyclin D1 in ErbB2-positive breast cancer and tamoxifen resistance. Breast Cancer Res Treat 2005;91:145–151.
Lambros MBK, Simpson PT, Jones C, et al. Unlocking pathology archives for molecular genetic studies: a reliable method to generate probes for chromogenic and fluorescent in situ hybridisation. Lab Invest 2006;86:398–408.
Reis-Filho JS, Simpson PT, Jones C, et al. Pleomorphic lobular carcinoma of the breast: role of comprehensive molecular pathology in characterization of an entity. J Pathol 2005;207:1–13.
Reis-Filho JS, Milanezi F, Carvalho S, et al. Metaplastic breast carcinomas exhibit EGFR, but not HER2, gene amplification and overexpression: immunohistochemical and chromogenic in situ hybridization analysis. Breast Cancer Res 2005;7:R1028–R1035.
Bhargava R, Gerald WL, Li AR, Pan Q, Lal P, Ladanyi M, Chen B . EGFR gene amplification in breast cancer: correlation with epidermal growth factor receptor mRNA and protein expression and HER-2 status and absence of EGFR-activating mutations. Mod Pathol 2005;18:1027–1033.
Cheuk W, Wong KO, Wong CS, et al. Consistent immunostaining for cyclin D1 can be achieved on a routine basis using a newly available rabbit monoclonal antibody. Am J Surg Pathol 2004;28:801–807.
Ioachim HL, Ratech H . Ioachim's Lymph Node Pathology. Lippincott Williams and Wilkins: Philadelphia, 2002.
Sun T, Nordberg ML, Cotelingam JD, et al. Fluorescence in situ hybridization: method of choice for a definitive diagnosis of mantle cell lymphoma. Am J Hematol 2003;74:78–84.
Reis-Filho JS, Steele D, Di Palma S, et al. Distribution and significance of nerve growth factor receptor (NGFR/p75(NTR)) in normal, benign and malignant breast tissue. Mod Pathol 2006;19:307–319.
Ellis IO, Galea M, Broughton N, et al. Pathological prognostic factors in breast cancer. II. Histological type. Relationship with survival in a large study with long-term follow-up. Histopathology 1992;20:479–489.
Singletary SE, Connolly JL . Breast cancer staging: working with the sixth edition of the AJCC cancer staging manual. CA Cancer J Clin 2006;56:37–47.
Rossi S, Laurino L, Furlanetto A, et al. Rabbit monoclonal antibodies: a comparative study between a novel category of immunoreagents and the corresponding mouse monoclonal antibodies. Am J Clin Pathol 2005;124:295–302.
Harvey JM, Clark GM, Osborne CK, et al. Estrogen receptor status by immunohistochemistry is superior to the ligand-binding assay for predicting response to adjuvant endocrine therapy in breast cancer. J Clin Oncol 1999;17:1474–1481.
Nielsen TO, Hsu FD, Jensen K, et al. Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 2004;10:5367–5374.
Hwang TS, Han HS, Hong YC, et al. Prognostic value of combined analysis of cyclin D1 and estrogen receptor status in breast cancer patients. Pathol Int 2003;53:74–80.
Peters G, Fantl V, Smith R, et al. Chromosome 11q13 markers and D-type cyclins in breast cancer. Breast Cancer Res Treat 1995;33:125–135.
Loden M, Stighall M, Nielsen NH, et al. The cyclin D1 high and cyclin E high subgroups of breast cancer: separate pathways in tumorogenesis based on pattern of genetic aberrations and inactivation of the pRb node. Oncogene 2002;21:4680–4690.
Koziczak M, Holbro T, Hynes NE . Blocking of FGFR signaling inhibits breast cancer cell proliferation through downregulation of D-type cyclins. Oncogene 2004;23:3501–3508.
Cicatiello L, Addeo R, Sasso A, et al. Estrogens and progesterone promote persistent CCND1 gene activation during G1 by inducing transcriptional derepression via c-Jun/c-Fos/estrogen receptor (progesterone receptor) complex assembly to a distal regulatory element and recruitment of cyclin D1 to its own gene promoter. Mol Cell Biol 2004;24:7260–7274.
Altucci L, Addeo R, Cicatiello L, et al. 17beta-Estradiol induces cyclin D1 gene transcription, p36D1-p34cdk4 complex activation and p105Rb phosphorylation during mitogenic stimulation of G(1)-arrested human breast cancer cells. Oncogene 1996;12:2315–2324.
Oh DS, Troester MA, Usary J, et al. Estrogen-regulated genes predict survival in hormone receptor-positive breast cancers. J Clin Oncol 2006;24:1656–1664.
Park KJ, Krishnan V, O'Malley BW, et al. Formation of an IKKalpha-dependent transcription complex is required for estrogen receptor-mediated gene activation. Mol Cell 2005;18:71–82.
Lukas J, Bartkova J, Bartek J . Convergence of mitogenic signalling cascades from diverse classes of receptors at the cyclin D-cyclin-dependent kinase-pRb-controlled G1 checkpoint. Mol Cell Biol 1996;16:6917–6925.
Vaziri SA, Tubbs RR, Darlington G, et al. Absence of CCND1 gene amplification in breast tumours of BRCA1 mutation carriers. Mol Pathol 2001;54:259–263.
Korsching E, Packeisen J, Agelopoulos K, et al. Cytogenetic alterations and cytokeratin expression patterns in breast cancer: integrating a new model of breast differentiation into cytogenetic pathways of breast carcinogenesis. Lab Invest 2002;82:1525–1533.
Kenny FS, Hui R, Musgrove EA, et al. Overexpression of cyclin D1 messenger RNA predicts for poor prognosis in estrogen receptor-positive breast cancer. Clin Cancer Res 1999;5:2069–2076.
Koreth J, Bakkenist CJ, McGee JO . Chromosomes, 11Q and cancer: a review. J Pathol 1999;187:28–38.
Janssen JW, Cuny M, Orsetti B, et al. MYEOV: a candidate gene for DNA amplification events occurring centromeric to CCND1 in breast cancer. Int J Cancer 2002;102:608–614.
Kodet R, Mrhalova M, Krskova L, et al. Mantle cell lymphoma: improved diagnostics using a combined approach of immunohistochemistry and identification of t(11;14)(q13;q32) by polymerase chain reaction and fluorescence in situ hybridization. Virchows Arch 2003;442:538–547.
Ott MM, Helbing A, Ott G, et al. bcl-1 rearrangement and cyclin D1 protein expression in mantle cell lymphoma. J Pathol 1996;179:238–242.
Acknowledgements
This study was funded by Breakthrough Breast Cancer. The authors are grateful to Professor Alan Ashworth for his invaluable comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reis-Filho, J., Savage, K., Lambros, M. et al. Cyclin D1 protein overexpression and CCND1 amplification in breast carcinomas: an immunohistochemical and chromogenic in situ hybridisation analysis. Mod Pathol 19, 999–1009 (2006). https://doi.org/10.1038/modpathol.3800621
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800621
Keywords
This article is cited by
-
Aberrant Cyclin D1 splicing in cancer: from molecular mechanism to therapeutic modulation
Cell Death & Disease (2023)
-
Impact of circulating miRNA-373 on breast cancer diagnosis through targeting VEGF and cyclin D1 genes
Journal of Genetic Engineering and Biotechnology (2021)
-
Prognostic Utility of Cyclin D1 in Invasive Breast Carcinoma
Indian Journal of Surgical Oncology (2019)
-
Expression of Cyclin D1 protein in residual tumor after neoadjuvant chemotherapy for breast cancer
Breast Cancer Research and Treatment (2018)
-
PIK3CA mutations are common in lobular carcinoma in situ, but are not a biomarker of progression
Breast Cancer Research (2017)