Abstract
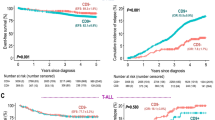
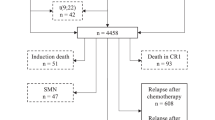
Minimal residual disease (MRD) quantified after induction treatment of childhood acute lymphoblastic leukemia (ALL) predicts risk of relapse. It has been assumed that early relapses derive from a residual population of leukemic cells, which is still present after induction and that relapsed disease will consequently be more resistant to treatment. To test these hypotheses, we performed a prospective study on patients treated according to the frontline-trial ALL-BFM 2000, which used MRD response for risk-group stratification. Patients (n=45) showed a median time to relapse of 1.5 years. In 89% of patients at least one T-cell-receptor/immunoglobulin gene rearrangement chosen for initial MRD quantification remained stable; however, at least one of the preferred markers for MRD stratification at relapse was different to diagnosis in 50% of patients. A similar proportion of very early, early and late relapses appeared to gain a marker at relapse although backtracking-analysis revealed that in 77% of cases, the gained markers were present as small sub-clones at initial diagnosis. Comparing initial and relapse MRD response to induction, 38% of patients showed a similar, 38% a better and 25% a poorer response after relapse. These data demonstrate an unexpectedly high clonal heterogeneity among very early/early relapses and challenge some current assumptions about relapsed ALL.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Eckert C, Biondi A, Seeger K, Cazzaniga G, Hartmann R, Beyermann B et al. Prognostic value of minimal residual disease in relapsed childhood acute lymphoblastic leukaemia. Lancet 2001; 358: 1239–1241.
van Dongen JJ, Seriu T, Panzer-Grumayer ER, Biondi A, Pongers-Willemse MJ, Corral L et al. Prognostic value of minimal residual disease in acute lymphoblastic leukaemia in childhood. Lancet 1998; 352: 1731–1738.
Flohr T, Schrauder A, Cazzaniga G, Panzer-Grumayer R, van der Velden V, Fischer S et al. Minimal residual disease-directed risk stratification using real-time quantitative PCR analysis of immunoglobulin and T-cell receptor gene rearrangements in the international multicenter trial AIEOP-BFM ALL 2000 for childhood acute lymphoblastic leukemia. Leukemia 2008; 22: 771–782.
Szczepanski T, Flohr T, van der Velden VH, Bartram CR, van Dongen JJ, Seriu T et al. Molecular monitoring of residual disease using antigen receptor genes in childhood acute lymphoblastic leukaemia. Best Pract Res Clin Haematol 2002; 15: 37–57.
Davi F, Gocke C, Smith S, Sklar J . Lymphocytic progenitor cell origin and clonal evolution of human B-lineage acute lymphoblastic leukemia. Blood 1996; 88: 609–621.
Li A, Zhou J, Zuckerman D, Rue M, Dalton V, Lyons C et al. Sequence analysis of clonal immunoglobulin and T-cell receptor gene rearrangements in children with acute lymphoblastic leukemia at diagnosis and at relapse: implications for pathogenesis and for the clinical utility of PCR-based methods of minimal residual disease detection. Blood 2003; 102: 4520–4526.
Peham M, Konrad M, Harbott J, Konig M, Haas OA, Panzer-Grumayer ER . Clonal variation of the immunogenotype in relapsed ETV6/RUNX1-positive acute lymphoblastic leukemia indicates subclone formation during early stages of leukemia development. Genes Chromosomes Cancer 2004; 39: 156–160.
Steenbergen EJ, Verhagen OJ, Nibbering CP, van den Berg H, van Leeuwen EF, Behrendt H et al. Clonal evolution of immunoglobulin heavy chain rearrangements in childhood B-precursor acute lymphoblastic leukemia after engraftment in SCID mice. Leukemia 1996; 10: 1471–1478.
Weston VJ, McConville CM, Mann JR, Darbyshire PJ, Lawson S, Gordon J et al. Molecular analysis of single colonies reveals a diverse origin of initial clonal proliferation in B-precursor acute lymphoblastic leukemia that can precede the t(12;21) translocation. Cancer Res 2001; 61: 8547–8553.
Wright JJ, Poplack DG, Bakhshi A, Reaman G, Cole D, Jensen JP et al. Gene rearrangements as markers of clonal variation and minimal residual disease in acute lymphoblastic leukemia. J Clin Oncol 1987; 5: 735–741.
Germano G, del Giudice L, Palatron S, Giarin E, Cazzaniga G, Biondi A et al. Clonality profile in relapsed precursor-B-ALL children by GeneScan and sequencing analyses. Consequences on minimal residual disease monitoring. Leukemia 2003; 17: 1573–1582.
Guggemos A, Eckert C, Szczepanski T, Hanel C, Taube T, van der Velden VH et al. Assessment of clonal stability of minimal residual disease targets between 1st and 2nd relapse of childhood precursor B-cell acute lymphoblastic leukemia. Haematologica 2003; 88: 736–746.
Stankovic T, Weston V, McConville CM, Green E, Powell JE, Mann JR et al. Clonal diversity of Ig and T-cell receptor gene rearrangements in childhood B-precursor acute lymphoblastic leukaemia. Leuk Lymphoma 2000; 36: 213–224.
Szczepanski T, van der Velden VH, Raff T, Jacobs DC, van Wering ER, Bruggemann M et al. Comparative analysis of T-cell receptor gene rearrangements at diagnosis and relapse of T-cell acute lymphoblastic leukemia (T-ALL) shows high stability of clonal markers for monitoring of minimal residual disease and reveals the occurrence of second T-ALL. Leukemia 2003; 17: 2149–2156.
Szczepanski T, Willemse MJ, Brinkhof B, van Wering ER, van der Burg M, van Dongen JJ . Comparative analysis of Ig and TCR gene rearrangements at diagnosis and at relapse of childhood precursor-B-ALL provides improved strategies for selection of stable PCR targets for monitoring of minimal residual disease. Blood 2002; 99: 2315–2323.
van der Velden VH, Bruggemann M, Hoogeveen PG, de Bie M, Hart PG, Raff T et al. TCRB gene rearrangements in childhood and adult precursor-B-ALL: frequency, applicability as MRD-PCR target, and stability between diagnosis and relapse. Leukemia 2004; 18: 1971–1980.
Choi S, Henderson MJ, Kwan E, Beesley AH, Sutton R, Bahar AY et al. Relapse in children with acute lymphoblastic leukaemia involving selection of a pre-existing drug resistant sub-clone. Blood 2007; 19: 19.
Konrad M, Metzler M, Panzer S, Ostreicher I, Peham M, Repp R et al. Late relapses evolve from slow-responding subclones in t(12;21)-positive acute lymphoblastic leukemia: evidence for the persistence of a preleukemic clone. Blood 2003; 101: 3635–3640.
Mullighan CG, Phillips LA, Su X, Ma J, Miller CB, Shurtleff SA et al. Genomic analysis of the clonal origins of relapsed acute lymphoblastic leukemia. Science 2008; 322: 1377–1380.
Ford AM, Fasching K, Panzer-Grumayer ER, Koenig M, Haas OA, Greaves MF . Origins of ‘late’ relapse in childhood acute lymphoblastic leukemia with TEL-AML1 fusion genes. Blood 2001; 98: 558–564.
Zuna J, Ford AM, Peham M, Patel N, Saha V, Eckert C et al. TEL deletion analysis supports a novel view of relapse in childhood acute lymphoblastic leukemia. Clin Cancer Res 2004; 10: 5355–5360.
Campana D . Molecular determinants of treatment response in acute lymphoblastic leukemia. Hematol Am Soc Hematol Educ Program 2008, 366–373.
Bailey LC, Lange BJ, Rheingold SR, Bunin NJ . Bone-marrow relapse in paediatric acute lymphoblastic leukaemia. Lancet Oncol 2008; 9: 873–883.
Henderson MJ, Choi S, Beesley AH, Sutton R, Venn NC, Marshall GM et al. Mechanism of relapse in pediatric acute lymphoblastic leukemia. Cell Cycle 2008; 7: 1315–1320.
Klumper E, Pieters R, Veerman AJ, Huismans DR, Loonen AH, Hahlen K et al. In vitro cellular drug resistance in children with relapsed/refractory acute lymphoblastic leukemia. Blood 1995; 86: 3861–3868.
Prokop A, Wieder T, Sturm I, Essmann F, Seeger K, Wuchter C et al. Relapse in childhood acute lymphoblastic leukemia is associated with a decrease of the Bax/Bcl-2 ratio and loss of spontaneous caspase-3 processing in vivo. Leukemia 2000; 14: 1606–1613.
Yang JJ, Bhojwani D, Yang W, Cai X, Stocco G, Crews K et al. Genome-wide copy number profiling reveals molecular evolution from diagnosis to relapse in childhood acute lymphoblastic leukemia. Blood 2008; 112: 4178–4183.
Hagedorn N, Acquaviva C, Fronkova E, von Stackelberg A, Barth A, zur Stadt U et al. Submicroscopic bone marrow involvement in isolated extramedullary relapses in childhood acute lymphoblastic leukemia: a more precise definition of ‘isolated’ and its possible clinical implications, a collaborative study of the Resistant Disease Committee of the International BFM study group. Blood 2007; 110: 4022–4029.
van der Velden VH, Panzer-Grumayer ER, Cazzaniga G, Flohr T, Sutton R, Schrauder A et al. Optimization of PCR-based minimal residual disease diagnostics for childhood acute lymphoblastic leukemia in a multi-center setting. Leukemia 2007; 21: 706–713.
Schrappe M . Risk-adapted stratification and treatment of childhood acute lymphoblastic leukaemia. Radiat Prot Dosimetry 2008; 132: 130–133.
Henze G, von Stackelberg A . Treatment of relapsed acute lymphoblastic leukemia. In: Pui CH (ed.). Treatment of Acute Leukemias New Directions for Clinical Research. Humana Press: Memphis, TN, 2002.
Pongers-Willemse MJ, Seriu T, Stolz F, d’Aniello E, Gameiro P, Pisa P et al. Primers and protocols for standardized detection of minimal residual disease in acute lymphoblastic leukemia using immunoglobulin and T cell receptor gene rearrangements and TAL1 deletions as PCR targets: report of the BIOMED-1 CONCERTED ACTION: investigation of minimal residual disease in acute leukemia. Leukemia 1999; 13: 110–118.
Szczepanski T, Pongers-Willemse MJ, Langerak AW, Harts WA, Wijkhuijs AJ, van Wering ER et al. Ig heavy chain gene rearrangements in T-cell acute lymphoblastic leukemia exhibit predominant DH6-19 and DH7-27 gene usage, can result in complete V-D-J rearrangements, and are rare in T-cell receptor alpha beta lineage. Blood 1999; 93: 4079–4085.
Szczepanski T, van der Velden VH, Hoogeveen PG, de Bie M, Jacobs DC, van Wering ER et al. Vdelta2-Jalpha rearrangements are frequent in precursor-B-acute lymphoblastic leukemia but rare in normal lymphoid cells. Blood 2004; 103: 3798–3804.
Taube T, Seeger K, Beyermann B, Hanel C, Duda S, Linderkamp C et al. Multiplex PCR for simultaneous detection of the most frequent T cell receptor-delta gene rearrangements in childhood ALL. Leukemia 1997; 11: 1978–1982.
Langerak AW, Szczepanski T, van der Burg M, Wolvers-Tettero IL, van Dongen JJ . Heteroduplex PCR analysis of rearranged T cell receptor genes for clonality assessment in suspect T cell proliferations. Leukemia 1997; 11: 2192–2199.
Eckert C, Landt O . Real-time PCR to detect minimal residual disease in childhood ALL. Methods Mol Med 2004; 91: 175–182.
van der Velden VH, Cazzaniga G, Schrauder A, Hancock J, Bader P, Panzer-Grumayer ER et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 2007; 21: 604–611.
Brisco MJ, Latham S, Sutton R, Hughes E, Wilczek V, van Zanten K et al. Determining the repertoire of IGH gene rearrangements to develop molecular markers for minimal residual disease in B-lineage acute lymphoblastic leukemia. J Mol Diagn 2009; 11: 194–200.
Greaves M . Cancer stem cells: back to Darwin? Semin Cancer Biol 2010; 20: 65–70.
Zuna J, Cave H, Eckert C, Szczepanski T, Meyer C, Mejstrikova E . et al. Childhood secondary ALL after ALL treatment. Leukemia 2007; 21: 1431–1435.
Bleyer WA . Biology and pathogenesis of CNS leukemia. Am J Pediatr Hematol Oncol 1989; 11: 57–63.
Meyer C, Kowarz E, Hofmann J, Renneville A, Zuna J, Trka J et al. New insights to the MLL recombinome of acute leukemias. Leukemia 2009; 23: 1490–1499.
von Goessel H, Jacobs U, Semper S, Krumbholz M, Langer T, Keller T et al. Cluster analysis of genomic ETV6-RUNX1 (TEL-AML1) fusion sites in childhood acute lymphoblastic leukemia. Leuk Res 2009; 33: 1082–1088.
Acknowledgements
We are grateful to NW, NP, CH, SH and WK for their excellent technical assistance. We thank the study documentation officers for the data management of the ALL-BFM trial (Kiel, Germany) and the ALL-REZ BFM trial (Berlin, Germany). We are very thankful to RS for her detailed reading, comments and suggestions for our manuscript. This work was kindly supported by the Deutsche José Carreras Leukämie-Stiftung e.V, by the Kompetenznetz für Pädiatrische Onkologie (BMBF), by the Deutsche Kinderkrebsstiftung and by the Deutsche Krebshilfe, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Leukemia website
Rights and permissions
About this article
Cite this article
Eckert, C., Flohr, T., Koehler, R. et al. Very early/early relapses of acute lymphoblastic leukemia show unexpected changes of clonal markers and high heterogeneity in response to initial and relapse treatment. Leukemia 25, 1305–1313 (2011). https://doi.org/10.1038/leu.2011.89
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2011.89
Keywords
This article is cited by
-
Integrated analysis of relapsed B-cell precursor Acute Lymphoblastic Leukemia identifies subtype-specific cytokine and metabolic signatures
Scientific Reports (2019)
-
Serum peptidome based biomarkers searching for monitoring minimal residual disease in adult acute lymphocytic leukemia
Proteome Science (2014)
-
Flow cytometry and IG/TCR quantitative PCR for minimal residual disease quantitation in acute lymphoblastic leukemia: a French multicenter prospective study on behalf of the FRALLE, EORTC and GRAALL
Leukemia (2013)