Abstract
Objective:
To test whether implementing a nursing-driven comfort protocol standardizes morphine use in one neonatal intensive care unit (NICU) and to examine how non-standard morphine (N-SM) relates to days of ventilation, days of total parenteral nutrition (TPN) and length of stay (LOS).
Study Design:
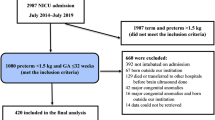
This was a retrospective/prospective observational study using pharmacy records, medical records, and an outcomes database. Comfort protocol implementation began February 2011 and was applied to preterm, ventilated neonates <1500 grams. Pre- and post-implementation proportions of N-SM days were compared using the binomial test. A percent ‘P’-chart spanning 30 quarters was constructed with statistical-process control analysis. Multivariable linear regression adjusting for acuity assessed the relationship between N-SM use and days of ventilation, TPN and LOS.
Result:
Hundred and thirty-four patients met inclusion criteria, 116 prior to and 18 after implementation. The proportion of patients given N-SM for one or more days decreased from 59 to 35% after protocol implementation (P=0.017). A 9-month period of decreased N-SM days was observed after protocol implementation. Controlling for acuity, each additional day of N-SM use was associated with 0.47 more days of ventilation (95% confidence interval (CI): 0.26–0.69, P<0.001) and 0.52 more days of TPN (95% CI: 0.35–0.68, P<0.001). Exposure to N-SM was associated with 17 additional days of hospitalization (P=0.009, 95% CI: 4.5–30).
Conclusion:
Implementing a nursing-driven comfort protocol significantly reduced N-SM use. N-SM in the NICU is negatively associated with key clinical outcomes. Testing similar protocols in other settings is warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Anand KJ, Brown MJ, Causon RC, Christofides ND, Bloom SR, Aynsley-Green A . Can the human neonate mount an endocrine and metabolic response to surgery? J Pediatr Surg 1985; 20 (1): 41–48.
Anand KJ, Hall RW . Controversies in neonatal pain: an introduction. Semin Perinatol 2007; 31 (5): 273–274.
Stevens B, Johnston C, Petryshen P, Taddio A . Premature infant pain profile: development and initial validation. Clin J Pain 1996; 12 (1): 13–22.
Stevens B, Johnston C, Taddio A, Gibbins S, Yamada J . The premature infant pain profile: evaluation 13 years after development. Clin J Pain 2010; 26 (9): 813–830.
Stevens B, Craig K, Johnston C, Harrison D, Ohlsson A . Oral sucrose for procedural pain in infants. Lancet 2011; 377 (9759): 25–26.
Meek J, Huertas A . Cochrane review: non-nutritive sucking, kangaroo care and swaddling/facilitated tucking are observed to reduce procedural pain in infants and young children. Evid Based Nurs 2012; 15 (3): 84–85.
Bellu R, de Waal K, Zanini R . Opioids for neonates receiving mechanical ventilation: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2010; 95 (4): F241–F251.
Anand KJ, Aranda JV, Berde CB, Buckman S, Capparelli EV, Carlo W et al. Summary proceedings from the neonatal pain-control group. Pediatrics 2006; 117 (3 Pt 2): S9–S22.
Simons SH, van Dijk M, van Lingen RA, Roofthooft D, Duivenvoorden HJ, Jongeneel N et al. Routine morphine infusion in preterm newborns who received ventilatory support: a randomized controlled trial. JAMA 2003; 290 (18): 2419–2427.
Anand KJ, Hall RW, Desai N, Shephard B, Bergqvist LL, Young TE et al. Effects of morphine analgesia in ventilated preterm neonates: primary outcomes from the NEOPAIN randomised trial. Lancet 2004; 363 (9422): 1673–1682.
de Graaf J, van Lingen RA, Simons SH, Anand KJ, Duivenvoorden HJ, Weisglas-Kuperus N et al. Long-term effects of routine morphine infusion in mechanically ventilated neonates on children's functioning: five-year follow-up of a randomized controlled trial. Pain 2011; 152 (6): 1391–1397.
de Graaf J, van Lingen RA, Valkenburg AJ, Weisglas-Kuperus N, Groot Jebbink L, Wijnberg-Williams B et al. Does neonatal morphine use affect neuropsychological outcomes at 8 to 9years of age? Pain 2013; 154 (3): 449–458.
Thewissen L, Allegaert K . Analgosedation in neonates: do we still need additional tools after 30 years of clinical research? Arch Dis Child Educ Pract Ed 2011; 96 (3): 112–118.
Sharek PJ, Powers R, Koehn A, Anand KJ . Evaluation and development of potentially better practices to improve pain management of neonates. Pediatrics 2006; 118 (Suppl 2): S78–S86.
Stevens B, Riahi S, Cardoso R, Ballantyne M, Yamada J, Beyene J et al. The influence of context on pain practices in the NICU: perceptions of health care professionals. Qual Health Res 2011; 21 (6): 757–770.
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30 (1): 119–141.
Grant MJ, Scoppettuolo LA, Wypij D, Curley MA . Prospective evaluation of sedation-related adverse events in pediatric patients ventilated for acute respiratory failure. Crit Care Med 2012; 40 (4): 1317–1323.
Durrmeyer X, Vutskits L, Anand KJ, Rimensberger PC . Use of analgesic and sedative drugs in the NICU: integrating clinical trials and laboratory data. Pediatr Res 2010; 67 (2): 117–127.
Ng E, Taddio A, Ohlsson A . Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev 2012; 6: CD002052.
Holsti L, Grunau RE . Initial validation of the behavioral indicators of infant pain (BIIP). Pain 2007; 132 (3): 264–272.
Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W et al. Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med 1999; 27 (12): 2609–2615.
Deeter KH, King MA, Ridling D, Irby GL, Lynn AM, Zimmerman JJ . Successful implementation of a pediatric sedation protocol for mechanically ventilated patients. Crit Care Med 2011; 39 (4): 683–688.
Lenfant C . Shattuck lecture—clinical research to clinical practice—lost in translation? N Engl J Med 2003; 349 (9): 868–874.
Horbar JD, Plsek PE, Leahy K . NIC/Q 2000: establishing habits for improvement in neonatal intensive care units. Pediatrics 2003; 111 (4 Pt 2): e397-410.
Curtis JR, Cook DJ, Wall RJ, Angus DC, Bion J, Kacmarek R et al. Intensive care unit quality improvement: a ‘how-to’ guide for the interdisciplinary team. Crit Care Med 2006; 34 (1): 211–218.
Menon G, Boyle EM, Bergqvist LL, McIntosh N, Barton BA, Anand KJ . Morphine analgesia and gastrointestinal morbidity in preterm infants: secondary results from the NEOPAIN trial. Arch Dis Child Fetal Neonatal Ed 2008; 93 (5): F362–F367.
Bhandari V, Bergqvist LL, Kronsberg SS, Barton BA, Anand KJ . Morphine administration and short-term pulmonary outcomes among ventilated preterm infants. Pediatrics 2005; 116 (2): 352–359.
Hall RW, Kronsberg SS, Barton BA, Kaiser JR, Anand KJ . Morphine, hypotension, and adverse outcomes among preterm neonates: who's to blame? Secondary results from the NEOPAIN trial. Pediatrics 2005; 115 (5): 1351–1359.
Boyle EM, Freer Y, Wong CM, McIntosh N, Anand KJ . Assessment of persistent pain or distress and adequacy of analgesia in preterm ventilated infants. Pain 2006; 124 (1-2): 87–91.
Carbajal R, Rousset A, Danan C, Coquery S, Nolent P, Ducrocq S et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA 2008; 300 (1): 60–70.
Grunau RE, Whitfield MF, Petrie-Thomas J, Synnes AR, Cepeda IL, Keidar A et al. Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain 2009; 143 (1-2): 138–146.
Acknowledgements
The authors would like to acknowledge the nursing staff and leadership at the University of Washington Medical Center for their willingness to adapt their clinical practice and the faculty in the Division of Neonatology for their ongoing mentorship and flexibility with this project. Funding for this study was provided by a grant from the University of Washington, Department of Pediatrics, Division of Neonatology Neonatal Bioresearch Fund, which was used to help with statistical analytic support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fleishman, R., Zhou, C., Gleason, C. et al. Standardizing morphine use for ventilated preterm neonates with a nursing-driven comfort protocol. J Perinatol 35, 46–51 (2015). https://doi.org/10.1038/jp.2014.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.131
This article is cited by
-
Reduced narcotic and sedative utilization in a NICU after implementation of pain management guidelines
Journal of Perinatology (2017)