Abstract
Objective:
To determine risk factors for cesarean delivery in nulliparas at labor admission.
Study Design:
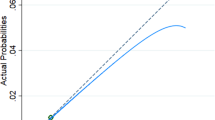
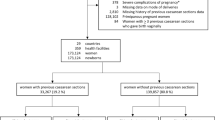
Nulliparas with live-born, singleton gestations ⩾37 weeks in spontaneous or induced labor were analyzed from the Consortium on Safe Labor database in a retrospective observational study. Classification and regression tree (CART) and multivariate logistic regression analysis determined risk factors for cesarean delivery.
Result:
Of the 66 539 nulliparas, 22% had a cesarean delivery. In the CART analysis, the first cervical dilation exam was the first branch followed by body mass index (BMI). Cesarean deliveries occurred in 45%, 25%, 14% and 10% of deliveries at <1 , 1 to 3, 4 and ⩾5 cm dilated, respectively. The BMI influence was most evident in the <1 cm dilation category with 26% of BMI <25 kg m−2 and 66% of BMI ⩾40 kg m−2 having a cesarean delivery. The fewest cesarean deliveries (5%) occurred in those ⩾5 cm and BMI <25 kg m−2. In the multivariate regression analysis, first cervical dilation exam <1 cm (odds ratio (OR) 5.1, 95% confidence interval (CI): 4.5 to 5.7; reference ⩾5 cm) and BMI ⩾40 kg m−2 (OR 5.1, 95% CI: 4.6 to 5.7; reference BMI <25.0 kg m−2) had the highest odds for cesarean delivery.
Conclusion:
Cervical dilation on admission followed by BMI were the two most important risk factors for cesarean delivery identified in both CART and multivariate regression analysis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hamilton BE, Martin JA, Ventura SJ . Births: preliminary data for 2012. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 2013; 62 (3): 1–20.
Coonrod DV, Drachman D, Hobson P, Manriquez M . Nulliparous term singleton vertex cesarean delivery rates: institutional and individual level predictors. Am J Obstet Gynecol 2008; 198 (6): 694 e1–e11; discussion e11.
Makoha FW, Felimban HM, Fathuddien MA, Roomi F, Ghabra T . Multiple cesarean section morbidity. Int J Gynaecol Obstet 2004; 87 (3): 227–232.
Silver RM, Landon MB, Rouse DJ, Leveno KJ, Spong CY, Thom EA et al. Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 2006; 107 (6): 1226–1232.
Eden KB, McDonagh M, Denman MA, Marshall N, Emeis C, Fu R et al. New insights on vaginal birth after cesarean: can it be predicted? Obstet Gynecol 2010; 116 (4): 967–981.
Flamm BL, Geiger AM . Vaginal birth after cesarean delivery: an admission scoring system. Obstet Gynecol 1997; 90 (6): 907–910.
Grobman WA, Lai Y, Landon MB, Spong CY, Leveno KJ, Rouse DJ et al. Development of a nomogram for prediction of vaginal birth after cesarean delivery. Obstet Gynecol 2007; 109 (4): 806–812.
Grobman WA, Terkildsen MF, Soltysik RC, Yarnold PR . Predicting outcome after emergent cerclage using classification tree analysis. Am J Perinatol 2008; 25 (7): 443–448.
Pickhardt MG, Martin JN Jr, Meydrech EF, Blake PG, Martin RW, Perry KG Jr et al. Vaginal birth after cesarean delivery: are there useful and valid predictors of success or failure?. Am J Obstet Gynecol 1992; 166 (6 Part 1): 1811–1815; discussion 1815–1819.
Gregory KD, Korst LM, Platt LD . Variation in elective primary cesarean delivery by patient and hospital factors. Am J Obstet Gynecol 2001; 184 (7): 1521–1532; discussion 1532–1524.
Hamilton EF, Smith S, Yang L, Warrick P, Ciampi A . Third- and fourth-degree perineal lacerations: defining high-risk clinical clusters. Am J Obstet Gynecol 2011; 204 (4): 309 e1–6.
Lu MC, Korst LM, Fridman M, Muthengi E, Gregory KD . Identifying women most likely to benefit from prevention strategies for postpartum hemorrhage. J Perinatol 2009; 29 (6): 422–427.
Zhang J, Landy HJ, Branch DW, Burkman R, Haberman S, Gregory KD et al. Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstet Gynecol 2010; 116 (6): 1281–1287.
Zhang J, Troendle J, Reddy UM, Laughon SK, Branch DW, Burkman R, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol 2010; 203 (4): 326 e1–e10.
Brennan DJ, Murphy M, Robson MS, O'Herlihy C . The singleton, cephalic, nulliparous woman after 36 weeks of gestation: contribution to overall cesarean delivery rates. Obstet Gynecol 2011; 117 (2, Part 1): 273–279.
Heffner LJ, Elkin E, Fretts RC . Impact of labor induction, gestational age, and maternal age on cesarean delivery rates. Obstet Gynecol 2003; 102 (2): 287–293.
Kominiarek MA, Vanveldhuisen P, Hibbard J, Landy H, Haberman S, Learman L et al. The maternal body mass index: a strong association with delivery route. Am J Obstet Gynecol 2010; 203 (3): 264 e1–e7.
Lynch CM, Sexton DJ, Hession M, Morrison JJ . Obesity and mode of delivery in primigravid and multigravid women. Am J Perinatol 2008; 25 (3): 163–167.
Treacy A, Robson M, O'Herlihy C . Dystocia increases with advancing maternal age. Am J Obstet Gynecol 2006; 195 (3): 760–763.
Wilkes PT, Wolf DM, Kronbach DW, Kunze M, Gibbs RS . Risk factors for cesarean delivery at presentation of nulliparous patients in labor. Obstet Gynecol 2003; 102 (6): 1352–1357.
WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser 2000; 894 (i–xii): 1–253.
Oshiro BT, Kowalewski L, Sappenfield W, Alter CC, Bettegowda VR, Russell R et al. A multistate quality improvement program to decrease elective deliveries before 39 weeks of gestation. Obstet Gynecol 2013; 121 (5): 1025–1031.
Fisch JM, English D, Pedaline S, Brooks K, Simhan HN . Labor induction process improvement: a patient quality-of-care initiative. Obstet Gynecol 2009; 113 (4): 797–803.
Reisner DP, Wallin TK, Zingheim RW, Luthy DA . Reduction of elective inductions in a large community hospital. Am J Obstet Gynecol 2009; 200 (6): 674 e1–e7.
Ehrenthal DB, Jiang X, Strobino DM . Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet Gynecol 2010; 116 (1): 35–42.
Darney BG, Snowden JM, Cheng YW, Jacob L, Nicholson JM, Kaimal A et al. Elective induction of labor at term compared with expectant management: maternal and neonatal outcomes. Obstet Gynecol 2013; 122 (4): 761–769.
Stock SJ, Ferguson E, Duffy A, Ford I, Chalmers J, Norman JE . Outcomes of elective induction of labour compared with expectant management: population based study. BMJ 2012; 344: e2838.
Main EK, Moore D, Farrell B, Schimmel LD, Altman RJ, Abrahams C et al. Is there a useful cesarean birth measure? Assessment of the nulliparous term singleton vertex cesarean birth rate as a tool for obstetric quality improvement. Am J Obstet Gynecol 2006; 194 (6): 1644–1651; discussion 1651–1642.
Main EK, Bloomfield L, Hunt G . Development of a large-scale obstetric quality-improvement program that focused on the nulliparous patient at term. Am J Obstet Gynecol 2004; 190 (6): 1747–1756; discussion 1756–1748.
Spong CY . Preventing the First Cesarean Delivery Summary of a Joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal–Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol 2012; 120 (5): 1181–1193.
Acknowledgements
The data included in this paper were obtained from the Consortium on Safe Labor, which was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through Contract No. HHSN267200603425C. Institutions involved in the Consortium include, in alphabetical order: Baystate Medical Center, Springfield, MA; Cedars-Sinai Medical Center Burnes Allen Research Center, Los Angeles, CA; Christiana Care Health System, Newark, DE; Georgetown University Hospital, MedStar Health, Washington, DC; Indiana University Clarian Health, Indianapolis, IN; Intermountain Healthcare and the University of Utah, Salt Lake City, UT; Maimonides Medical Center, Brooklyn, NY; MetroHealth Medical Center, Cleveland, OH; Summa Health System, Akron City Hospital, Akron, OH; The EMMES Corporation, Rockville MD (Data Coordinating Center); University of Illinois at Chicago, Chicago, IL; University of Miami, Miami, FL; and University of Texas Health Science Center at Houston, Houston, TX, USA. The named authors alone are responsible for the views expressed in this manuscript, which does not necessarily represent the decisions or the stated policy of the NICHD.
This study was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, through a contract (Contract No. HHSN267200603425C) for the original Consortium on Safe Labor study; Grant No. K23 HD076010 from the NICHD and NIH (to MK); and University of Illinois at Chicago (UIC) Center for Clinical and Translational Science (CCTS), Award No. UL1RR029879 from the National Center for Research Resources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
This study was presented in part as a poster at the Annual Meeting for the Society of Maternal Fetal Medicine in San Francisco, California on 11 February 2011. Drs Kominiarek, VanVeldhuisen, Gregory and Hibbard all received funding from the NIH/NICHD for the original Consortium on Safe Labor project. Ms Kim and Dr Fridman declare no potential conflict of interest. Dr Kominiarek currently has a K23 Mentored Career Development Award from the NIH/NICHD.
Rights and permissions
About this article
Cite this article
Kominiarek, M., VanVeldhuisen, P., Gregory, K. et al. Intrapartum cesarean delivery in nulliparas: risk factors compared by two analytical approaches. J Perinatol 35, 167–172 (2015). https://doi.org/10.1038/jp.2014.179
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.179
This article is cited by
-
Chorioamnionitis at latent phase more than doubles the risk for cesarean delivery compared to chorioamnionitis at active phase
Archives of Gynecology and Obstetrics (2021)
-
Impact of obesity and other risk factors on labor dystocia in term primiparous women: a case control study
BMC Pregnancy and Childbirth (2018)