Abstract
Objective:
Intraventricular reservoirs (IVRs) are used to drain cerebrospinal fluid (CSF) in neonates with post-hemorrhagic ventricular dilatation (PHVD). The objectives of this case–control study were to evaluate changes in CSF parameters in serial IVR taps and to compare CSF parameters in culture-positive and -negative specimens.
Study Design:
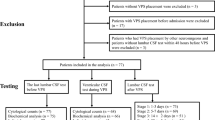
Clinical and laboratory data from serial (up to 7) reservoir taps at 5- to 8-day intervals were collected on preterm neonates with PHVD and IVR insertion.
Result:
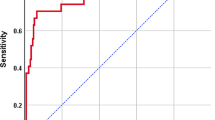
The median (range) gestational age and birth weight of our cohort (n=52) was 26 (23 to 33) weeks and 796 (450 to 1620) grams. Significant decreases in percentage of CSF neutrophils and protein were noted in later taps, compared with the first tap at insertion of IVR. Five (9.6%) infants had positive CSF cultures on 10 occasions. Compared with negative specimens (n=266), the mean (s.d.) proportion of neutrophils in CSF (55% (33) vs 26% (23)) was significantly higher and ratio of CSF to serum glucose significantly lower (0.19 (0.08) vs 0.29 (0.13)) in culture-positive specimens (n=10). The area under the curve was 0.82 (95% confidence interval (CI) 0.72 to 0.93) for CSF white blood cell (WBC) count, 0.79 (95% CI 0.68 to 0.90) for CSF protein and 0.75 (95% CI 0.56 to 0.95) for percentage of neutrophils. The sensitivities and specificities for diagnosis of infection was 90 and 63% for CSF WBC count > 42 mm–3, 89 and 58% for CSF protein at > 250 mg dl–1 and 80 and 67% for CSF neutrophil proportion >31.5%.
Conclusion:
CSF parameters from IVR taps, specifically proportion of neutrophils and proteins are higher at insertion and progressively normalize over time. Although they vary widely, CSF WBC, protein and neutrophil proportion using higher cut-off values have good sensitivity in the diagnosis of infection.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Persson EK, Hagberg G, Uvebrant P . Hydrocephalus prevalence and outcome in a population-based cohort of children born in 1989–1998. Acta Paediatr 2005; 94: 726–732.
Whitelaw A, Cherian S, Thoresen M, Pople I . Posthaemorrhagic ventricular dilatation: new mechanics and new treatment. Acta Paediatr Suppl 2004; 444: 11–14.
Murphy BP, Inder TE, Rooks V, Taylor GA, Anderson NJ, Mogridge N et al. Posthaemorrhagic ventricular dilatation in the preterm infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed 2002; 87: F37–F41.
Dykes FD, Dunbar B, Lazarra A, Ahmann PA . hydrocephalus in high-risk preterm infants: natural history, management, and long-term outcome. J Pediatr 1989; 114: 611–618.
Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R, NICHD Research Network. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 2008; 2: e1167–e1177.
Resch B, Gedermann A, Maurer U, Ritschl E, Müller W . Neurodevelopmental outcome of hydrocephalus following intra-/periventricular hemorrhage in preterm infants: short- and long-term results. Childs Nerv Syst 1996; 12: 27–33.
Shooman D, Portess H, Sparrow O . A review of the current treatment methods for posthaemorrhagic hydrocephalus of infants. Cerebrospinal Fluid Res 2009; 6: 1.
Whitelaw A, Kennedy CR, Brion LP . Diuretic therapy for newborn infants with posthemorrhagic ventricular dilatation. Cochrane Database Syst Rev 2001; 2: CD002270.
International PHVD Drug Trial Group. International randomized controlled trial of acetazolamide and furosemide in posthaemorrhagic ventricular dilatation in infancy. Lancet 1998; 352: 433–440.
Hudgins RJ, Boydston WR, Gilreath CL . Treatment of posthemorrhagic hydrocephalus in the preterm infant with a ventricular access device. Pediatr Neurosurg 1998; 29: 309–313.
Gaskill SJ, Marlin AE, Rivera S . The subcutaneous ventricular reservoir: an effective treatment for posthemorrhagic hydrocephalus. Childs Nerv Syst 1988; 4: 291–295.
Richard E, Cinalli G, Assis D, Pierre-Kahn A, Lacaze-Masmonteil T . Treatment of post-haemorrhage ventricular dilatation with an Ommaya′s reservoir: management and outcome of 64 preterm infants. Childs Nerv Syst 200; 17: 334–340.
Brouwer AJ, Groenendaal F, van den Hoogen A, Verboon-Maciolek M, Hanlo P, Rademaker KJ et al. Incidence of infections of ventricular reservoirs in the treatment of post-haemorrhagic ventricular dilatation: a retrospective study (1992–2003). Arch Dis Child Fetal Neonatal Ed 2007; 92: F41–F43.
Lenfestey RW, Smith PB, Moody MA, Clark RH, Cotten CM, Seed PC et al. Predictive value of cerebrospinal fluid parameters in neonates with intraventricular drainage devices. J Neurosurg 2007; 107: 209–212.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage:a study of infants with birth weights less than 1500 gm. J Pediatr 1978; 92: 529–534.
Berman RE, Kliegman RM, Arvin AM . Nelson Textbook of Pediatrics. 17th edn WB Saunders: Philadelphia, PA, 2004.
Oski FA . Principles and Practice of Pediatrics. 2nd edn. JB Lippincott: Philadelphia, PA, 1994.
Ahmed A, Hickey SM, Ehrett S, llo M, Brito F, Goto C et al. Cerebrospinal fluid values in the term neonate. Pediatr Infect Dis J 1996; 15: 298–303.
Garges HP, Moody MA, Cotten CM, Smith PB, Tiffany KF, Lenfestey R et al. Neonatal meningitis: what is the correlation among cerebrospinal fluid cultures, blood cultures, and cerebrospinal fluid parameters? Pediatrics 2006; 117: 1094–1100.
Wiswell TE, Baumgart S, Gannon CM, Spitzer AR . No lumbar puncture in the evaluation for early neonatal sepsis: will meningitis be missed? Pediatrics 1995; 119: 803–806.
Stoll BJ, Hansen N, Fanaroff AA, Wright LL, Carlo WA, Ehrenkranz RA et al. To tap or not to tap: high likelihood of meningitis without sepsis among very low birth weight infants. Pediatrics 2004; 113: 1181–1186.
Baumeister FA, Pohl-Koppe A, Hofer M, Kim JO, Weiss M . IL-6 in CSF during ventriculitis in preterm infants with posthemorrhagic hydrocephalus. Infection 2000; 28: 234–236.
Scribano PV, Pool S, Smally AJ . Comparison of ventriculoperitoneal shunt tap and lumbar puncture in a child with meningitis. Pediatr Emerg Care 2002; 18: E1–E3.
Acknowledgements
We would like to thank Dr Seetha Shankaran for her guidance in the preparation of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bajaj, M., Lulic-Botica, M. & Natarajan, G. Evaluation of cerebrospinal fluid parameters in preterm infants with intraventricular reservoirs. J Perinatol 32, 786–790 (2012). https://doi.org/10.1038/jp.2011.190
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.190
Keywords
This article is cited by
-
Ventricular access device infection rate: a retrospective study and review of the literature
Child's Nervous System (2014)