Abstract
Objective:
Compassion fatigue (CF) is distress experienced by caregivers from ongoing contact with patients who are suffering. Burnout (BO) is occupational stress directly related to dissonance between job demands and available resources. Compassion satisfaction (CS) is professional fulfillment experienced through helping others. CF in physicians is not well studied. Neonatologists may be at particular risk for CF by virtue of recurrent exposure to distress in patients and their families. The objectives of this study were to determine the prevalence of CF, BO and CS, and to identify potential predictors for these phenomena in neonatologists.
Study design:
A modified Compassion Fatigue and Satisfaction Self-Test and a questionnaire of professional details and personal characteristics were distributed electronically to neonatologists nationally. Multivariable logistic and linear regression models for CF, BO and CS as a function of potential predictors were constructed.
Results:
The survey response rate was 47%. The prevalence of CF, BO and CS was 15.7, 20.8 and 21.9%, respectively. Female gender, emotional depletion, distress from ‘a clinical situation’, ‘co-workers’, ‘personal health issues’ and ‘not talking about distressing issues’ were each significant determinants of CF. Emotional depletion, distress from the ‘physical work environment’ and ‘co-workers’, and ‘not talking about distressing issues’ were significant determinants of BO. Self-identification as Hispanic; ‘not currently feeling distressed’; talking about distressing issues; and utilization of pediatric palliative care services were significant determinants of higher CS.
Conclusions:
CF and BO may impact emotional well-being and professional performance of neonatologists. Enhancement of CS is a potential target for intervention.
Similar content being viewed by others
Introduction
For parents, the unpredictable quotidian life of infants in the neonatal intensive care unit (NICU) is at best emotionally challenging, and at worst, traumatic.1, 2, 3, 4, 5 For NICU professionals, recurrent or chronic occupational exposure to patient and family distress can be emotionally taxing. Compassion fatigue (CF) is emotional distress that can be experienced by caregivers who have ongoing contact with patients who are distressed or traumatized.6, 7, 8 Conceptually, it has been framed as a form of ‘vicarious’ traumatization in which the caregiver experiences post-traumatic stress disorder-like symptoms in response to repeated exposure to the suffering of others.6, 7, 8, 9 CF is not synonymous with burnout (BO), although the two phenomena may coexist. BO is chronic occupational stress that may affect workers in any profession, and is characterized by emotional exhaustion, feelings of depersonalization and career dissatisfaction.10 It has been posited that CF can lead to BO among caregivers.11 Both CF and BO can generate feelings of exhaustion, helplessness, frustration, loneliness, anxiety and depression.12, 13 For physicians, these negative sentiments have the potential to compromise the quality of patient care and patient satisfaction, as well as the mental and physical health of the physicians themselves.12, 13, 14, 15 In contrast to CF and BO, compassion satisfaction (CS) describes the gratification caregivers experience by helping others and the degree to which they feel successful and supported in these professional endeavors.16 As work-related positive and negative sequelae coexist, the net balance of these factors impacts the quality of life of the caregiver.
While the literature about BO in physician is extensive, CF and CS in physicians have not been well studied.17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 By virtue of recurrent occupational exposure to the distress of NICU patients and their families, neonatologists would appear to be at particular risk for CF. To address this issue, we conducted the first national study of these phenomena among US neonatologists. The primary study aims were to determine the prevalence of CF, BO and CS, and to identify potential predictors of these phenomena in this population.
Materials and Methods
Instruments
The Compassion Fatigue and Satisfaction Self-Test for Helpers (CFST) is a 66-item instrument with three subscales to measure the potential for CF, BO and CS.6, 7, 16 The CF subscale assesses work-related exposure of caregivers to patients or clients who have experienced trauma or extremely stressful events, and represents the degree to which the relationship with the client has traumatized the helper.6, 7, 16 The BO subscale assesses feelings of hopelessness and difficulties in dealing with work or in doing one’s job effectively.6, 7, 16 The CS subscale assesses the ability to feel gratified from the role of caregiver.16 The instrument utilizes a 5-point Likert scale (0=never to 5=very often) for respondents to estimate the frequency with which each item occurred in their lives in the previous work week. Convergent and discriminant validity and α reliability have been established for the scales.6, 7, 38 For our current study, the CFST was modified with permission by its author (Figley, personal communication, 2014). The phrasing of statements was modified to more accurately reflect the study participant’s role as a medical caregiver to patients, rather than as a ‘helper’ to a ‘victim’. As such, statements that used the words ‘violence’ or ‘perpetrator’ were removed due to a lack of relevance to the clinical practice of neonatal intensive care. Duplicate statements were removed. Our modified CFST included 54 statements, with 18, 13 and 23 items on the CF, BO and CS subscales, respectively (Supplementary Table S1). In addition to the modified CFST, a 36-item questionnaire was created for self-report of professional details and personal characteristics that were hypothesized to have impact upon development of CF, BO and CS (Supplementary Table S2).
Subjects
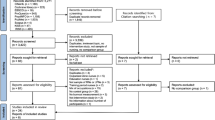
A list of potential participants was generated from the 2011 American Academy of Pediatrics, Section on Perinatal Pediatrics NICUs and Neonatologists of the USA and Canada Directory. The internet website for each program listed in the directory was searched for current faculty listings and e-mail addresses. A short summary of the purpose of the study, as well as a single hyperlink to the modified CFST and questionnaire, were distributed by e-mail via SurveyMonkey. This e-mail was re-sent to non-responders every 2 weeks for a total of five attempts. Individual survey data were collected anonymously by SurveyMonkey without IP addresses or other identifiers.
Data analysis
Individual survey responses were downloaded from SurveyMonkey, coded and entered into SPSS Statistics Version 22 (IBM, Armonk, NY, USA). Subscale scores for CF, BO and CS were summed. For each subscale, reliability was evaluated using Cronbach’s α and normality was assessed by kurtosis, skew and histogram analysis. Subscale scores were analyzed as dichotomous and continuous outcomes. To analyze scores with a binary outcome, we defined the high-end cut point for each subscale. As our instrument was a modification of the original, there were no explicit cutoff values for each scale. To set these, we considered using either a numeric score that was one standard deviation above the mean, or a numeric score greater than the 75th percentile, as have been previously described.16 However, visual inspection of the histogram generated for each subscale revealed a natural high-end cut point that fell between one standard deviation above the mean and the 75th percentile. We chose these natural high-end cut points for each subscale to define CF, BO and high CS for use in analyses of categorical data. Descriptive statistics (means, standard deviations and percentages) were calculated for responses to the CFST and the questionnaire. Pearson’s r and Spearman’s ρ were used as appropriate to examine correlations between subscales and to identify relationships between study variables. Univariate analyses of personal and professional characteristics of respondents’ subscale scores above or below the high-end cut point for CF, BO and CS were compared by χ2 square tests, Fisher’s exact tests or independent t-tests as appropriate. Both multivariable logistic (using score dichotomized at the cut point) and linear regression (using score as a continuous variable) models for CF, BO and CS as a function of potential predictors were constructed. For each model, variables significant at P<0.05 in univariable analyses were added sequentially, and if the model improved significantly (P<0.05) with their inclusion, were retained. Additionally, we conducted principal component analysis and two-step cluster analysis on the 54 items on the modified CFST.
This project was designated as exempt human research by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai.
Results
Of the 1258 study surveys delivered to potential subjects by SurveyMonkey, 593 responses were returned (47.1% response rate). Fifty-two responses were excluded because the respondents were neonatology fellows rather than faculty, and 108 were excluded for an incomplete CFST. This left a final study population of 433 respondents.
The personal and professional characteristics of the study population are presented in Table 1. Most respondents were white, female, lived with a partner or spouse and/or children, and were mid-career or senior level faculty at Level IV institutions. At the time of survey completion, 71% of respondents reported feeling ‘distressed’ about some aspect of their personal or professional lives. Substantial physical exhaustion and emotional depletion were reported by 25.6 and 15.7% of respondents, respectively. The broad range of self-care activities pursued by the study population is listed in Table 1.
Descriptive statistics for the modified CFST are shown in Table 2. Cronbach α-values were 0.91 for CF, 0.83 for BO and 0.93 for CS, which indicated reliable scales that were comparable to the α-values obtained for the original instrument.16 Scores on the three subscales were normally distributed. Relationships between subscale scores and between predictors were investigated using Pearson product moment correlation coefficients and are presented in Supplementary Table S3. A strong positive correlation was identified between CF and BO scores, with a shared variance of 58%. Strong negative correlations were seen between BO and CS scores and between CF and CS scores, with shared variances of 54 and 38%, respectively. Owing to the large shared variance between physical exhaustion and emotional depletion (28%), each of these risk factors was tested separately in all models. The shared variances of other correlated variables were small enough to allow these variables to be tested together in all models. Principal component analysis and two-step cluster analysis did not identify discrete latent profiles in the study population.
The prevalence of CF in the study population was 15.7%. In univariable analyses, individuals at risk for CF were significantly more likely to be female; to report feeling distressed by ‘a clinical situation’, the ‘physical work environment’, ‘co-workers’ or ‘personal health issues’; and to describe substantial recent physical exhaustion and/or emotional depletion. These respondents were also significantly less likely to talk about distressing issues and were more likely to state ‘self-care is not a priority’. The most parsimonious multivariable logistic and linear regression models for CF are presented in Tables 3A and 4A, respectively. Female gender, report of substantial emotional depletion, feelings of distress from ‘a clinical situation’, ‘co-workers’, and ‘personal health issues’, ‘not talking about distressing issues’ as a means of self-care and the statement ‘self-care is not a priority’ remained significant determinants of CF in the multivariable logistic model (Table 3A). When the numeric CF score was modeled by linear regression as a function of significant risk factors, all factors that were significant in the logistic model remained significant predictors, with the exception of the statement ‘self-care is not a priority’ (Table 4A).
The prevalence of BO in the study population was 20.8%. In univariable analyses, predictors for BO were identical to those identified for CF, with the exception of gender. The most parsimonious logistic and linear regression models for BO are presented in Tables 3B and 4B, respectively. Substantial emotional depletion, feelings of distress from the ‘physical work environment’ and ‘co-workers’, and ‘not talking about distressing issues’ remained significant determinants of BO in the multivariable logistic model (Table 3B). When the numeric BO score was modeled by linear regression as a function of significant risk factors, all factors that were significant in the logistic model remained significant predictors (Table 4B).
High CS was identified in 21.9% of the study population. In univariable analyses, highly satisfied respondents were significantly more likely to be male; to self-identify as Hispanic; to have additional family members in their household; to have >10 years of experience as faculty; to have been on call or working in the well-baby nursery as their most recent clinical activity; to report ‘not currently feeling distressed’; and to read as a self-care activity. Respondents with high CS were also significantly less likely to report substantial recent physical exhaustion and/or emotional depletion. The most parsimonious logistic and linear regression models for CS are presented in Tables 3C and 4C, respectively. Self-identification as Hispanic; the presence of additional family members in the household; faculty appointment for >10 years; self-reports of ‘not currently feeling distressed’ and ‘not currently feeling emotionally depleted’; and the most recent clinical activity reported as ‘on call’ remained significant predictors of high compassion satisfaction in the multivariable logistic model (Table 3C). When the numeric CS score was modeled by linear regression as a function of significant risk factors, self-identification as Hispanic; self-report of ‘not currently feeling distressed’; talking about distressing issues as part of self-care; and utilization of pediatric palliative care team services were all significant determinants of higher satisfaction scores (Table 4C). Female gender, substantial recent emotional depletion, and recent performance of a prenatal consult for a family with a fetus at the limits of viability were all significant predictors of lower satisfaction scores (Table 4C).
Discussion
In our national survey of neonatologists, 15.7% of respondents were identified at risk for CF, 20.8% were identified at risk for BO and 21.9% reported high CS using the modified CFST. We present herein the first comprehensive evaluation of potential predictors of these phenomena in neonatologists.
Although CF is recognized as an important cause of emotional distress in caregivers, there are few validated reports about its prevalence in physicians, and none about neonatologists. In a recent systematic review of literature about emotional distress in intensive care health professionals, only seven studies focused solely on physicians, and all explored BO, not CF.39 In studies of mixed populations of pediatric health-care providers that included but were not limited to physicians, the prevalence of CF has been reported at 7.3 to 39%.31, 35
In contrast to CF, BO in physicians has been studied more extensively. Internationally, and across medical specialties, it has been suggested that one-third of physicians will experience BO at some point in their career.21 Higher rates of BO have been reported in pediatric subspecialists than in general pediatricians, with rates as high as 50% in pediatric intensivists.18, 19, 22, 23 The single study assessing BO among neonatologists in Italy reported a prevalence of 30%.17
Comparisons of the prevalence of CF or BO between studies are obfuscated by the different instruments used for assessment. Most published studies of BO in physicians have utilized the Maslach Burnout Inventory.10 The length of this instrument and the expense of administration, however, constrain its usefulness in large samples or in studies with assessments in multiple areas.21 Studies of CF across disciplines, including health care, have used the Professional Quality of Life Scale, the most recent adaptation of the CFST, as the assessment tool.6, 7, 8, 38, 40 Both the Professional Quality of Life Scale and the CFST contain subscales with the potential to assess CF, BO and CS in a single instrument.38, 40 In designing our study instrument, we compared the individual statements of both instruments side-by-side, and felt the CFST, though longer, was the better fit for our screening goals. Since a priori, it was not clear whether CF and BO would be best analyzed by utilizing a binary cutoff score or by a continuum of scores, each subscale was analyzed both ways; the results of both approaches were essentially the same.
We found that more than half the variance in CF in our subjects was accounted for by BO, which may explain why our data did not segregate into discrete latent profiles. As such, it is not surprising that some predictors for CF and BO overlapped (feelings of distress about ‘co-workers’, report of emotional depletion and being less likely to talk about distressing issues as a means of self-care). What emerged as unique predictors of CF in our population were female gender, feelings of distress from a ‘clinical situation’ or ‘personal health issue’, and the reflection that ‘self-care is not a priority’. Of note, prior personal experience of trauma (defined as recent loss of loved one(s), survivor of life-threatening illness, domestic or criminal violence, natural disaster, war or terrorist attack) was not a predictor of CF in our population. For BO, female gender was not identified as a predictor, and the reported feelings of distress were related to the work environment itself. Interestingly, BO was not related to the number of years in clinical practice or objective indices of perceived work demands (i.e. ratio of faculty to size of clinical service, frequency and length of clinical rotations, on call schedules) as have been reported for other intensivists.14, 41
We found a strong negative correlation between CS and CF, and between CS and BO.31, 33, 35, 36, 42, 43 As with our analyses for CF and BO, it was not apparent at the outset whether the optimal approach would be a binary cutoff score or a continuum of scores for evaluation of CS. Although both approaches are presented in Tables 3 and 4, we feel strongly that analysis of CS scores as a continuous variable seems more aligned with human nature. What emerged as unique predictors for higher CS scores were self-identification as Hispanic; report of ‘not currently feeling distressed’; talking about distressing issues as part of self-care; and utilization of pediatric palliative care team services, whereas female gender, substantial recent emotional depletion and recent performance of a prenatal consult for a family with a fetus at the limits of viability were unique predictors of lower satisfaction scores.
Very little has been written about CS in physicians. As a positive occupational corollary, it has been suggested that high CS may be protective against CF and BO, and may therefore be a target for intervention for emotional well-being.16, 44 How can we decrease caregiver distress and enhance satisfaction? Our results suggest that making pediatric palliative care team services available to neonatologists to enrich education about pediatric palliative care principles, and to promote comfort in integration of these principles into day-to-day clinical practice, may be a relatively straightforward intervention for enhancing CS. In addition, our data clearly shows that individuals who talk about their distress have higher CS, and lower CF and BO scores. Therefore, it seems essential to establish an institutional culture in which neonatologists and other NICU staff ‘debrief’ regularly about emotional issues that arise from bearing witness to patient and family suffering.
There are several limitations to our study. Despite a good survey response rate, there is a risk of non-response bias.45 It is impossible to compare variables between those who responded to the survey and those who did not; it may well be that individuals at greatest risk for CF or BO were less likely to participate in the study, or alternatively, the reverse may be true. The generalizability of our findings is limited by the modest sample size and by the fact that the majority of respondents were white and in mid-career or at the senior faculty level. Because of the time frame of self-reflection imposed by the survey instrument, there may have been bias towards more acute symptoms. Owing to the need to limit the survey length, some potentially significant predictors may not have been included. While identified factors accounted for ~30% of the variance in CF, BO and CS scores, two-thirds of the variance in these scores has yet to be explained. Finally, our findings are observed associations to which causality cannot be applied.
In conclusion, CF and BO may profoundly impact the emotional well-being and professional performance of neonatologists. While most physicians are cognizant of BO, this is not necessarily true for CF. In order to provide effective and compassionate patient care, physicians must be able to recognize and reconcile the impact that the suffering of others has on their own psyche. Lack of awareness of unexpressed grief and unresolved distress can allow symptom progression to spiral into multiple other personal and professional problems (e.g., low morale, decreased productivity and quality of care, absenteeism, avoidance, medical errors, stress in personal relationships, substance abuse).6, 7, 8, 12, 14, 25, 26, 27, 41 In light of this, it seems critical that neonatologists and other NICU staff be provided resources and education to promote awareness of this phenomenon and its potential sequelae. It is also incumbent upon us to identify additional modifiable targets in this population to enhance satisfaction as a means to lessening caregiver distress.
References
Davis L, Edwards H, Mohay H, Wollin J . The impact of very premature birth on the psychological health of mothers. Early Hum Dev 2003; 73 (1–2): 61–70.
Kersting A, Dorsch M, Wesselmann U, Lüdorff K, Witthaut J, Ohrmann P et al. Maternal posttraumatic stress response after the birth of a very low-birth-weight-infant. J Psychosom Res 2004; 57: 473–476.
Peebles-Kleiger MJ . Pediatric and neonatal intensive care hospitalization as traumatic stressor: implications for intervention. Bull Menninger Clin 2000; 64: 257–280.
Shaw RJ, Deblois T, Ikudta L, Ginzburg K, Fleisher B, Koopman C . Acute stress disorder among parents of infants in the neonatal intensive care nursery. Psychosomatics 2006; 47: 206–212.
Shaw RJ, Bernard RS, Deblois T, Ikudta L, Ginzburg K, Koopman C . The relationship between acute stress disorder and post-traumatic stress disorder in the neonatal intensive care unit. Psychosomatics 2009; 50: 131–137.
Figley CR . Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in those Who Treat the Traumatized. Taylor & Francis Group: New York, NY, 1995.
Figley CR . Compassion fatigue as secondary traumatic stress disorder: an overview. In: Figley CR (ed). Compassion Fatigue. Brunner/Mazel: New York, NY, 1995, pp 1–20.
Figley CR . Compassion fatigue: toward a new understanding of the costs of caring. In: Stamm BH (ed). Secondary Traumatic Stress: Self-Care Issues for Clinicians, Researchers, and Educators, 2nd edn. Sidran Press: Lutherville, MD, 1999, pp 3–28.
McCann L, Pearlman LA . Vicarious traumatization: a framework for understanding the psychological effects of working with victims. J Trauma Stress 1989; 3: 131–149.
Maslach C, Jackson SE . The measurement of experienced burnout. J Occup Behav 1981; 2: 99–113.
Figley CR . Treating Compassion Fatigue. Brunner-Routledge: New York, NY, 2002.
Kahill S . Interventions for burnout in helping professions: a review of the empirical evidence. Canad J Counsel Rev 1988; 22: 310–342.
Wallace JE, Lemaire JB, Ghali WA . Physician wellness: a missing quality indicator. Lancet 2009; 374: 1714–1721.
Balch CM, Freishlag JA, Shanafelt TD . Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg 2009; 144: 371–376.
Shanafelt TD, Balch CM, Bechamps G, Russell T, Dyrbye L, Satele D et al. Burnout and medical errors among American surgeons. Ann Surg 2009; 251: 995–1000.
Stamm BH . Measuring compassion satisfaction as well as fatigue: developmental history of the compassion satisfaction and fatigue test. In: Figley CR (ed). Treating Compassion Fatigue. Routledge: New York, NY, 2002, pp 107–119.
Bellieni CV, Righetti P, Clampa R, Iacoponi F, Coviello C, Buonocore G . Assessing burnout among neonatologists. J Matern Fetal Neonat Med 2012; 25: 2130–2134.
Garcia TT, Garcia PCR, Molon ME, Piva JP, Tasker RC, Branco RG et al. Prevalence of burnout in pediatric intensivists: an observational comparison with general pediatricians. Pediatr Crit Care Med 2014; 15 (8): e347–e353.
Galvan ME, Vassallo JC, Rodriguez SP, Otero P, Montonati MM, Cardigni G et al. Professional burnout in pediatric intensive care units in Argentina. Arch Argent Pediatr 2012; 110: 466–473.
Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med 2006; 175: 686–692.
Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D et al. Burnout and satisfaction with work-life balance among US physicians relative to the general population. Arch Intern Med 2012; 172: 1377–1385.
Fields A, Cuerdon T, Brasseux CO, Getson PR, Thompson AE, Orlowski SP et al. Physician burnout in pediatric critical care medicine. Crit Care Med 1995; 23: 1425–1429.
Shugerman R, Linzer M, Nelson K, Douglas J, Williams R, Konrad R, for the Career Satisfaction Study Group. Pediatric generalists and subspecialists: determinants of career satisfaction. Pediatrics 2001; 108 (3): E40.
Shanafelt T, Dyrbye L . Oncologist burnout: causes, consequences, and responses. J Clin Oncol 2015; 30: 1235–1241.
Dyrbye LN, Varkey P, Boone SL, Satele DV, Sloan JA, Shanafelt TD . Physician satisfaction and burnout at different career stages. Mayo Clin Proc 2013; 88 (12): 1358–1367.
Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general US population. Acad Med 2014; 89: 443–451.
Spickard A, Gabbe SG, Christensen JF . Mid-career burnout in generalist and specialist physicians. JAMA 2002; 288 (12): 1447–1450.
Curtis JR, Puntillo K . Is there an epidemic of burnout and post-traumatic stress in critical care clinicians? Am J Respir Crit Care Med 2007; 175: 634–636.
Merlani P, Verdon M, Businger A, Domenighetti G, Pargger H, Ricou B, The STRESI+ Group. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med 2011; 184: 1140–1146.
Azoulay E, Herridge M . Understanding ICU burnout: the show must go on. Am J Respir Crit Care Med 2011; 184: 1099–1100.
Robins PM, Meltzer L, Zelikovsky N . The experience of secondary traumatic stress upon care providers working within a children’s hospital. J Pediatr Nurs 2009; 24 (4): 270–279.
Bellolio MF, Cabrera D, Sadosty AT, Hess EP, Campbell RL, Lohse CM et al. Compassion fatigue is similar in emergency medicine residents compared to other medical and surgical specialties. West J Emerg Med 2014; 15 (6): 629–635.
El-bar N, Levy A, Wald HS, Biderman A . Compassion fatigue, burnout and compassion satisfaction among family physicians in the Negev area- a cross-sectional study. Isr J Health Policy 2013; 2: 31–37.
Zeidner M, Hadar D, Matthews G, Roberts RD . Personal factors related to compassion fatigue in health professionals. Anxiety Stress Coping 2013; 26 (6): 595–609.
Meadors P, Lamson A, Swanson M, White M, Sira N . Secondary traumatization in pediatric healthcare providers: compassion fatigue, burnout, and secondary traumatic stress. OMEGA 2009; 60: 103–128.
Meadors P, Lamson A . Compassion fatigue and secondary traumatization: provider self-care on intensive care units for children. J Pediatr Health Care 2008; 22: 24–34.
Dasan S, Gohil P, Cornelius V, Taylor C . Prevalence, causes and consequences if compassion satisfaction and compassion fatigue in emergency care: a mixed-methods study of U.K. NHS consultants. Emerg Med J 2015; 32: 588–594.
Figley CR . Psychometric review of the Compassion Fatigue Self-Test. In: Stamm BH (ed). Measurement of Stress, Trauma, and Adaptation. Sidran Press: Baltimore, MD, 1996, pp 127–130.
van Mol MMC, Kompanje EJO, Benoit DD, Bakker J, Nijkamp MD . The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PLoS One 2015; 10 (8): e0136955.
Stamm BH . The ProQOL 5 [Internet]. [Place unknown]. ProQOL.org; 2009. Available from http://www.proqol.org [updated 2 March 2012].
Balch CM, Shanafelt TD, Sloan J, Satele DV, Kuerer HM . Burnout and career satisfaction among surgical oncologists compared with other surgical subspecialties. Ann Surg Oncol 2011; 18: 16–25.
Sanso N, Galiana L, Oliver A, Pascual A, Sinclair S, Benito E . Palliative care professionals’ inner life: exploring the relationships among awareness, self-care, and compassion satisfaction and fatigue, burnout, and coping with death. J Pain Symptom Manage 2015; 50: 200–207.
Hinderer KA, VonRueden KT, Friedmann E, McQuillan KA, Gilmore R, Kramer B et al. Burnout, compassion fatigue, compassion satisfaction, and secondary traumatic stress in trauma nurses. J Trauma Nurs 2014; 21: 160–169.
Tremblay MA, Messervey D . The Job Demands-Resources Model: Further evidence for the buffering effect of personal resources. SA J Ind Psychol 2011; 37: 10–19.
Cunningham CT, Quan H, Hemmelgarn B, Noseworthy T, Beck CA, Dixon E et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol 2015; 15: 32–39.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Weintraub, A., Geithner, E., Stroustrup, A. et al. Compassion fatigue, burnout and compassion satisfaction in neonatologists in the US. J Perinatol 36, 1021–1026 (2016). https://doi.org/10.1038/jp.2016.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.121
This article is cited by
-
Impact of the SARS-CoV-2 pandemic on pediatric subspecialists’ well-being and perception of workplace value
Pediatric Research (2023)
-
Compassion fatigue, burnout, and compassion satisfaction in pediatric subspecialists during the SARS-CoV-2 pandemic
Pediatric Research (2022)
-
Racial/Ethnic Differences in Burnout: a Systematic Review
Journal of Racial and Ethnic Health Disparities (2022)
-
Maternal and neonatal health care worker well-being and patient safety climate amid the COVID-19 pandemic
Journal of Perinatology (2021)
-
A pilot study exploring interventions for physician distress in pediatric subspecialists
Pediatric Research (2020)