Abstract
Objective:
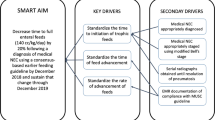
To implement feeding guidelines to reduce advancement time and the incidence of parenteral nutrition-associated liver disease (PNALD) among intestinal surgical infants requiring parenteral nutrition (PN).
Study Design:
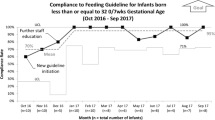
Feeding guidelines with higher initial enteral nutrition (EN) volume and specific advancement criteria were implemented for surgical infants aged <6 months. Preimplementation and postimplementation outcomes were compared.
Results:
There were 57 preimplementation and 33 postimplementation infants. The initial EN volume improved from 10 to 20 ml kg−1 day−1 (P<0.001). Time to reach 50% of goal calories from EN decreased by a median of 6 days (P=0.012) without a change in necrotizing enterocolitis incidence after resuming feeding. PNALD incidence decreased from 70% to 48% (P=0.046), and median peak direct bilirubin (DB) decreased from 5.6 to 2.3 mg dl−1 (P=0.011).
Conclusion:
Feeding guideline implementation with higher initial feeding volume was well tolerated and resulted in faster achievement of 50% goal EN calories. PNALD incidence and peak DB were reduced.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Goulet O, Olieman J, Ksiazyk J, Spolidoro J, Tibboe D, Kohler H et al. Neonatal short bowel syndrome as a model of intestinal failure: Physiological background for enteral feeding. Clin Nutr 2012; 32 (2): 162–171.
Barclay AR, Beattie LM, Weaver LT, Wilson DC . Systematic review: medical and nutritional interventions for the management of intestinal failure and its resultant complications in children. Aliment Pharmacol Ther 2011; 33 (2): 175–184.
Squires RH, Duggan C, Teitelbaum DH, Wales PW, Balint J, Venick R et al. Natural history of pediatric intestinal failure: initial report from the Pediatric Intestinal Failure Consortium. J Pediatr 2012; 161 (4): 723.e2–728.e2.
Drongowski RA, Coran AG . An analysis of factors contributing to the development of total parenteral nutrition-induced cholestasis. JPEN J Parenter Enteral Nutr 1989; 13 (6): 586–589.
Kelly DA . Intestinal failure-associated liver disease: what do we know today? Gastroenterology 2006; 130 (2 Suppl 1): S70–S77.
Kaufman SS, Pehlivanova M, Fennelly EM, Rekhtman YM, Gondolesi GE, Little CA et al. Predicting liver failure in parenteral nutrition-dependent short bowel syndrome of infancy. J Pediatr 2010; 156 (4): 580–5 e1.
Kurvinen A, Nissinen MJ, Gylling H, Miettinen TA, Lampela H, Koivusalo AI et al. Effects of long-term parenteral nutrition on serum lipids, plant sterols, cholesterol metabolism, and liver histology in pediatric intestinal failure. J Pediatr Gastroenterol Nutr 2011; 53 (4): 440–446.
Goulet O, Ruemmele F . Causes and management of intestinal failure in children. Gastroenterology 2006; 130 (2 Suppl 1): S16–S28.
Duro D, Mitchell PD, Kalish LA, Martin C, McCarthy M, Jaksic T et al. Risk factors for parenteral nutrition-associated liver disease following surgical therapy for necrotizing enterocolitis: a Glaser Pediatric Research Network Study [corrected]. J Pediatr Gastroenterol Nutr 2011; 52 (5): 595–600.
Javid PJ, Malone FR, Reyes J, Healey PJ, Horslen SP . The experience of a regional pediatric intestinal failure program: Successful outcomes from intestinal rehabilitation. Am J Surg 2010; 199 (5): 676–679.
Neu J, Mihatsch WA, Zegarra J, Supapannachart S, Ding ZY, Murguia-Peniche T . Intestinal mucosal defense system, Part 1. Consensus recommendations for immunonutrients. J Pediatr 2013; 162 (3 Suppl): S56–S63.
Shores DR, Bullard JE, Aucott SW, Stewart FD, Haney C, Nonyane BAS et al. Analysis of nutrition practices and intestinal failure-associated liver disease in infants with intestinal surgery. Infant Child Adolesc Nutr 2015; 7 (1): 29–37.
Javid PJ, Malone FR, Dick AA, Hsu E, Sunseri M, Healey P et al. A contemporary analysis of parenteral nutrition-associated liver disease in surgical infants. J Pediatr Surg 2011; 46 (10): 1913–1917.
Leaf A, Dorling J, Kempley S, McCormick K, Mannix P, Linsell L et al. Early or delayed enteral feeding for preterm growth-restricted infants: a randomized trial. Pediatrics 2012; 129 (5): e1260–e1268.
Wales PW, Allen N, Worthington P, George D, Compher C, Teitelbaum D . A.S.P.E.N. clinical guidelines: support of pediatric patients with intestinal failure at risk of parenteral nutrition-associated liver disease. JPEN J Parenter Enteral Nutr 2014; 38 (5): 538–557.
Fallon EM, Nehra D, Potemkin AK, Gura KM, Simpser E, Compher C et al. A.S.P.E.N. clinical guidelines: nutrition support of neonatal patients at risk for necrotizing enterocolitis. JPEN J Parenter Enteral Nutr 2012; 36 (5): 506–523.
Rudolph JA, Squires R . Current concepts in the medical management of pediatric intestinal failure. Curr Opin Organ Transplant 2010; 15 (3): 324–329.
Gosselin KB, Duggan C . Enteral nutrition in the management of pediatric intestinal failure. J Pediatr 2014; 165 6: 1085–1090.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG . Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009; 42 (2): 377–381.
Perla RJ, Provost LP, Murray SK . The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf 2011; 20 (1): 46–51.
Willis TC, Carter BA, Rogers SP, Hawthorne KM, Hicks PD, Abrams SA . High rates of mortality and morbidity occur in infants with parenteral nutrition-associated cholestasis. JPEN J Parenter Enteral Nutr 2010; 34 (1): 32–37.
Hans DM, Pylipow M, Long JD, Thureen PJ, Georgieff MK . Nutritional practices in the neonatal intensive care unit: analysis of a 2006 neonatal nutrition survey. Pediatrics 2009; 123 (1): 51–57.
van Elburg RM, Neu J . Nutrition support of neonatal patients at risk for necrotizing enterocolitis: response to Fallon et al (2012). JPEN J Parenter Enteral Nutr 2013; 37 (1): 11.
Stanger JD, Oliveira C, Blackmore C, Avitzur Y, Wales PW . The impact of multi-disciplinary intestinal rehabilitation programs on the outcome of pediatric patients with intestinal failure: a systematic review and meta-analysis. J Pediatr Surg 2013; 48 (5): 983–992.
Kirby RS, Marshall J, Tanner JP, Salemi JL, Feldkamp ML, Marengo L et al. Prevalence and correlates of gastroschisis in 15 states, 1995 to 2005. Obstet Gynecol 2013; 122 (2 Pt 1): 275–281.
Cober MP, Killu G, Brattain A, Welch KB, Kunisaki SM, Teitelbaum DH . Intravenous fat emulsions reduction for patients with parenteral nutrition-associated liver disease. J Pediatr 2012; 160 (3): 421–427.
Nehra D, Fallon EM, Carlson SJ, Potemkin AK, Hevelone ND, Mitchell PD et al. Provision of a soy-based intravenous lipid emulsion at 1 g/kg/d does not prevent cholestasis in neonates. JPEN J Parenter Enteral Nutr 2013; 37 (4): 498–505.
Acknowledgements
We thank Jennifer Shepard who assisted with data collection, and other team members who assisted in implementation: Howard Pryor, MD, Daniel Rhee, MD, Karen Frank, DNP, Beth Diehl-Svrjcek, NP, and Lynn Morooney, NP. This publication was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR), which is funded in part by Grant Number 1KL2TR001077-01 from the National Center of Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTAR, NCATS or NIH. This project was also partially funded by The Thomas Wilson Sanitarium for the Children of Baltimore City.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shores, D., Bullard, J., Aucott, S. et al. Implementation of feeding guidelines in infants at risk of intestinal failure. J Perinatol 35, 941–948 (2015). https://doi.org/10.1038/jp.2015.105
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.105
This article is cited by
-
Dilemmas in establishing preterm enteral feeding: where do we start and how fast do we go?
Journal of Perinatology (2023)