Abstract
Objective:
To analyze the levels of regional tissue oxygenation in preterm infants in association with echocardiographically significant patent ductus arteriosis (PDA).
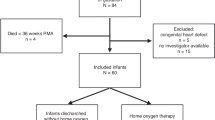
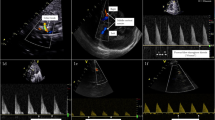
Study Design:
Preterm infants with gestational age less than 32 week were enrolled before the first dose of the pharmacological treatment for the PDA. Non-invasive near-infrared spectroscopy (NIRS) technology was utilized to measure cerebral (rSO2-C), renal (rSO2-R) and mesenteric (rSO2-M) tissue oxygenation for approximately 60 min. Regional fractional oxygen extraction (FOE) was calculated using simultaneously measured arterial saturation (SaO2). We analyzed regional tissue oxygenation and oxygen extraction, hemodynamic parameters, and demographic and clinical information in association with the size of the PDA (moderate vs large).
Result:
Among the 38 enrolled infants, the majority were diagnosed with a large (63.2%, n=24) and the rest with a moderate-sized PDA. Infants with large and moderate PDA were comparable in terms of gestational age, study age and weight, mode of delivery and hemodynamic parameters. A significantly higher proportion of infants with a moderate PDA were mechanically ventilated as compared with those with a large PDA. We found no significant differences in the rSO2-C and rSO2-R, irrespective of the type of respiratory support. However, in infants with a large PDA on continuous nasal positive airway pressure (NCPAP), the rSO2-M was lower and mesenteric FOE was higher than that in mechanically ventilated neonates with a large PDA, and in those with moderate PDA irrespective of the type of respiratory support.
Conclusion:
The PDA size did not affect cerebral and renal tissue oxygenation, but the mesenteric tissue oxygenation was decreased in infants with a large PDA on NCPAP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Markham M . Patent ductus arteriosus in the premature infant: a clinical dilemma. Newborn Infant Nurs Rev 2006; 6: 151–157.
Evans N, Iyer P . Assessment of ductus arteriosus shunt in preterm infants supported by mechanical ventilation: effect of inter-atrial shunting. J Pediatr 1994; 125: 778–785.
Reese J . Death, dying, and exhaustion in the ductus arteriosus: prerequisites for permanent closure. Editorial Focus. Am J Physiol Regul Integr Comp Physiol 2006; 290: R357–R358.
Agarwal R, Deorari AK, Paul VK . Patent ductis arteriosus in preterm neonates. Indian J Pediatr 2008; 75: 277–280.
Lipman B, Serwer GA, Brazy JE . Abnormal cerebral hemodynamics in preterm infants with patent ductus arteriosus. Pediatrics 1982; 69: 778–781.
Kluckow M, Evans N . Early echocardiographic prediction of symptomatic patent ductus arteriosus in preterm infants undergoing mechanical ventilation. J Pediatr 1995; 127: 774–779.
Evans N, Iyer P . Longitudinal changes in the diameter of the ductus arteriosus in ventilated preterm infants: correlation with respiratory outcomes. Arch Dis Childhood 1995; 72: F156–F161.
McNamara PJ, Sehgal A . Toward rational management of the ductus arteriosus: the need for disease staging. Arch Dis Child Fetal Neonatal Ed 2007; 92: F424–F427.
Petrova A, Mehta R . Near-infrared spectroscopy in the detection of regional tissue oxygenation during hypoxic events in preterm infants undergoing critical care. Pediatr Crit Care Med 2006; 7: 449–454.
Hoffman GM, Stuth EA, Jaquiss RD, Vanderwal PL, Staudt SR, Troshynski TJ et al. Changes in cerebral and somatic oxygenation during stage 1 palliation of hypoplastic left heart syndrome using continuous regional cerebral perfusion. J Thorac Cardiovasc Surg 2004; 127: 223–233.
Varela JE, Cohn SM, Giannotti GD, Dolich MO, Ramon H, Wiseberg JA et al. Near-infrared spectroscopy reflects changes in mesenteric and systemic perfusion during abdominal compartment syndrome. Surgery 2001; 129: 363–370.
Kocsis L, Herman P, Eke A . Mathematical model for the estimation of hemodynamic and oxygenation variables by tissue spectroscopy. J Theor Biol 2006; 241: 262–275.
Kleinman CS, Seri I, Victor S, Weindling MA . Near-infrared spectroscopy and its use for the assessment of tissue perfusion in the neonates. In: Kleinman CS, Seri I (eds). Hemodynamics and Cardiology. Elsevier Health Sciences: Philadephia, PA, 2008, pp 111–130.
Boushel R, Langberg H, Olesen J, Gonzales-Alonzo J, Bülow J, Kjaer M . Monitoring tissue oxygen availability with near infrared spectroscopy (NIRS) in health and disease. Scand J Med Sci Sports 2001; 11: 213–222.
Franceschini MA, Boas DA, Zourabian A, Diamond SG, Nadgir S, Lin DW et al. Near-infrared spirometry: noninvasive measurements of venous saturation in piglets and human subjects. J Appl Physiol 2002; 92: 372–384.
Abdul-Khaliq H, Troitzsch D, Berger F, Lange PE . Regional transcranial oximetry with near infrared spectroscopy (NIRS) in comparison with measuring oxygen saturation in the jugular bulb in infants and children for monitoring cerebral oxygenation. Biomed Technol (Berl) 2000; 45: 328–332.
Bay-Hansen R, Elfving B, Greisen G . Use of near infrared spectroscopy for estimation of peripheral venous saturation in newborns: comparison with co-oximetry of central venous blood. Biol Neonate 2002; 82: 1–8.
Wickramasinghe YA, Livera LN, Spencer SA, Rolfe P, Thorniley MS . Plethysmographic validation of near infrared spectroscopic monitoring of cerebral blood volume. Arch Dis Child 1992; 67: 407–411.
Tichauer KM, Brown DW, Hadway J, Lee TY, St Lawrence K . Near-infrared spectroscopy measurements of cerebral blood flow and oxygen consumption following hypoxia–ischemia in newborn piglets. J Appl Physiol 2006; 100: 850–857.
Kaufman J, Almodovar MC, Zuk J, Friesen RH . Correlation of abdominal site near-infrared spectroscopy with gastric tonometry in infants following surgery for congenital heart disease. Pediatr Crit Care Med 2008; 9: 62–68.
Petros AJ, Heys R, Tasker RC, Fortune PM, Roberts I, Kiely E . Near infrared spectroscopy can detect changes in splanchnic oxygen delivery in neonates during apnoeic episodes. Eur J Pediatr 1999; 158: 173–174.
Fortune PM, Wagstaff M, Petros AJ . Cerebro-splanchnic oxygenation ratio (CSOR) using near infrared spectroscopy may be able to predict splanchnic ischaemia in neonates. Intens Care Med 2001; 27: 1401–1407.
Wardle SP, Yoxall CW, Weindling AM . Determinants of cerebral fractional oxygen extraction using near infrared spectroscopy in preterm neonates. J Cereb Blood Flow Metab 2000; 20: 272–279.
Owen-Reece H, Smith M, Elwell CE, Goldstone JC . Near infrared spectroscopy. Br J Anaesth 1999; 82: 418–426.
Poets CF, Stebbens VA, Alexander JR, Arrowsmith WA, Salfield SA, Southall DP . Arterial oxygen saturation in preterm infants at discharge from the hospital and six weeks later. J Pediatr 1992; 120: 447–454.
Martin RM, Abu-Shaweesh JM, Baird MT . Apnea of prematurity. Pediatr Resp Rev 2004; 5: S377–S382.
Miall-Allen VM, de Vries LS, Whitelaw AG . Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child 1987; 62: 1068–1069.
Schears G, Schultz SE, Creed J, Greeley WJ, Wilson DF, Pastuszko A . Effect of perfusion flow rate on tissue oxygenation in newborn piglets during cardiopulmonary bypass. Ann Thorac Surg 2003; 75: 560–565.
Havranek T, Thompson Z, Carver JD . Factors that influence mesenteric artery blood flow velocity in newborn preterm infants. J Perinatol 2006; 26: 493–497.
Havranek T, Madramootoo C, Carver JD . Nasal continuous positive airway pressure affects pre- and postprandial intestinal blood flow velocity in preterm infants. J Perinatol 2007; 27: 704–708.
Loick HM, Tokyay R, Abdi S, Traber DL, Nichols RJ, Herndon DL . Halothane markedly reduces mesenteric blood flow but does not impair gut mucosal oxygenation in pigs. Eur J Pharmacol 1991; 16: 91–96.
Cortez J, Gupta M, Amaram A, Pizzino J, Sawhney M, Sood BG . Noninvasive evaluation of splanchnic tissue oxygenation using near-infrared spectroscopy in preterm neonates. J Matern Fetal Neonatal Med 2010 (e-pub ahead of print).
McNeill S, Gatenby JC, McElroy S, Engelhardt B . Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J Perinatol 2010; 31: 51–57.
Lemmers PM, Toet MC, van Bel F . Impact of patent ductus arteriosus and subsequent therapy with indomethacin on cerebral oxygenation in preterm infants. Pediatrics 2008; 121: 142–147.
Zaramella P, Freato F, Quaresima V, Ferrari M, Bartocci M, Rubino M et al. Surgical closure of patent ductus arteriosus reduces the cerebral tissue oxygenation index in preterm infants: a near-infrared spectroscopy and Doppler study. Pediatr Int 2006; 48: 305–312.
Naulaers G, Morren G, Van Huffel S, Casaer P, Devlieger H . Measurement of tissue oxygenation index during the first three days in premature born infants. Adv Exp Med Biol 2003; 510: 379–383.
Kishi K, Kawaguchi M, Yoshitani K, Nagahata T, Furuya H . Influence of patient variables and sensor location on cerebral oxygen saturation measured by INVOS 4100 near-infrared spectrophotometers. J Neurosurg Anesthesiol 2003; 4: 302–306.
Vanderhaegen J, Dehing L, Naulaers G, Devlieger H, Al-Olayet Y, Penninckx F et al. Use of the liver tissue oxygenation index as a noninvasive parameter of intestinal ischemia in rabbits. World J Surg 2007; 31: 2359–2362El.
Desoky E, Seifalian A, Cope M, Delpy D, Davidson B . Changes in tissue oxygenation of the porcine liver measured by near-infrared spectroscopy. Liver Transpl Surg 1999; 5: 219–226.
Meier SD, Eble BK, Stapleton GE, Morales DL, Chang AC, Andropoulos DB . Mesenteric oxyhemoglobin desaturation improves with patent ductus arteriosus ligation. J Perinatol 2006; 26: 562–564.
Stapleton GE, Eble BK, Dickerson HA, Andropoulos DB, Chang AC . Mesenteric oxygen desaturation in an infant with congenital heart disease and necrotizing enterocolitis. Tex Heart Inst J 2007; 34: 442–444.
Climan RI . Mechanisms regulating the ductus arteriosus. Biol Neonate 2006; 89: 330–335.
Acknowledgements
We would like to express our most sincere appreciation for the infants and their families for participation and commitment to this research project. This study was funded in part by a grant from Ovation Pharmaceuticals.
Contributor's Statement Page
Each of the three co-authors has made substantive intellectual contribution to the study (conception and design, acquisition of data, or analysis and interpretation of data, drafting of the manuscript or revising it critically for important intellectual content) and takes public responsibility for appropriate portions of the content of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Petrova, A., Bhatt, M. & Mehta, R. Regional tissue oxygenation in preterm born infants in association with echocardiographically significant patent ductus arteriosus. J Perinatol 31, 460–464 (2011). https://doi.org/10.1038/jp.2010.200
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.200
Keywords
This article is cited by
-
Nutrition of the preterm infant with persistent ductus arteriosus: existing evidence and practical implications
Pediatric Research (2023)
-
End-organ saturations correlate with aortic blood flow estimates by echocardiography in the extremely premature newborn – an observational cohort study
BMC Pediatrics (2021)
-
Brain and renal oxygenation measured by NIRS related to patent ductus arteriosus in preterm infants: a prospective observational study
BMC Pediatrics (2021)
-
The effect of patent ductus arteriosus on coronary artery blood flow in premature infants: a prospective observational pilot study
Journal of Perinatology (2020)
-
Regional tissue oxygenation monitoring in the neonatal intensive care unit: evidence for clinical strategies and future directions
Pediatric Research (2019)