Abstract
The chemokine, CXCL12, and its receptor, CXCR4, have recently been shown to play an important role in metastasis of several kinds of carcinoma. It has also been demonstrated that VEGF regulates both the expression of CXCR4 and invasiveness in breast cancer cell lines. We compared the immunohistochemical expression of CXCR4 and VEGF between the primary site and a concordant pulmonary metastatic site in 30 osteosarcoma patients, all of which had undergone thoracotomy. Microvessel density (MVD) as shown by immunostaining of CD34 and proliferative activity with MIB-1 monoclonal antibody was also evaluated. CXCR4 expression (primary, 33.3% positive vs metastatic, 66.6% positive; P=0.0097) and MVD (primary, 29.86±6.87/0.26 mm2 vs metastatic, 43.32±8.65/0.26 mm2; P=0.0015) in the metastatic site were both significantly increased compared with those in the primary site, whereas no difference between primary and metastatic sites was observed with regard to VEGF expression. There was a significant positive correlation between immunohistochemical CXCR4 and VEGF expression (P=0.0269). In total population, the MIB-1-labeling index (LI) was significantly higher in tumors, which showed immunoreactivity for VEGF (MIB-1-LI in VEGF-positive tumors, 24.29±5.4 vs VEGF-negative tumors, 18.33±4.16; P=0.034). Furthermore, those patients with VEGF-positive primary tumors had a significantly worse prognosis compared with the patients with VEGF-negative primary tumors (P=0.0053). Our results suggested that CXCR4 expression was associated with metastatic progression, and immunohistochemical VEGF expression in the primary site had predictive value for the osteosarcoma patients, who developed lung metastasis.
Similar content being viewed by others
Main
It has been demonstrated that certain chemokines can serve as tissue-specific attractant molecules for tumor cells, promoting tumor cell migration to particular sites in vivo. Among chemokines and their receptors, the stromal cell-derived factor-1 (SDF-1/CXCL12)/CXCR4 system has been demonstrated to be involved in the lymph node metastasis or distant metastasis of several types of cancer.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12
Osteosarcoma is the most frequent primary bone tumor in young adults and adolescents. Despite recent advances in multimodality treatments consisting of adjuvant chemotherapy and surgical-wide resection, pulmonary metastasis occurs in approximately 40–50% of the patients.13 In such cases, the overall 5-year survival rate is only 28%, despite the multidisciplinary therapy.14 Involvement of the CXCR4/SDF-1 pathway in the metastatic process in the lung has also been demonstrated in osteosarcoma cell lines.15
Immunohistochemical VEGF expression in the untreated primary site has been reported to be correlated with pulmonary metastasis and microvessel density (MVD) in osteosarcoma.16 Wang et al17 showed poor prognosis in a group of patients with high MVD tumors, whereas Kreuter et al18 demonstrated that high MVD in the primary tumor was correlated with a good response to chemotherapy and a favorable prognosis in a group of systematically treated osteosarcoma patients. Although several authors have investigated the correlation between VEGF expression in the primary site and the development of metastasis in osteosarcoma,16, 19, 20 no studies have compared VEGF expression and MVD between primary and metastatic sites. Moreover, the expression of CXCR4 is unclear in clinical samples of malignant mesenchymal tumors as well as in osteosarcoma.
To elucidate the role of both VEGF expression and the CXCR4/SDF-1 pathway, we examined immunohistochemical VEGF and CXCR4 expression and MVD in both primary and pulmonary metastatic sites.
Materials and methods
Patients
In all, 30 patients underwent thoracotomy for pulmonary metastases of intramedullary conventional osteosarcoma at Kyushu University Hospital and the Kyushu National Medical Center, between 1974 and 2004. nm23 and c-MET expression in 24 out of the 30 patients has been published previously.21
Immunohistochemistry
Immunohistochemistry was performed on formalin-fixed tissue with or without decalcification taken from both the primary site and the concordant pulmonary metastatic site in each case. As for the primary site, one untreated open biopsy specimen from each case was used for immunohistochemical study. The cases with only needle biopsy in the primary site were excluded in this study because of its rather small amount of tumor. Concerning metastatic tumors, one representative section was selected in each case. Sections were cut at 4 μm thickness from paraffin-embedded material and then dewaxed with xylene and rehydrated through a graded series of ethanol. After inhibition of endogenous peroxidase, sections were exposed to the primary antibodies at 4°C overnight, followed by staining with a streptavidin–biotin–peroxidase kit (Nichirei, Tokyo, Japan). The sections were then finally reacted in 3,3′-diaminobenzidine, counterstained with hematoxylin and mounted. The following antibodies were used as the primary antibody: anti-CXCR4 (12G5, monoclonal, 1:100 (BD PharMingen, San Diego, CA, USA)), anti-VEGF (A-20, polyclonal 1:500 (Santa Cruz Biotechnology, Santa Cruz, CA, USA)), anti-CD34 (QBEnd/10, monoclonal 1:50 (Novocastra Laboratories, Newcastle, UK)) and anti-Ki-67 (MIB-1, monoclonal 1:100 (DAKO, Grostrup, Denmark)). For staining with all the antibodies, sections were pretreated with microwave irradiation in citrate buffer for the purpose of antigen retrieval. Sections from breast carcinoma specimens, which had resulted in lymph node metastasis was used as a positive control for CXCR4. The utility of all antibodies after decalcification was confirmed, using decalcified breast carcinoma specimen.
Evaluation
A consensus judgment was adopted as to the proper immunohistochemical score of the tumors based on the strength of CXCR4 and VEGF expression: 0=negative; 1+=weak staining; 2+=moderate staining; and 3+=strong staining. The distribution of positive cells was also recorded to impart the diffuse or focal nature of the positive cells: sporadic (positive cells <10%); focal (≥11% but less than 50%); and diffuse (positive cells ≥50%). The immunohistochemical scores of 2+ and 3+ with focal to diffuse distributions were considered to be positive for CXCR4 and VEGF antibodies. Two independent pathologists (YO and HY), who were not aware of the clinical characteristics of the patients, judged the immunoreactivity.
The degree of angiogenesis was determined by the number of microvessels in defined areas of the untreated biopsy specimen and concordant pulmonary metastatic specimen according to a slightly modified version of the method of Kaya et al.16 Two independent pathologists also estimated the microvessel count using microscopy. The number of CD34-positive vessels was counted in four selected hot spots in a × 400 field (0.26 mm2 field area). The mean value of the two independent readings of the same specimen was calculated, and MVD was defined as the mean count of microvessels per 0.26 mm2 field area.
The MIB-1-labeling index (LI) was estimated by counting the number of positive cells per 1000 tumor cells.
Statistical Analysis
Fisher's exact test was used to evaluate the association between two dichotomous variables. The difference in the MIB-1-LI or MVD between two groups was estimated by an unpooled t-test. The outcomes of different groups of patients were compared by the log-rank test. A P-value of less than 0.05 was considered statistically significant.
Results
Patient Characteristics
Their clinicopathological characteristics are summarized in Table 1. The patients comprised 18 males and 12 females, ranging in age from 7 to 69 years (median, 15.0 years). The anatomic distribution of the primary site was as follows: 15 in the distal femur, five in the proximal tibia, four in the femoral shaft, three in the proximal humerus and one each in the proximal femur, proximal fibula and iliac wing. Follow-up ranged from 9 to 145 months (median, 38.5 months). The primary lesions were treated with either amputation or limb salvage procedure in 29 extremity cases, whereas wide resection was performed in the iliac wing cases. Before the surgical procedure, preoperative chemotherapy was carried out in all cases. Lung metastases occurred from 2 to 72 months after the surgical procedure. Seven patients survived without disease for a period ranging from 39 to 145 months. A total of 23 patients either died of disease or currently remain alive with disease for a period ranging from 9 to 74 months. Histologically, the osteosarcoma lesions in the primary site comprised 25 osteoblastic type, two chondroblastic type, one malignant fibrous histiocytoma-like type, one small cell type and one fibroblastic type. According to the three-tiered grading system,22 all the lesions were classified as grade 3.
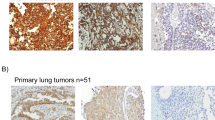
CXCR4 and VEGF Immunostaining
Immunohistochemical results of the distribution of cases in strength and positivity for CXCR4 and VEGF are summarized in Table 2 and 3. The expression of VEGF protein was seen in the cytoplasm of tumor cells and endothelium, whereas CXCR4 expression was recognized also in the nucleus as well as cytoplasm of tumor cells. In 10 out of 30 cases (33.3%), the primary tumor cells were positive for CXCR4, whereas in 20 cases (66.6%), the metastatic site showed positive immunoreactivity (Table 3 and Figure 1a–d). CXCR4 expression was significantly increased in the metastatic site, compared with the primary site (Table 2 and 3: P=0.0321 in strength, P=0.0097 in positivity). VEGF expression was observed in 19 out of 30 (63.3%) primary tumors, whereas 21 out of 30 cases (70%) showed positive reaction for VEGF in the metastatic sites (Table 2 and Figure 1e and f). There was no significant difference between primary and metastatic sites regarding the expression of VEGF. In the evaluation of both primary and metastatic sites together, of the 30 tumors, in which CXCR4 expression was recognized, 24 tumors (80%) showed positive immunoreaction for VEGF, and there was a significant correlation between CXCR4 and VEGF expression (P=0.0269). However, no significant relationship was observed between CXCR4 or VEGF expression and duration until lung metastasis or histological subtype.
Histology (a, c) and immunohistochemical CXCR4 expression (b, d) in primary osteoblastic osteosarcoma and its pulmonary metastasis (Case 24). The primary tumor is composed of a proliferation of atypical rounded or polygonal cells with fine lace-like osteoid. (a) It shows only focal and weak reaction for CXCR4 and is interpreted as negative (b). The metastatic tumor is made up of atypical large rounded cells with massive tumor osteoid (c) and reveals diffuse and strong cytoplasmic and nuclear immunoreactivity for CXCR4, judged as positive (d). (e and f) Immunostaining for VEGF in the primary site of osteoblastic osteosarcoma (e, Case 5; f, Case 16). No reaction products are detected in the primary tumor of the proximal humerus (e) and this patient remains free of disease 145 months after the initial surgery. Another primary tumor of the proximal tibia (f) shows diffuse positive reaction for VEGF and this patient died of disseminated disease 21 months after the initial surgery. (g and h) Immunohistochemical staining with CD34 for quantification of MVD in fibroblastic osteosarcoma and its metastatic site (Case 15). MVD in the metastatic site (h; 51/0.26 mm2) is higher than that in the primary site (g; 19/0.26 mm2).
CD34 Immunostaining and MVD
MVD assessed by immunohistochemical staining of CD34 ranged from 13.75 to 91.0/0.26 mm2 (36.59±8.45/0.26 mm2). MVD in the metastatic sites was significantly higher than that in the primary sites (metastatic site, 43.32±8.65; primary site, 29.86±6.87; P=0.0015; Table 3 and Figure 1g and h). There was no significant correlation between MVD and CXCR4 or VEGF expression. No correlation was detected between MVD and histologic type or duration until lung metastasis.
MIB-1-LI
MIB-1-LI ranged from 7.1 to 51.2 (22.3±5.18; Table 2). MIB-1 LI of VEGF-positive tumor in primary or metastatic site was higher, compared with negative tumors, although it did not show statistical significance (Table 4). However, in total population, MIB-1-LI of VEGF-positive tumors was significantly higher than that of VEGF-negative tumors (positive, 24.29±5.4; negative, 18.33±4.16; P=0.0346; Table 4). There was no correlation between MIB-1-LI and CXCR4 expression, MVD, histologic type or duration until lung metastasis.
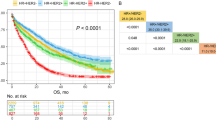
Survival Analysis
Patients with VEGF-positive tumors in the primary sites had a significantly shorter survival than those with VEGF-negative tumors (P=0.0053; Figures 1e, f and 2), whereas VEGF expression status in the metastatic sites did not affect the patient's prognosis. Moreover, CXCR4 expression nor MVD in either the primary or metastatic sites had any relationship with the survival of the patients.
Discussion
In this study, we compared CXCR4 expression between the primary site and the metastatic site in osteosarcoma and found that its expression is increased in the metastatic site. Müller et al1 showed that the chemokine receptor, CXCR4, is highly expressed in breast cancer tissue compared with normal mammary tissue and that its ligand CXCL12/SDF-1 is expressed in a variety of tissues including bone marrow, lymph nodes and the lung, sites to which breast cancer cells preferentially metastasize. Following their investigation, CXCR4 involvement in metastasis has been suggested in a variety of tumors and its expression in the primary site has been clinically correlated with poor survival or tumor progression in ovarian carcinoma,2 neuroblastoma,8 head and neck squamous cell carcinoma,10 colorectal carcinoma11 and urinary bladder cancer.12 However, no investigators have compared CXCR4 expression in the primary site with that in the concordant metastatic site, using a rather large series of clinical samples. Moreover, no studies have evaluated CXCR4 expression in human sarcoma. The current study was the first investigation to compare the expression of CXCR4 between primary and metastatic site in human malignancy and elucidated the involvement of CXCR4 expression in the metastatic process in osteosarcoma, one of the common sarcomas. However, the predictive value of CXCR4 expression for the patients' survival was not evident in osteosarcoma, in contrast with previously reported other human malignancies.
Perissinotto et al15 proved CXCR4/SDF-1 axis involvement in the metastatic process of osteosarcoma cells within a mouse model. Our immunohistochemical results and the experimental results of Perissinotto et al15 would seem to suggest that CXCR4 expression has an important role to play in the metastatic process in osteosarcoma. This study assessed only those cases where the patients developed lung metastasis. Therefore, the prognostic value of CXCR4 expression in the primary site of osteosarcoma needs to be elucidated, through analysis of a systematically treated large series of osteosarcoma.
Bachelder et al23 demonstrated that VEGF regulates CXCR4 expression in breast carcinoma cells. Moreover, they showed that CXCR4 mediates the migration of breast carcinoma cells toward to SDF-1, and that this migration is dependent on autocrine VEGF. In the current study, a significant correlation was found between VEGF and CXCR4 expression in the clinical samples of osteosarcoma.
VEGF has been identified as both a mitogen for endothelial cells in vitro and an angiogenesis-promoting factor in vivo.24, 25 Several studies have found a correlation between angiogenesis measured as MVD and distant metastasis or prognosis in malignant tumors. In osteosarcoma, some authors have investigated the correlation between MVD in the primary site and prognosis;17, 18 however, their results remain controversial. No investigators have compared MVD between the primary and the metastatic site in osteosarcoma. In the current study, MVD in the metastatic site was significantly higher than that in primary site. Some authors have shown a significant relationship between VEGF expression and MVD in osteosarcoma;16, 19 however, no such correlation was observed in the current study. All the patients in our study had developed lung metastasis, whereas other studies included both patients with metastatic tumors and those with nonmetastatic tumors.16, 19 Osteosarcoma with lung metastasis has been reported to show a higher expression of VEGF.16 This discrepancy between VEGF expression and MVD in our study may be owing to the inclusion of the patients with primary tumors with an initially higher VEGF expression, compared with patients included in other studies.
Kaya et al16 reported that VEGF expression in the untreated primary site of osteosarcoma is predictive for pulmonary metastasis and poor prognosis. Moreover, Lee et al19 demonstrated that the patients whose tumors showed the expression of VEGF165 had a worse prognosis than those without VEGF165 expression. The current study also revealed that VEGF expression in the primary site was an adverse prognostic factor in osteosarcoma, although all of the patients included in our study had in fact already developed lung metastasis. Moreover, VEFG-positive tumors showed a significantly higher MIB-1-LI, compared with VEGF-negative tumors. Considering our results and the results of previously reported studies,16, 19 VEGF expression may be one of the important molecules, which define biological behavior in osteosarcoma.
In conclusion, our results suggest that CXCR4 expression was involved in the metastatic process in osteosarcoma and that VEGF expression has an important role to play in biological aggressiveness in metastatic osteosarcoma. There is also the possibility that CXCR4 and VEGF antagonists may actually prevent distant metastasis and tumor progression in cases of osteosarcoma.
References
Müller A, Homey B, Soto H, et al. Involvement of chemokine receptors in breast cancer metastases. Nature 2001;410:50–56.
Scotton CJ, Wilson JL, Milliken D, et al. Epithelial cancer cell migration: a role for chemokine receptors? Cancer Res 2001;61:4961–4965.
Taichman RS, Cooper C, Keller ET, et al. Use of the stromal cell-derived factor-1/CXCR4 pathway in prostate cancer metastases to bone. Cancer Res 2002;62:1832–1837.
Schrader AJ, Lechner O, Templin M, et al. CXCR4/CXCL12 expression and signaling in kidney cancer. Br J Cancer 2002;86:1250–1256.
Shibuta K, Mori M, Shimoda K, et al. Regional expression of CXCL12/CXCR4 in liver and hepatocellular carcinoma and cell-cycle variation during in vitro differentiation. Jpn J Cancer Res 2002;93:789–797.
Delibasi CB, Okura M, Iida S, et al. Investigation of CXCR4 in squamous cell carcinoma of the tongue. Oral Oncol 2004;40:154–157.
Fernandis AZ, Prasad A, Band H, et al. Regulation of CXCR4-mediated chemotaxis and chemoinvasion of breast cancer cells. Oncogene 2004;23:157–167.
Russell HV, Hicks J, Okcu MF, et al. CXCR4 expression in neuroblastoma primary tumors is associated with clinical presentation of bone and bone marrow metastases. J Pediatr Surg 2004;10:1506–1511.
Uchida D, Begum N-M, Tomizuka Y, et al. Acquisition of lymph node, but not distant metastatic potentials, by the overexpression of CXCR4 in human oral squamous cell carcinoma. Lab Invest 2004;84:1538–1546.
Katayama A, Ogino T, Bandoh N, et al. Expression of CXCR4 and its down-regulation by IFN-gamma in head and neck squamous cell carcinoma. Clin Cancer Res 2005;11:2937–2946.
Kim J, Takeuchi H, Lam ST, et al. Chemokine receptor CXCR4 expression in colorectal cancer patients increases the risk for recurrence and for poor prognosis. J Clin Oncol 2005;23:2744–2753.
Retz MM, Sidhu SS, Blaveri E, et al. CXCR4 expression reflects tumor progression and regulates motility of bladder cancer cells. Int J Cancer 2005;114:182–189.
Wada T, Isu K, Takeda N, et al. A preliminary report of neoadjuvant chemotherapy NSH-7 study in osteosarcoma: preoperative salvage chemotherapy based on clinical tumor response and the use of granulocyte colony-stimulating factor. Oncology 1996;53:221–227.
Kempf-Bielack B, Bielack SS, Jurgens H, et al. Osteosarcoma relapse after combined modality therapy: an analysis of unselected patients in the Cooperative Osteosarcoma Study Group (COSS). J Clin Oncol 2005;23:559–568.
Perissinotto E, Cavalloni G, Leone F, et al. Involvement of chemokine receptor 4/stromal derived factor 1 system during osteosarcoma tumor progression. Clin Cancer Res 2005;11:490–497.
Kaya M, Wada T, Akatsuka T, et al. Vascular endothelial growth factor expression in untreated osteosarcoma is predictive of pulmonary metastasis and poor prognosis. Clin Cancer Res 2000;6:572–577.
Wang D, Chen L, Gao F . Correlation of tumor microvessel density with prognosis in osteogenic sarcoma. Chinese J Pathol 1997;26:266–269.
Kreuter M, Bieker R, Bielack SS, et al. Prognostic relevance of increased angiogenesis in osteosarcoma. Clin Cancer Res 2004;10:8531–8537.
Lee YH, Tokunaga T, Oshika Y, et al. Cell-retained isoforms of vascular endothelial growth factor (VEGF) are correlated with poor prognosis in osteosarcoma. Eur J Cancer 1999;35:1089–1093.
Kaya M, Wada T, Kawaguchi S, et al. Increased pre-therapeutic serum vascular endothelial growth factor in patients with early clinical relapse of osteosarcoma. Br J Cancer 2002;86:864–869.
Oda Y, Naka T, Takeshita M, et al. Comparison of histologic changes and changes in nm23 and c-MET expression between primary and metastatic sites in osteosarcoma. A clinicopathologic and immunohistochemical study. Hum Pathol 2000;31:709–716.
Dorfman HD, Vanel D, Czerniak B, et al. WHO classification of tumours of bone: Introduction. In: Fletcher CDM, Unni KK, Mertens F (eds). WHO Classification of Tumours: Pathology and Genetics: Tumours of Soft Tissue and Bone. IARC Press: Lyon, 2002, pp 227–232.
Bachelder RE, Wendt MA, Mercurio AM . Vascular endothelial growth factor promotes breast carcinoma invasion in an autocrine manner by regulating the chemokine receptor CXCR4. Cancer Res 2002;62:7203–7206.
Ferrara N, Henzel WJ . Pituitary follicular cells secrete a novel heparin-binding growth factor specific for vascular endothelial cells. Biochem Biophys Res Commun 1989;161:851–858.
Gospodarowicz D, Abraham JA, Schilling J . Isolation and characterization of a vascular endothelial cell mitogen produced by pituitary-derived folliculo stellate cells. Proc Natl Acad Sci USA 1989;86:7311–7315.
Acknowledgements
This work was supported in part by a Grant-in-Aid for Scientific Research from the Japan Society of the Promotion of Science (15590304), Tokyo, Japan. The English used in this manuscript was revised by Miss K Miller (Royal English Language Centre, Fukuoka, Japan).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oda, Y., Yamamoto, H., Tamiya, S. et al. CXCR4 and VEGF expression in the primary site and the metastatic site of human osteosarcoma: analysis within a group of patients, all of whom developed lung metastasis. Mod Pathol 19, 738–745 (2006). https://doi.org/10.1038/modpathol.3800587
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800587
Keywords
This article is cited by
-
Active targeting schemes for nano-drug delivery systems in osteosarcoma therapeutics
Journal of Nanobiotechnology (2023)
-
The role of vascular endothelial growth factor as a prognostic and clinicopathological marker in osteosarcoma: a systematic review and meta-analysis
Journal of Orthopaedic Surgery and Research (2021)
-
Caveolin-1 Expression Together with VEGF can be a Predictor for Lung Metastasis and Poor Prognosis in Osteosarcoma
Pathology & Oncology Research (2020)
-
The Tumor Microenvironment of Pediatric Sarcoma: Mesenchymal Mechanisms Regulating Cell Migration and Metastasis
Current Oncology Reports (2019)
-
Chemokines in homeostasis and diseases
Cellular & Molecular Immunology (2018)