Abstract
Objective:
To determine the influence of physiological status and diagnosis at the time of death on end-of-life care.
Study Design:
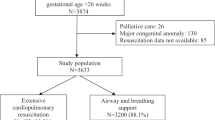
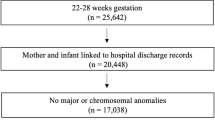
Retrospective descriptive study in a regional referral level IV neonatal intensive care unit (NICU) of infants who died from 1 January 1999 to 31 December 2008. Infants were categorized based on diagnosis (very preterm, congenital anomalies or other) and level of stability. Primary outcome was level of clinical service provided at end of life (care withheld, care withdrawn or full resuscitation).
Result:
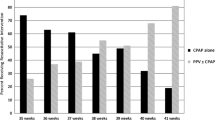
From 1999 to 2008, there were 414 deaths in the NICU. Congenital anomaly was the leading diagnosis at the time of death, representing 45% of all deaths. Comparing mode of death, very preterm newborns were more likely than infants with congenital anomalies to have received cardio-pulmonary resuscitation (CPR) at the time of death (26% vs 13%, P<0.01) and were significantly more unstable (75% vs 52%, P<0.01). Infants aged 22 to 24 weeks were mostly unstable and significantly more likely to receive CPR than infants with any other diagnosis.
Conclusion:
Over the 10-year period, very preterm infants were more likely to be physiologically unstable and to receive CPR at the time of death than infants with any other diagnosis. This finding was especially true for infants at the edge of viability (22 to 24 weeks). These differences in end-of-life care suggest that the quality of life and medical futility may be viewed differently for the least mature infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Weiner J, Sharma J, Kilbride H, Lantos J . How infants die in the neonatal intensive care unit: trends from 1999 through 2008. Arch Pediatr Adolesc Med 2011; 165 (7): 630–634.
Hagen C, Hansen T . Deaths in a neonatal intensive care unit: a 10-year perspective. Ped Crit Care Med 2004; 5 (5): 463–468.
Barton L, Hodgman J . The contribution of withholding or withdrawing care to newborn mortality. Pediatrics 2005; 116: 1487–1491.
Verhagen AA, Janvier A, Leuthner S, Andrews B, Lagatta J, Bos AF et alCategorizing neonatal deaths: a cross-cultural study in the United States, Canada, and The Netherlands. J Pediatr 2010; 07: 1–5.
Adams-Chapman I, Hansen N, Shankaran S, Bell E, Boghossian N, Murray J et alTen year review of major birth defects in VLBW infants. Pediatrics 2013; 132: 49–61.
Stoll B, Hansen N, Bell E, Shankaran S, Laptook A, Walsh M et alNeonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126: 443–456.
Costloe K, Hennessy E, Gibson AT, Marlow N, Wilkinson AR . for the EPICure Study Group. The EPICure Study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics 2000; 106: 659–671.
Saigal S, Rosenbaum PT, Feeny D, Burrows E . Parental perspectives of the health status and health-related quality of life of teen-aged children who were extremely low birthweight and term controls. Pediatrics 2000; 105: 569–574.
Saigal S, Hoult LA, Streiner DL . School difficulties at adolescence in a regional cohort of children who were extremely low birthweight. Pediatrics 2000; 105: 325–331.
Marlow N, Wolke D, Bracewell M, Samara M . Neurologic and developmental diability at six years of age after extremely preterm birth. N Engl J Med 2005; 352: 9–19.
Pierucci RL, Kirby RS, Leuthner SR . End-of-life care for neonates and infants: the experience and effects of a palliative care consultation service. Pediatrics 2001; 108 (3): 653–660.
Institute of Medicine. Approaching Death: Improving Care at the End of Life. National Academy Press: Washington, DC, 1997.
Emanuel EJ, Emanuel LL . The promise of a good death. Lancet 1998; 351 (2): SII21–SII29.
Leuthner SR, Pierucci RL . Experience with neonatal palliative care consultation at the Medical College of Wisconsin-Children's Hospital of Wisconsin. J Palliat Med 2001; 4: 39–47.
American Academy of Pediatrics Committee on Fetus and Newborn. Noninitiation or withdrawal of intensive care for high-risk newborns. Pediatrics 2007; 119: 401–403.
Shah PS . Extensive cardiopulmonary resuscitation for VLBW and ELBW infants: a systematic review and meta-analyses. J Perinatol 2009; 29 (10): 655–661.
Kostelanetz AS, Dhanireddy R . Survival of the very-low-birth-weight infants after cardiopulmonary resuscitation in neonatal intensive care unit. J Perinatol 2004; 24 (5): 279–283.
Catlin A . Transition from curative efforts to purely palliative care for neonates. Adv Neonatal Care 2011; 11 (3): 216–222.
Catlin A . Extremely long hospitalizations of newborns in the United States: data, descriptions, dilemmas. J Perinatol 2006; 26: 742–748.
American Academy of Pediatrics Committee on Fetus and Newborn. Antenatal counseling regarding resuscitation at an extremely low gestational age. Pediatrics 2009; 124 (1): 422–427.
Singh J, Fanaroff J, Andrews B, Caldarelli L, Lagatta J, Plesha-Troyke S et al. Resuscitation in the ‘Gray Zone’ of viability: determining physician preferences and predicting infant outcomes. Pediatrics 2007; 120 (3): 519–526.
Singh J, Lantos J, Meadow W . End-of-life after birth: death and dying in a neonatal intensive care unit. Pediatrics 2004; 114: 1620–1626.
Campbell DE, Fleischman AR . Limits of viability: dilemmas, decisions, and decision makers. A J Perinatol 2001; 18 (3): 117–128.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Weiner, J., Sharma, J., Lantos, J. et al. Does diagnosis influence end-of-life decisions in the neonatal intensive care unit?. J Perinatol 35, 151–154 (2015). https://doi.org/10.1038/jp.2014.170
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.170
This article is cited by
-
Infant mode of death in the neonatal intensive care unit: A systematic scoping review
Journal of Perinatology (2022)
-
Experiences in palliative home care of infants with life-limiting conditions
European Journal of Pediatrics (2016)