Abstract
The development of interstitial fibrosis occurs with aging. Impaired angiogenesis, associated with progressive loss of the renal microvasculature, is thought to be a cause of age-related nephropathy. However, the mechanism of capillary loss in aging kidney has not been fully elucidated. Angiostatin is a kringle-containing fragment of plasminogen and is a potent inhibitor of angiogenesis in vivo. Whether angiostatin generation is increased in the aging kidney has not been investigated. We examined 4, 10, 16, and 24-month-old Sprague-Dawley rats for angiostatin production and found that angiostatin generation was increased in aged rats. The protein expression and the activity of cathepsin D—the enzyme for angiostatin production—were increased in aged rats. In the aging kidney, nitric oxide (NO) availability is decreased. To investigate the role of NO in angiostatin production, human umbilical vein endothelial cells were treated with L-NG-nitroarginine methyl ester (L-NAME). L-NAME-treated cells showed increased cathepsin D activity and angiostatin production. For in vivo experiments, 16- to 18-month-old rats were treated with L-NAME or molsidomine for 3 months. Angiostatin production was increased in L-NAME-treated kidney, accompanied by increased cathepsin D activity. In contrast, angiostatin production was decreased in molsidomine-treated kidney, accompanied by decreased cathepsin D activity. In conclusion, angiostatin generation by cathepsin D was increased in the aging rat kidney. Decreased NO production activated cathepsin D activity. Increased angiostatin production may be related to capillary loss and interstitial damage in the aging rat kidney.
Similar content being viewed by others
Main
Aging is a risk factor for the progression of chronic kidney diseases.1 In addition, there is a progressive decrease in glomerular filtration rate with increasing age.2 Age-related vascular changes are linked to the decline in renal function observed with aging.2 Arteriosclerosis-related renal morphological changes, such as increased number of hyalinized glomeruli, decreased number of total glomeruli, tubulointerstitial fibrosis, and fibrous thickening of the vascular endothelium, are increased with aging. Multiple studies have shown peritubular capillary (PTC) loss in experimental and human progressive renal disease.3, 4, 5 The aging kidney also shows PTC loss accompanied by the development of interstitial fibrosis.6 Impaired angiogenesis, associated with progressive loss of the renal microvasculature, is thought to be a cause of age-related nephropathy.7 We have reported that altered expression of vascular endothelial growth factor is one of the causes of PTC loss in aged kidney.8 However, anti-angiogenic humoral factors synthesized in the aging kidney and which may compromise vessel integrity have not been fully elucidated.
Angiostatin is an endogenous angiogenesis inhibitor.9 It is a kringle-containing fragment of plasminogen, a potent inhibitor of angiogenesis in vivo, and it selectively inhibits endothelial cell proliferation and migration in vitro.10 It has been reported that renal angiostatin generation is increased along with activation of matrix metalloproteinase (MMP)-2 and MMP-9 after ischemia-reperfusion injury and may modulate renal capillary density.11 In the kidney of streptozotocin-treated diabetic rats, the angiostatin level is decreased, with decreased expression and proteolytic activity of MMP-2, which may contribute to the pathological changes of diabetic nephropathy.12 These reports indicate that angiostatin acts as an anti-angiogenic factor or pro-fibrotic factor in kidney diseases. However, the expression levels or the function of angiostatin in the aging kidney has not been studied previously.
Nitric oxide (NO) is one of the main factors involved in the angiogenic effects of the endothelium.13, 14 NO production is impaired not only in chronic kidney disease15 but also in the aging kidney16 coinciding with the progression of renal injury and decreased renal plasma flow.17, 18 NO has been reported to mediate downregulation of the anti-angiogenic factor thrombospondin-1.19 NO also has been reported to mediate angiostatin production.20 Matsunaga et al reported that inhibition of NO production increased the levels of angiostatin. Therefore, decreased NO production in aged kidney may increase angiostatin production. We hypothesized that NO deficiency in the aging kidney increases angiostatin production, which in turn causes tubular damage. To investigate whether angiostatin is increased with aging, we examined the kidney in rats of four age groups (4, 10, 16, and 24 months). To elucidate the effect of NO on angiostatin production, we treated 16- to 18-month-old rats with the potent inhibitor of NO synthase, L-NG-nitroarginine methyl ester (L-NAME), or the long-lasting NO-releasing vasodilator, molsidomine, and examined angiostatin production and tubular injury.
MATERIALS AND METHODS
Materials
Sprague-Dawley rats were purchased from Charles River Japan (Kanagawa, Japan). Anti-angiostatin antibody was from R&D Systems (BAF226; Minneapolis, MN, USA) and anti-cathepsin D antibody was from Santa Cruz Biotechnology (sc-10725; Santa Cruz, CA, USA). Antibody against rat endothelial cell antigen 1 (RECA-1; MCA970GA) was from AbD Serotec MorphoSys (Oxford, UK). Anti-Tie2, anti-matrix metalloproteinase (MMP)-2, and anti-MMP-9 antibody was from Abcam (ab71712, ab3158, and ab58803; Cambridge, MA, USA). L-NAME (N5751), molsidomine (M2901), bovine cathepsin D (C3138), plasminogen (P7397), pepstatin A (P4265), and a fluorimetric cathepsin D assay kit (CS0800) were from Sigma-Aldrich (St Louis, MO, USA). The NO colorimetric assay kit was from Enzo Life Science (ADI-917-010; Farmingdale, NY, USA). Amersham ECL Plus Western Blotting Detection Reagents and Amersham Hyperfilm ECL were from GE Healthcare Japan (Tokyo, Japan). Primers for quantitative real-time PCR and TaqMan probes for real-time PCR were from Sigma-Genosys (Hokkaido, Japan). Real-time PCR reagents were from Takara Bio (Otsu, Shiga, Japan). Human umbilical vein endothelial cells (HUVECs), culture medium (endothelial basal medium 2 (EBM-2)), and the additional factor set (endothelial growth medium-2 (EGM-2) SingleQuots) were from Clonetics (San Diego, CA, USA). Gibco Medium 199 (M199) was from Life Technologies Japan (Tokyo, Japan). Other reagents were locally available and of analytic grade.
In Vivo Experimental Protocol 1
Male Sprague-Dawley rats of four age groups (4 months, n=8; 10 months, n=8; 16 months, n=8; and 24 months, n=6) were individually housed under controlled temperature and humidity conditions with a 12-h light/dark cycle and free access to water. The experimental protocol (no. 06-029, 08-005) was approved by the Animal Research Committee of Kawasaki Medical School, and this study was conducted according to the Guide for the Care and Use of Laboratory Animals of Kawasaki Medical School, based on the National Institutes of Health Guide for the Care and Use of Laboratory Animals (NIH publication no. 80–23, revised 1996). One week before tissue harvesting, body weight was recorded, and blood pressure was measured by the tail-cuff method with an automatic sphygmomanometer (BP98A; Softron, Tokyo, Japan), and rats in each age group were placed in metabolic cages for 24 h to collect urine. All rats were anesthetized with pentobarbital (50 mg/kg, intraperitoneal) and sevoflurane (5%, inhalation), blood was collected via cardiac puncture, and the kidneys were removed via a midperitoneal incision. Half of each left kidney was cut in cross-section and fixed in 4% paraformaldehyde, and the remaining half of each left kidney was used for the preparation of unfixed cryostat sections. A sample of cortical tissue from each right kidney was snap frozen in liquid nitrogen and stored at −80 °C for subsequent RNA and protein assays. Serum creatinine and urinary protein levels were measured by SRL (Tokyo, Japan).
In Vivo Experimental Protocol 2
Male Sprague-Dawley rats (16–18 months old) were randomly assigned to one of three experimental groups: control (n=6); 20 mg/l L-NAME in drinking water (n=6); or 120 mg/l molsidomine in drinking water (n=6). The dosage of L-NAME and molsidomine were referred previous report.21 All treatments were continued for 3 months. Two rats from the control group and one from the L-NAME group died during the treatment period. After body weight and blood pressure measurement, rats were placed in metabolic cages, and urine was collected for 24 h. Urinary NO metabolites were measured with an enzyme-linked immunosorbent assay kit, according to the manufacturer’s instructions (Enzo Life Science). Kidney samples were obtained as described for experimental protocol 1.
Cell Culture
HUVECs (passages three to six) were cultured in EBM-2 containing 10% fetal bovine serum with additional factor EGM-2 SingleQuots. After starvation with 0.5% fetal bovine serum for 24 h, L-NAME (1.0 or 5.0 mM) was added to the culture medium for 24 h. Then, the expression and activity of cathepsin D, MMP-2, and MMP-9 were measured. In another experiment, after treatment with L-NAME, the medium was changed to acidic M199 medium (pH. 4.0). After 1 h, human plasminogen (4 μg/ml) was added, and cells were incubated for 1 h. The medium was collected, and western blot analysis was performed for angiostatin. Pepstatin A (200 μmol/l) was used as a cathepsin D inhibitor. Bovine cathepsin D (500 ng/ml) was used as the positive control.
Histological Assessment
Kidney sections (4 μm thick) were stained with Masson trichrome stain and were photographed under a microscope (Eclipse E800; Nikon, Tokyo, Japan). Images were digitized to 1372- to 1024-pixel color scale images with a software program (ACT-1C DXM 1200C; Nikon). Histological scores were assessed with a Coolscope (Nikon). Three nephrologists semiquantitatively analyzed Masson trichrome-stained sections in a blind manner. Tubulointerstitial injury was graded according to the extent of tubular and interstitial damage per field compared with areas of normal architecture as follows: 0=no change; 1=<25%; 2=25%–50%; 3=50%–75%; and 4=75%–100%. At least 20 fields at × 100 magnification were randomly selected from each rat, and the mean score was calculated.
Immunohistochemistry
Cryostat sections (4 μm thickness) were used for immunohistochemical studies of RECA-1. Anti-RECA-1 antibodies were applied to renal sections overnight at 4 °C. Antibody binding was detected with fluorescein-labeled secondary antibody (Sigma-Aldrich Japan, Tokyo, Japan). For evaluation of RECA-positive areas, percent positive area was measured with a color image analyzer (WinLoof; Mitani Co., Fukui, Japan). Twenty consecutive fields from each kidney were evaluated randomly at × 100 magnification, and the mean score was calculated.
Western Blot
Extraction of total cellular protein was performed in extraction reagent (T-PER Tissue Protein Extraction Reagent, Thermo Fisher Scientific, Rockford, IL, USA), according to the manufacturer’s instructions, and SDS-polyacrylamide gel electrophoresis was performed (50 μg protein/lane). Anti-angiostatin antibody, anti-Tie2 antibody, anti-MMP-2 antibody, anti-MMP-9 antibody, and anti-cathepsin D antibody were used as primary antibodies. Coomassie Brilliant Blue staining of the membrane confirmed equal loading and transfer. Signals were detected with the ECL system. Relative optical densities of the bands were quantified with Image J software version 1.42 (Available at: http://rsbweb.nih.gov/ij/. Accessed January 2012).
Quantitative Real-Time PCR
Total RNA extraction from kidney samples, reverse transcriptase reaction, and real-time quantitative PCR were performed as described previously.8 Primers and probes used for rat monocyte chemotactic protein-1 (MCP1), rat interleukin-18 (IL18), rat endothelial NO synthase (eNOS), rat dimethylarginine dimethylaminohydrolase (DDAH) 1, rat DDAH2, and rat vascular endothelial growth factor receptor-2 (VEGFR2) are listed in Supplementary Table 1.
Cathepsin D Activity Assay
Cathepsin D activity was determined by fluorimetric enzyme assay, according to the manufacturer’s protocol (Sigma-Aldrich). The internally quenched fluorescent substrate MCA-Gly-Lys-Pro-lle-Leu-Phe-Phe-Arg-Leu-Lys(DNP)-D-Arg-NH2 trifluoroacetate salt was used as the cathepsin D substrate. The release of fluorogenic reagent was measured at excitation and emission wavelengths of 328 and 393 nm, respectively. The change in activity was normalized to that of sample protein concentrations and is expressed as relative fluorescence fold change.
Nitrite Release From Kidney Slices
We measured nitrite release from kidney slices as described previously.22 Kidneys were cut into 50 μm sections by a vibratome. Five sections from each kidney were incubated with 10 mmol/l L-arginine in buffer (pH 7.4) containing 25 mmol/l HEPES, 140 mmol/l NaCl, 5 mmol/l KCl, 2 mmol/l CaCl2, 1 mmol/l MgCl2, and 5 mmol/l glucose at 37 °C for 36 h. Nitrite in the supernatant of the kidney slices was measured by the Griess method after protein precipitation. Values are corrected for protein in the tissue sample.
Statistical Analysis
Values are expressed as mean±s.e.m. All variables except the fibrosis score were evaluated by two-tailed unpaired Student t-test or Welch t-test. The glomerular fibrosis score was evaluated by Mann–Whitney U-test. A P-value of <0.05 denotes a statistically significant difference.
RESULTS
Pathophysiological Changes in Aging Rats
The physiological characteristics of the four age groups are listed in Table 1. Body weight increased with aging, and blood pressure was increased at 24 months of age. Serum creatinine level was increased from 10 months of age and was further elevated at 24 months of age. Levels of urinary protein excretion also increased with aging. Pathologically, tubulointerstitial injury, including tubular atrophy and interstitial fibrosis, was significantly increased in aged rats (24 months old) compared with young rats (4 months of age; Supplementary Figures 1a and b).
Angiostatin Generation in Aging Rat Kidney
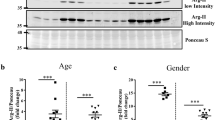
We detected kidney angiostatin generation by western blot analysis with an antibody against angiostatin kringle 1–3, so it could also detect plasminogen. Angiostatin generation increased with age (Figure 1a). Angiostatin can be generated from circulating plasminogen by cathepsin D23 or MMP-9.24 Cathepsin D expression (Figure 1a) and activity (Figure 1b) were also significantly increased in old rats compared with younger rats. MMP-9 expression and activity were decreased in older rats (Figures 1a and c).
Angiostatin production in aging rat kidney. (a) Western blot analysis for angiostatin, cathepsin D (CTPD), and matrix metalloproteinase 9 (MMP-9). n=6 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months of age (4 months). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH). (b) Cathepsin activity as determined by enzyme-linked immunosorbent assay. n=6–8 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months. (c) MMP-9 activity as determined by zymography. n=6 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months.
Capillary Volume and Inflammation in Aging Rat Kidney
Angiostatin has both an anti-angiogenic effect and an anti-inflammatory effect.25 Therefore, we assessed peritubular capillaries and inflammation in aging rats. PTC volume, as assessed by Tie2 protein expression (Figure 2a) and staining for RECA-1 (Figure 2b), showed no significant change in 10- or 16-month-old rats but showed a statistically significant decrease in 24-month-old rats compared with 4-month-old rats. The expression of the inflammatory cytokine MCP1 and IL18 was significantly increased after 16 months of age compared with 4 months of age (Figures 2c and d).
Peritubular capillary (PTC) loss and inflammatory cytokine expressions in aging rat kidney. (a) Western blot analysis for Tie2. n=6 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months of age (4 months). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH). (b) Staining for rat endothelial cell antigen-1 (RECA-1) in cortical PTC cells in 4 months and 24 months rats. Bar=100 μm. (d) Percent volume of PTC cells in renal cortex. n=6–8 for each group. Values are shown as mean±s.e.m. *P<0.05 versus 4 months. (c, d) Expression of monocyte chemotactic protein-1 (MCP1; (c) and interleukin-18 (IL18; d) mRNA as determined by quantitative real-time PCR. n=6–8 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months.
NO Production in Aging Rat Kidney
Decreases in NO promote angiostatin production.20 Therefore, we examined NO production in aging rat kidney. The expression of eNOS was decreased in aging rat kidney (Figure 3a). NOS activity is blocked by asymmetric dimethylarginine, which is metabolized by DDAH1, the predominant isoform in the proximal tubules of the kidney, and DDAH2, the predominant isoform in the vasculature. The expression of DDAH1 and DDAH2 were both decreased in aging rat kidney (Figure 3b). As shown in Figure 3c, nitrite production in the kidney was significantly decreased at 24 months of age.
Nitric oxide (NO) production in aging rat kidney. (a) Expression of endothelial NO synthase (eNOS) mRNA as determined by quantitative real-time PCR. n=6–8 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months of age (4 months). (b) Expression of dimethylarginine dimethylaminohydrolase (DDAH) 1 and DDAH2 mRNA as determined by quantitative real-time PCR. n=6–8 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months. (c) Nitrite production in kidney slices. n=6–8 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus 4 months.
Angiostatin Generation During Impaired NO Production
In vitro, we assessed the expression and activity of cathepsin D and MMP-9 in HUVECs under the condition of decreased NO production. Cathepsin D expression was increased in L-NAME-treated cells compared with control cells (Figure 4a). Cathepsin D activity was also increased in L-NAME-treated cells (Figure 4b). However, the expression and activity of MMP-9, also involved in angiostatin generation, were decreased in L-NAME-treated cells compared with control cells (Supplementary Figure 2). The generation of angiostatin from plasminogen was increased under the condition of decreased NO in response to L-NAME treatment (Figure 5), and angiostatin generation was blocked by pepstatin A, an inhibitor of acid proteases including cathepsin D.
Regulation of cathepsin D by nitric oxide in human umbilical vein endothelial cells. (a) Western blot analysis for cathepsin D (CTPD) after treatment with L-NG-nitroarginine methyl ester (L-NAME). n=8 for each group. Values are expressed as mean±s.e.m. *P<0.05 versus control. (b) CTPD activity after treatment with L-NAME. n=8 for each group. Values are expressed as mean±s.e.m. *P<0.05 versus control.
Angiostatin generation in response to decreased nitric oxide in human umbilical vein endothelial cells. After treatment with L-NG-nitroarginine methyl ester (L-NAME) for 24 h, the medium was changed to acidic medium. After 1 h, human plasminogen was added, and the cells were incubated for 1 h. The medium was collected, and western blot analysis was performed for angiostatin. Pepstatin A (Pep A) was used as a cathepsin D (CTPD) inhibitor. Bovine CTPD was used as a positive control. n=4 for each group. Values are expressed as mean±s.e.m. *P<0.05 versus control. †P<0.05 versus 5 mM L-NAME.
Angiostatin Generation in L-NAME or Molsidomine-Treated Aged-Rat Kidney
We used L-NAME- or molsidomine-treated rat kidney to elucidate the role of NO on angiostatin production. The physiological characteristics of L-NAME and molsidomine-treated rats are listed in Table 2. Blood pressure and serum creatinine level were significantly increased in L-NAME-treated rats. The excretion of urinary nitrate was decreased in L-NAME-treated rats compared with control rats. In contrast, the excretion of urinary nitrate was significantly increased in molsidomine-treated rats compared with control rats. Renal tubulointerstitial fibrosis was significantly increased in L-NAME-treated rat kidney (Figures 6a and b). Angiostatin generation was also significantly increased along with increased cathepsin D expression and activity in L-NAME-treated rat kidney (Figures 6c–e). Tubulointerstitial fibrosis was significantly lower in molsidomine-treated rat kidney than control rat kidney (Figures 6a and b). In molsidomine-treated rat kidney, angiostatin generation and the expression and activity of cathepsin D were also significantly decreased (Figures 6c and e).
Tubulointerstitial fibrosis and angiostatin production in L-NG-nitroarginine methyl ester (L-NAME) or molsidomine-treated aged-rat kidney. (a) Masson trichrome staining showing renal cortical morphology in control (n=4), L-NAME-treated (20 mg/l in drinking water; L-NAME, n=5), and molsidomine-treated (120 mg/l in drinking water; molsidomine, n=6) rats. Bar=100 μm. (b) Interstitial fibrosis score. n=4–6. Values are expressed as mean±s.e.m. *P<0.05 versus control. (c) Western blot analysis for angiostatin. n=4–6. Values are expressed as mean±s.e.m. *P<0.05 versus control. (d, e) Cathepsin D (CTPD) protein expression (d) and activity (e). n=4–6 for each group. Data are expressed as mean±s.e.m. *P<0.05 versus control.
Capillary Volume and Inflammation in L-NAME- or Molsidomine-Treated Aged-Rat Kidney
We examined whether modulating NO production in aged rats alters renal inflammation and capillary loss. L-NAME treatment decreased Tie2 and VEGFR2 expression (Figures 7a and b) but increased renal MCP1 and IL18 expression (Figures 7c and d). In contrast, molsidomine treatment did not change Tie2 or VEGFR2 expression (Figures 7a and b) but significantly decreased renal MCP1 and IL18 expression (Figures 7c and d).
Endothelial cell marker expression and inflammatory cytokine in L-NG-nitroarginine methyl ester (L-NAME) or molsidomine-treated aged-rat kidney. (a) Expression of Tie2 as determined by western blot analysis in control (n=4), L-NAME-treated (20 mg/l in drinking water; L-NAME, n=5), and molsidomine-treated (120 mg/l in drinking water; molsidomine, n=6) rats. Values are expressed as mean±s.e.m. *P<0.05 versus control. (b–d) Expression of vascular endothelial growth factor receptor-2 (VEGFR2; a), monocyte chemotactic protein-1 (MCP1; b), and interleukin-18 (IL18; c) mRNA as determined by quantitative real-time PCR. n=4–6 for each group. Values are expressed as mean±s.e.m. *P<0.05 versus control.
DISCUSSION
The purpose of this study was to investigate whether angiostatin generation is increased in the aging kidney and to elucidate the mechanism of angiostatin production, in addition to the effect of NO deficiency. Results indicated that NO deficiency activates cathepsin D activity in vivo and in vitro, and angiostatin generation by cathepsin D is increased in aging rat kidney.
Our results also showed that NO availability was decreased in aged rat kidney, accompanied by decreased eNOS and DDAH expression. These results are consistent with those of Erdely et al,26 who reported that renal NO synthase activity is decreased with advancing age. In the aging kidney, NO bioavailability is also decreased, owing to an excess amount of superoxide generated by NAD(P)H oxidase.27 We have also previously reported an accumulation of oxidative stress caused by decreased transcription of antioxidant genes in the aged rat kidney.8 Loss of NO availability in the aged kidney would be expected to result in several adverse effects, including decreased renal perfusion, increased renal vasoconstriction, and enhancement of fibrosis. NO may have a role in modulating matrix deposition in the kidney, the secretion of fibrogenic cytokines, and interstitial fibrosis.28 Thus, loss of NO availability might contribute to the formation of the tubulointerstitial lesions observed in aging by other pathways in addition to angiostatin production.
In this study, we showed that cathepsin D activity was increased in aged kidney, and decreased NO induced an increase in cathepsin D activity in vivo and in vitro. We also showed that cathepsin D activity was decreased in molsidomine-treated kidney, in which increased NO induced a decrease in cathepsin D activity. Graciano et al29 also reported that cathepsin D expression is increased in L-NAME-treated Wistar rat kidney. We also confirmed that cathepsin D activity was increased in eNOS deletion mice compared with the wild-type mice at the age of 12 months (observational data). Indeed, NO production could be involved in cathepsin D activity and angiostatin generation in the kidney.
Transcriptional activation of cathepsin D gene expression is regulated by several growth factors, including insulin-like growth factor-I, transforming growth factor-α, and epidermal growth factor.30 However, the mechanism whereby NO deficiency increases cathepsin D expression is not clear. Aspartic acid proteases change from precursor enzyme to active mature enzyme under appropriate conditions. Cathepsin D is converted from procathepsin D by MMP-2.31 The expression and activity of MMP-2 is negatively regulated by NO.32 Therefore, a loss of NO bioavailability would induce MMP-2 activation. In fact, we observed that MMP-2 activity was significantly increased in aged rat kidney (Supplementary Figure 3), which resulted in increased cathepsin D activity. These data indicate that cathepsin D activity may be regulated in part by MMP-2 via NO reduction.
Our present results provide evidence for increased angiostatin generation in aged rat kidney and L-NAME-treated kidney, accompanied by increased cathepsin D activation. Angiostatin can be generated by proteolytic cleavage from plasminogen. There are a number of proposed proteolytic mechanisms by which plasminogen is cleaved to form angiostatin.10 For example, cathepsin D possesses angiostatin-generating activity.23 We also confirmed that cathepsin D could generate angiostatin from plasminogen in L-NAME-treated endothelial cells. A cathepsin D inhibitor, pepstatin A, inhibited the cleavage of plasminogen to angiostatin. Perchick and Jabbour33 demonstrated that cathepsin D-mediated cleavage of plasminogen to angiostatin can be inhibited by overexpression of cyclooxygenase-2. Therefore, it is possible that a cyclooxygenase inhibitor could increase the angiostatin level in vivo. MMP-2 and MMP-9 also possess angiostatin-generating activity.34, 35 However, we confirmed that MMP-9 activity was decreased in aged rat kidney. Thus, MMP-9 may be not involved in angiostatin generation under the condition of decreased NO bioavailability.
The present findings showed that angiostatin generation is increased in aging kidney but did not elucidate whether angiostatin participates directly in tubulointerstitial damage through PTC loss in the aging rat kidney. Therefore, to determine whether angiostatin directly induces tubulointerstitial damage in the aging rat kidney, further studies of angiostatin blockake or angiostatin overexpression are needed. Conversely, there are some reports on the therapeutic potential of angiostatin in renal disease. It has been reported that angiostatin overexpression improves renal injury by an anti-inflammatory mechanism in a rats subjected to subtotal nephrectomy.25 Angiostatin may exert a therapeutic effect in renal disease via its anti-inflammatory actions. However, potential adverse effects, such as a decrease in PTCs via its anti-angiogenic actions, thus leading to acceleration of tubular hypoxia/ischemia, have to be considered.36 Angiostatin has been reported to inhibit diabetic renal injury in streptozotocin-induced diabetes.12 If neovascularization does indeed contribute significantly to the pathogenesis of diabetic nephropathy, then antiangiogenic therapies involving angiostatin might be effective.
Recent reports have indicated that angiostatin has anti-inflammatory and anti-fibrotic action in addition to anti-angiogenic action.12, 25 However, our data indicate that the expression of MCP1 and IL18 was increased in aged kidney in spite of increased angiostatin generation. Angiostatin generation was also increased in L-NAME-treated aged rat kidney, whereas MCP1 and IL18 expression was not decreased in L-NAME-treated aged rat kidney. In contrast, in molsidomine-treated rat kidney, MCP1 and IL18 expression and angiostatin generation were both decreased. On the basis of these data, we suggest that angiostatin production is increased to control inflammation induced by a decline in NO production in aged kidney. However, inflammation becomes so strong with aging that angiostatin generation is notably more increased. It appears that increased angiostatin levels can suppress new angiogenesis leading to PTC loss and tissue fibrosis in aged kidney. If so, inflammation control will become an important target for the amelioration of aged kidney function. However, further studies are needed to clarify whether inflammation control directly affects angiostatin generation.
In conclusion, our present results showed that angiostatin generation by cathepsin D was increased in the aging rat kidney, and decreased NO production activated cathepsin D activity. Increased angiostatin production could be related to interstitial damage in the aging rat kidney.
References
Levey AS, Coresh J, Balk E et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 2003;139:137–147.
Abdelhafiz AH, Brown SH, Bello A et al. Chronic kidney disease in older people: physiology, pathology or both? Nephron Clin Pract 2010;116:c19–c24.
Ohashi R, Kitamura H, Yamanaka N . Peritubular capillary injury during the progression of experimental glomerulonephritis in rats. J Am Soc Nephrol 2000;11:47–56.
Choi YJ, Chakraborty S, Nguyen V et al. Peritubular capillary loss is associated with chronic tubulointerstitial injury in human kidney: altered expression of vascular endothelial growth factor. Hum Pathol 2000;31:1491–1497.
Yuan HT, Li XZ, Pitera JE et al. Peritubular capillary loss after mouse acute nephrotoxicity correlates with down-regulation of vascular endothelial growth factor-A and hypoxia-inducible factor-1 alpha. Am J Pathol 2003;163:2289–2301.
Thomas SE, Anderson S, Gordon KL et al. Tubulointerstitial disease in aging: evidence for underlying peritubular capillary damage, a potential role for renal ischemia. J Am Soc Nephrol 1998;9:231–242.
Kang DH, Anderson S, Kim YG et al. Impaired angiogenesis in the aging kidney: vascular endothelial growth factor and thrombospondin-1 in renal disease. Am J Kidney Dis 2001;37:601–611.
Satoh M, Fujimoto S, Horike H et al. Mitochondrial damage-induced impairment of angiogenesis in the aging rat kidney. Lab Invest 2011;91:190–202.
O'Reilly MS, Holmgren L, Shing Y et al. Angiostatin: a novel angiogenesis inhibitor that mediates the suppression of metastases by a Lewis lung carcinoma. Cell 1994;79:315–328.
Soff GA . Angiostatin and angiostatin-related proteins. Cancer Metastasis Rev 2000;19:97–107.
Basile DP, Fredrich K, Weihrauch D et al. Angiostatin and matrix metalloprotease expression following ischemic acute renal failure. Am J Physiol Renal Physiol 2004;286:F893–F902.
Zhang SX, Wang JJ, Lu K et al. Therapeutic potential of angiostatin in diabetic nephropathy. J Am Soc Nephrol 2006;17:475–486.
Ziche M, Morbidelli L . Nitric oxide and angiogenesis. J Neurooncol 2000;50:139–148.
Cooke JP, Losordo DW . Nitric oxide and angiogenesis. Circulation 2002;105:2133–2135.
Wever R, Boer P, Hijmering M et al. Nitric oxide production is reduced in patients with chronic renal failure. Arterioscler Thromb Vasc Biol 1999;19:1168–1172.
Hill C, Lateef AM, Engels K et al. Basal and stimulated nitric oxide in control of kidney function in the aging rat. Am J Physiol 1997;272:R1747–R1753.
Reckelhoff JF, Kellum JA, Blanchard EJ et al. Changes in nitric oxide precursor, L-arginine, and metabolites, nitrate and nitrite, with aging. Life Sci 1994;55:1895–1902.
Tank JE, Vora JP, Houghton DC et al. Altered renal vascular responses in the aging rat kidney. Am J Physiol 1994;266:F942–F948.
Ridnour LA, Isenberg JS, Espey MG et al. Nitric oxide regulates angiogenesis through a functional switch involving thrombospondin-1. Proc Natl Acad Sci USA 2005;102:13147–13152.
Matsunaga T, Weihrauch DW, Moniz MC et al. Angiostatin inhibits coronary angiogenesis during impaired production of nitric oxide. Circulation 2002;105:2185–2191.
Bongartz LG, Braam B, Verhaar MC et al. The nitric oxide donor molsidomine rescues cardiac function in rats with chronic kidney disease and cardiac dysfunction. Am J Physiol Heart Circ Physiol 2010;299:H2037–H2045.
Tojo A, Kimoto M, Wilcox CS . Renal expression of constitutive NOS and DDAH: separate effects of salt intake and angiotensin. Kidney Int 2000;58:2075–2083.
Morikawa W, Yamamoto K, Ishikawa S et al. Angiostatin generation by cathepsin D secreted by human prostate carcinoma cells. J Biol Chem 2000;275:38912–38920.
Cornelius LA, Nehring LC, Harding E et al. Matrix metalloproteinases generate angiostatin: effects on neovascularization. J Immunol 1998;161:6845–6852.
Mu W, Long DA, Ouyang X et al. Angiostatin overexpression is associated with an improvement in chronic kidney injury by an anti-inflammatory mechanism. Am J Physiol Renal Physiol 2009;296:F145–F152.
Erdely A, Greenfeld Z, Wagner L et al. Sexual dimorphism in the aging kidney: effects on injury and nitric oxide system. Kidney Int 2003;63:1021–1026.
Adler S, Huang H, Wolin MS et al. Oxidant stress leads to impaired regulation of renal cortical oxygen consumption by nitric oxide in the aging kidney. J Am Soc Nephrol 2004;15:52–60.
Baylis C . Sexual dimorphism in the aging kidney: differences in the nitric oxide system. Nat Rev Nephrol 2009;5:384–396.
Graciano ML, Cavaglieri Rde C, Delle H et al. Intrarenal renin–angiotensin system is upregulated in experimental model of progressive renal disease induced by chronic inhibition of nitric oxide synthesis. J Am Soc Nephrol 2004;15:1805–1815.
Wang F, Duan R, Chirgwin J et al. Transcriptional activation of cathepsin D gene expression by growth factors. J Mol Endocrinol 2000;24:193–202.
Cho JH, Park IY, Kim MS et al. Matrix metalloproteinase 2 is involved in the regulation of the antimicrobial peptide parasin I production in catfish skin mucosa. FEBS Lett 2002;531:459–463.
Chen HH, Wang DL . Nitric oxide inhibits matrix metalloproteinase-2 expression via the induction of activating transcription factor 3 in endothelial cells. Mol Pharmacol 2004;65:1130–1140.
Perchick GB, Jabbour HN . Cyclooxygenase-2 overexpression inhibits cathepsin D-mediated cleavage of plasminogen to the potent antiangiogenic factor angiostatin. Endocrinology 2003;144:5322–5328.
Patterson BC, Sang QA . Angiostatin-converting enzyme activities of human matrilysin (MMP-7) and gelatinase B/type IV collagenase (MMP-9). J Biol Chem 1997;272:28823–28825.
O'Reilly MS, Wiederschain D, Stetler-Stevenson WG et al. Regulation of angiostatin production by matrix metalloproteinase-2 in a model of concomitant resistance. J Biol Chem 1999;274:29568–29571.
Maeshima Y, Makino H . Angiogenesis and chronic kidney disease. Fibrogenesis Tissue Repair 2010;3:13.
Acknowledgements
This study was supported by a Research Project Grant from Kawasaki Medical School (no. 20-213O and 23-KI69 to MS), Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (no. 21591046 to MS, no. 21591047 to NK) and the Ryobi Teien Memory Foundation (MS). We thank Ms Etsuko Yorimasa, Ms Miki Ishihara, Ms Keiko Satoh, and Ms Satomi Hanada (Kawasaki Medical School) for animal care and technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
Impaired angiogenesis, associated with progressive loss of renal microvasculature, may be a cause of age-related nephropathy. A mechanism is proposed for capillary loss in the aging kidney: When nitric oxide availability is decreased, activation of cathepsin D occurs, which increases generation of angiostatin, a potent inhibitor of angiogenesis.
Rights and permissions
About this article
Cite this article
Satoh, M., Kidokoro, K., Ozeki, M. et al. Angiostatin production increases in response to decreased nitric oxide in aging rat kidney. Lab Invest 93, 334–343 (2013). https://doi.org/10.1038/labinvest.2012.171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2012.171
Keywords
This article is cited by
-
Urinary angiostatin: a novel biomarker of kidney disease associated with disease severity and progression
BMC Nephrology (2019)
-
Ageing and microvasculature
Vascular Cell (2014)