Abstract
Objective:
We evaluated the efficacy of surfactant therapy and assisted ventilation on morbidity and mortality of neonates with birth weight (BW) ⩾1500 g and hypoxemic respiratory failure (HRF).
Study Design:
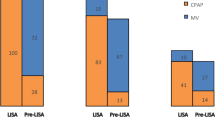
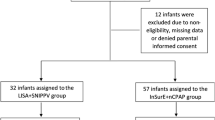
We retrospectively analyzed 5650 patients with BW ⩾1500 g for incidence, management and outcome of HRF, defined as acute hypoxemia requiring mechanical ventilation and/or nasal continuous positive airway pressure ⩾24 h. The patients were allocated into groups of moderate preterm (1735, 30.7%), late preterm (1431, 25.4%), early term (ETM, 986, 17.5%), full term (1390, 24.6%) and post term (79, 1.4%), with gestational age ⩽33, 34 to 36, 37 to 38, 39 to 41 and ⩾42 weeks, respectively.
Results:
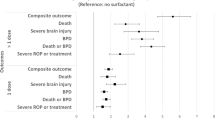
In the five groups, 66.9, 42, 21.6, 12.8 and 5.1% had respiratory distress syndrome (RDS). For pneumonia/sepsis and meconium aspiration syndrome (MAS), the proportion was 13.8%, 25.4%, 38.0%, 52.5% and 76.0%, respectively. Surfactant was given to 21.9% (n=1238) of HRF and 51.2% (n=1108) of RDS. Survival rates of RDS were 82.2%, 87.8%, 84.5%, 77.1% and 75.0%, respectively (numbers needed to treat was 8 to 11 for surfactant benefit). Overall mortality rate of HRF was 21%, or 17.9%, 14.7%, 25.6%, 28.9% and 39.2%, respectively. Mortalities of MAS and pneumonia/sepsis were 29.4 and 27.6%. Relative risk of death was associated with initial disease severity, female gender, mechanical ventilation and congenital anomalies by multivariate logistic regression analysis.
Conclusion:
Surfactant was effective for infants with RDS and BW ⩾1500 g, and different incidences and outcome of HRF among GA groups reflected standard of perinatal and respiratory care in emerging neonatal intensive care unit network.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hack M, Fanaroff AA . Outcomes of children of extremely low birth weight and gestational age in the 1990 s. Semin Neonatol 2000; 5 (2): 89–106.
Lemons J, Bauer C, Oh W, Korones S, Papile L, Stoll B et al. Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Research Network, January 1995 through December 1996. Pediatrics 2001; 107 (1): e1.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR et al. Trends in neonatal morbidity and mortality for very low birth weight infants. Am J Obstet Gynecol 2007; 196 (2): 147. e1–8.
Marshall DD, Kotelchuck M, Young TE, Bose CL, Kruyer L, O'Shea TM et al. Risk factors for chronic lung disease in the surfactant era: a North Carolina population-based study of very low birth weight infants. Pediatrics 1999; 104 (6): 1345–1350.
Kramer MS, Demissie K, Yang H, Platt RW, Sauvé R, Liston R et al. The contribution of mild and moderate preterm birth to infant mortality. JAMA 2000; 284 (7):843–849.
Raju TN, Higgins RD, Stark AR, Leveno KJ . Optimizing care and outcome for late preterm (near-term) infants: a summary of the workshop sponsored by the National Institute of Child Health and Human Development. Pediatrics 2006; 118 (3): 1207–1214.
Engle WA, Tomashek KM,, Wallman C. Committee on Fetus and Newborn, American Academy of Pediatrics. 'Late preterm' infants: a population at risk. Pediatrics 2007; 120 (6):1390–1401.
Clark RH, The Near-term Respiratory Failure Research Group. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol 2005; 25 (4): 251–257.
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J et al. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics 2008; 121 (2): e223–e232.
Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, Hoffman M et al. Respiratory morbidity in late preterm births. JAMA 2010; 304 (4): 419–425.
Reddy UM, Ko CW, Willinger M . ‘Early’ term births (37–38 weeks) are associated with increased mortality. Am J Obstet Gynecol 2006; 195 (6): S202.
Engle WA, Kominiarek MA . Late preterm infants, early term infants, and timing of elective deliveries. Clin Perinatol 2008; 35 (2): 325–341.
The American College of Obstetricians and Gynecologists Committee of Obstetric practice and Society of Maternal–Fetal Medicine. Committee opinion (No. 579): definition of term pregnancy. Obstet Gynecol 2013; 122 (5): 1139–1140.
Kamath BD, MacGuire ER, McClure EM, Goldenberg RL, Jobe AH . Neonatal mortality from respiratory distress syndrome: lessons for low-resource countries. Pediatrics 2011; 127 (6): 1139–1146.
Wilson A, Gardner MN, Armstrong MA, Folck BF, Escobar GJ . Neonatal assisted ventilation: predictors, frequency, and duration in a mature managed care organization. Pediatrics 2000; 105 (4, Part 1): 822–830.
Angus DC, Linde-Zwirble WT, Clermont G, Griffin MF, Clark RH . Epidemiology of neonatal respiratory failure in the United States: projections from California and New York. Am J Respir Crit Care Med 2001; 164 (7): 1154–1160.
Qian LL, Huang QW, Sun MY, Song SM, Li KH, Song GW et alon behalf of Chinese Collaborative Study Group for Neonatal Respiratory Diseases. Treatment of severe meconium aspiration syndrome with porcine surfactant: a multicenter, randomized, controlled trial. Acta Paediatr 2005; 94 (6):896–902.
Qian L, Liu C, Zhuang W, Gao Y, Yu J, Chen H et al. Neonatal respiratory failure: a 12-month clinical epidemiologic study from 2004 to 2005 in China. Pediatrics 2008; 121 (5): e1115–e1124.
Ma L, Liu C, Wang Y, Li S, Zhai S, Gu X et al. Mortality of neonatal respiratory failure related to socioeconomic factors in Hebei province of China. Neonatology 2010; 100 (1): 16–22.
Wang H, Gao X, Liu C, Yan C, Lin X, Yang Z et al. Morbidity and mortality of neonatal respiratory failure in China. Surfactant treatment in very immature infants. Pediatrics 2012; 129 (3): e731–e740.
Wang Y, Liu C, Gao X, Yang C, Shan R, Zhuang D et al. Effects of inhaled nitric oxide in neonatal hypoxemic respiratory failure in resource limited condition. Chin Med J 2011; 124 (8): 1156–1163.
Sun B, Shao X, Cao Y, Xia S, Yue H . Neonatal-perinatal medicine in a transitional period in China. Arch Dis Fetal Neonat Ed 2013; 98 (5): 440–444.
Sun L, Yue H, Sun B, Han L, Tian Z, Qi M et al. Estimation of birth population-based perinatal–neonatal mortality and preterm rate in China from a regional survey in 2010. J Matern Fetal Neonatal Med 2013; 26 (16): 1641–1648.
Sun L, Yue H, Sun B, Han L, Tian Z, Qi M et alHuai’an Perinatal–Neonatal Study Group.. Estimation of high risk pregnancy contributing to perinatal morbidity and mortality from a birth population-based regional survey in 2010 in China. BMC Pregn Childbirth 2014; 14: 338.
World Health Organization International Statistical Classification of Diseases and Related Health Problems, 10th revision, vol. 2, 2nd edn.WHO: Geneva, Switzerland, 2004.
Taeusch HW, Ballard RA . Avery’s Diseases of the Newborn, 7th edn.WB Saunders: Philadelphia, PA, USA, 1998.
Hjarlmarson O . Epidemiology and classification of acute neonatal respiratory disorders: a prospective study. Act Paediatr 1981; 70 (9): 773–783.
Dargaville PA, Copnell B, The Australian and New Zealand Neonatal Network. The epidemiology of meconium aspiration syndrome: incidence, risk factors, therapies, and outcome. Pediatrics 2006; 117 (5): 1712–1721.
Macones GA, Hankins GD, Spong CY, Hauth J, Moore T . The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol 2008; 112 (3): 661–666.
International Liaison Committee on Resuscitation. The International Liaison Committee on Resuscitation (ILCOR) consensus on science with treatment recommendations for pediatric and neonatal patients: neonatal resuscitation. Pediatrics 2006; 117 (5): e978–e988.
Peacock JL, Peacock PJ. Chapter 11. Analysing multiple observation per subject. In:Oxford Handbook of Medical Statistics, 1st edn.Oxford University Press: New York, NY, USA, 2011, pp377–392.
Sun B, Liang K, Yi B, Zhang L . Challenges in post-MDG4 achievement for Chinese child health care. Arch Dis Childh 2015; 100 (Suppl 1., Global Health MDG): s61–s62.
Khashu M, Narayanan M, Bhargava S, Osiovich H . Perinatal outcomes associated with preterm birth at 33 to 36 weeks’ gestation: a population-based cohort study. Pediatrics 2009; 123 (1): 109–113.
Engle WA, Committee on Fetus and Newborn. Surfactant replacement therapy for respiratory distress in the preterm and term neonate. Pediatrics 2008; 121 (2): 419–432.
Polin RA, Carlo WA, Committee on Fetus and Newborn; American Academy of Pediatrics. Surfactant-replacement therapy for preterm and term neonates with respiratory distress. Pediatrics 2014; 133 (1): 156–163.
Davidoff MJ, Dias T, Damus K, Russell R, Bettegowda VR et al. Changes in the gestational age distribution among U.S. singleton births: Impact on rates of late preterm birth, 1992 to 2002. Semin Perinatol 2006; 30 (1): 8–15.
Young PC, Glasgow TS, Li X, Guest-Warnick G, Stoddard G . Mortality of late-preterm (near-term) newborns in Utah. Pediatrics 2007; 119 (3): e659.
Colin AA, McEvoy C, Castile RG . Respiratory morbidity and lung function in preterm infants of 32 to 36 weeks' gestational age. Pediatrics 2010; 126 (1): 115–128.
Teune MJ, Bakhuizen S, Gyamfi Bannerman C, Opmeer BC, van Kaam AH, van Wassenaer AG et al. A systematic review of severe morbidity in infants born late preterm. Am J Obstet Gynecol 2011; 205 4 (374): e1–e9.
Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, Petrini JR . Differences in mortality between late-preterm and term singleton infants in the United States, 1995–2002. J Pediatr 2007; 151 (5): 450–456.
Leone A, Ersfeld P, Adams M, Schiffer PM, Bucher HU, Arlettaz R . Neonatal morbidity in singleton late preterm infants compared with full-term infants. Act Paediatr 2012; 101 (1): e6–e10.
Bastek JA, Sammel MD, Paré E, Srinivas SK, Posencheg MA, Elovitz MA . Adverse neonatal outcomes: examining the risks between preterm, late preterm, and term infants. Am J Obstet Gynecol 2008; 199 (4): e1–e8.
Celik IH, Demirel G, Canpolat FE, Dilmen U . A common problem for neonatal intensive care units: late preterm infants, a prospective study with term controls in a large perinatal center. J Matern Fetal Neonatal Med 2013; 26 (5): 459–462.
El Shahed AI, Dargaville PA, Ohlsson A, Soll R . Surfactant for meconium aspiration syndrome in term and late preterm infants. Cochrane Database Syst Rev 2014; 12 (12): CD002054.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R et al. European consensus guideline on the management of neonatal respiratory distress syndrome in preterm infants-2013 update. Neonatology 2013; 103 (4): 353–368.
Kattan J, González A, Becker P, Faunes M, Estay A, Toso P et al. Survival of newborn infants with severe respiratory failure before and after establishing an extracorporeal membrane oxygenation program. Pediatr Crit Care Med 2013; 14 (9): 876–888.
Acknowledgements
This study was supported by grants for Excellence in Neonatal Medicine, National Commission of Health and Family Planning, the Project 211 (phase III), Ministry of Education, and Shanghai Municipal Department of Health (No. LJ06038).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Chinese Collaborative Study Group for Neonatal Respiratory Diseases
Bo Sun6, Huanhuan Wang6, Chao Chen6, Yun Cao6, Liling Qian6, Xirong Gao7, Jinsong Mu7, Yong Xiao7, Jun Li7, Cuiqing Liu8, Yanmei Guo8, 9Chaoying Yang9, Min Qian9, Xinzhu Lin10, Jing Huang10, Changyi Yang11, Bin Yang11, Wenjian Chen11, Zhenlang Lin12, Baiwei Wu12, Wenjun Zhu13, Ning Tan13, Lixia Li13, Zhanghua Hou13, Yue’e Xie13, Xiaoqin Gong13, Zhouli Wu13, Zhenying Yang14, Ji Qi14, Fengqin Yu15, Yingge Kang15, Kai Jang15, Xiaojuan Shi15, Yan Sun15, Wansong Feng15, Yulian Hu15, Yinping Qiu16, Lin Shi16, Fang Zhao16, Baolan Yan16, Yanbo Zhang16, Xianzhi Liu17, Guang Lin17, Qiufen Wei17, Xiaoyu Zhou18, Rui Cheng18, Yun Feng18, Yue Wu18, Yunsu Zou18, Yan Guo18, Qing Que18, Li Zhao18, Li Qian18, Junying Xie19, Hong Xiong20, Huqing Sun20, Shaoru He21, Jin Zhong21, Yifei Wang21, Deyi Zhuang22, Xiaojuan Liu22, Acheng Chen22, Zhengkun He22, Fuqiang Sun23, Yuyan Wang23, Yuqin Chu23, Jie Yang24, Jianwen Xiang24, Hongni Yue25, Liangrong Han25, Dongmei Chen26, Ying He26, Sannan Wang27, Zuming Yang27, Jing Zhou27, Xiaofeng Gu28, Ying Huang28, Ruobing Shan29, Lihua Sun29, Jun Zheng30, Xiaopeng Wang30, Ling Liu31, Wei Wang31, Zhihui Xiao32, Xiaochun Ding32, Xiaoqian Chen32, Mei Li33, Fei Lu33, Xiaoyan Song33, Fang Liu34, Zhimei Guo34, Zhifang Du34, Dezhi Mu35, Ying Xiong35, Hua Wang35, Chao Chen35, Zhijun Wu36, Shanqiu Xiao36, Xiangming Zhou37, Huafei Huang37, Pingming Gao38, Lixia Zhang38, Xiaozhuang Gan39, Lifeng Hou39, Mingyue Liu39, Yuan Shi40, Li Wang40, Bin Yi41, Hongxia Gao41, Xiaohong Liu42, Di Gao42, Lifeng Qi42, Xiaodong Li43, Qing Tian43, Shuping Han44, Danqing Wu44, Zheng Liu45, Yangjiang Chen45, Qin Zhang46, Hongru Lu46, Hua Kang46, Hongtao Lei46, Xiaomei Yang46, Daxin Cheng46, Yuxing Zheng46, Min Yu47, Xiaolei Wang47, Xiaoliang Wang48, Qing Chu48, Wenjuan Tu49, Lin Li49, Baohai Shi50, Guo Yao50, Yan Wang50, Kun Liang51, Qinghua Zhong51, Shaojie Yue52, Zheng’e Liao52, Yuchun Huang53, Yudan Li53, Jichang Chen54, Liming Ni55, Li Zhang55, Juan Zhang55, Jun’an Zeng55, Yanna Fu56, Yuwei Zhao57, Ping Zha57, Yejun Jiang57, Xiaoling Bai58, Yanhua Cao58, Jiahua Pan59, Yong Lv59, Lihong Li60, Jin Bao60
6Children’s Hospital of Fudan University, Shanghai, China; 7Hunan Provincial Children’s Hospital, Changsha, China; 8Hebei Provincial Children’s Hospital, Shijiazhuang, China; 9First Hospital of Jilin University, Changchun, China; 10Xiamen Maternity Hospital, Xiamen, China; 11Fujian Provincial Maternity Hospital, Fuzhou, China; 12Yuying Children’s Hospital of Wenzhou Medical College, Wenzhou, China; 13Chenzhou Children’s Hospital, Chenzhou, China; 14Tai’an Maternity Hospital, Tai’an, China; 15Zhenzhou Maternity Hospital, Zhenzhou, China; 16Ningxia Medical University Hospital, Yinchuan, China; 17Guangxi Maternity Hospital, Nanning, China; 18Nanjing Children’s Hospital of Nanjing Medical University, Nanjing, China; 19Kaifeng Children’s Hospital, Kaifeng, China; 20Zhengzhou Children’s Hospital, Zhengzhou, China; 21Guangdong General Hospital, Guangzhou, China; 22First Hospital of Xiamen University, Xiamen, China; 23Second Hospital of Tianjin Medical University, Tianjin, China; 24Guangdong Provincial Maternity Hospital, Guangzhou, Guangdong, China; 25Huai’an Maternity Hospital, Huai’an, Jiangsu, China; 26Quanzhou Children’s Hospital, Quanzhou, Fujian, China; 27Suzhou Women and Children’s Health Center, Suzhou, China; 28Central Hospital of China National Petroleum Corporation, Langfang, China; 29Qingdao Children’s Hospital, Qingdao, China; 30Tianjin Central Maternity Hospital, China; 31Guiyang Maternity Hospital, Guiyang, China; 32Children’s Hospital of Suzhou University, Suzhou, China; 33Harbin Children’s Hospital, Harbin, China; 34Bethune International Peace Hospital, Shijiazhuang, China; 35Second Hospital of Sichuan University, Chengdu, China; 36Shenzhen Bao’an Maternity Hospital, Shenzhen, China; 37Jiaxing Maternity Hospital, Jiaxing, China; 38Foshan Maternity Hospital, Foshan, China; 39Children’s Hospital of Capital Institute of Pediatrics, Beijing, China; 40Daping Hospital of Third Military Medical University, Chongqing, China; 41Gansu Provincial Maternity Hospital, Lanzhou, China; 42Shenzhen Children’s Hospital, Shenzhen, China; 43Shenzhen Nanshan Hospital, Shenzhen, China; 44Nanjing Maternity Hospital, Nanjing, China; 45Shanxi Provincial Children’s Hospital, Taiyuan, China; 46Shaanxi Provincial General Hospital, Xi’an, China; 47Wuxi General Hospital, Wuxi, China; 48Yuhuangding Hospital, Yantai, China; 49Changzhou Children’s Hospital, Changzhou, China; 50Tai’an Central Hospital, Tai’an, China; 51First Hospital of Kunming Medical College, Kunming, China; 52Xiangya Hospital of Zhongnan University, Changsha, China; 53Dalian Children’s Hospital, Dalian, China; 54Liuzhou Maternity Hospital, Liuzhou, China; 55Shaanxi Provincial Maternity Hospital, Xi’An, China; 56Anhui Provincial Children’s Hospital, Hefei, China; 57Shaoxing Maternity Hospital, Shaoxing, China; 58PLA Military General Hospital, Jinan, China; 59Anhui Provincial Hospital, Hefei, China; 60Changchun Children’s Hospital, Changchun, China.
Rights and permissions
About this article
Cite this article
Wang, H., Gao, X., Liu, C. et al. Surfactant reduced the mortality of neonates with birth weight ⩾1500 g and hypoxemic respiratory failure: a survey from an emerging NICU network. J Perinatol 37, 645–651 (2017). https://doi.org/10.1038/jp.2016.272
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.272
This article is cited by
-
Global, Regional and National Trends in the Burden of Neonatal Respiratory Failure and essentials of its diagnosis and management from 1992 to 2022: a scoping review
European Journal of Pediatrics (2023)
-
Perinatal Risks of Neonatal and Infant Mortalities in a Sub-provincial Region of China: A Livebirth Population-based Cohort Study
BMC Pregnancy and Childbirth (2022)
-
Outcome of neonatal hypoxemic respiratory failure: a livebirth population-based retrospective survey
BMC Pediatrics (2022)
-
Outcomes associated with surfactant in more mature and larger premature infants with respiratory distress syndrome
Journal of Perinatology (2020)
-
High risk pregnancy associated perinatal morbidity and mortality: a second birth population-based survey in Huai’an in 2015
BMC Pregnancy and Childbirth (2019)