Abstract
Objective:
To reassess iron supplementation practice safety in very low birth weight (VLBW) preterm infants receiving restrictive red blood cell transfusions during initial hospitalization.
Study Design:
Iron status, including hemoglobin (Hb), serum iron, ferritin, and soluble transferrin receptor (sTfR) levels and reticulocyte count of transfused (n=236) and non-transfused (n=166) preterm infants at ⩽24 h and 2, 4 and 8 weeks were recorded. As per protocol, a restrictive blood transfusion policy and supplementation of 5 mg kg–1 per day of iron polymaltose complex from 4 weeks and 25 mg–1 per day of vitamin E from 2 weeks were imposed for all infants. Normative reference cord-blood ferritin value of preterm infants was used for comparison. Vitamin E levels and incidence of morbidities associated with prematurity were recorded.
Result:
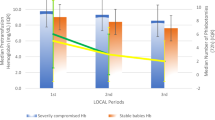
At ⩽24 h, the characteristics and iron status of both groups were similar. At 2, 4 and 8 weeks, the transfused group had significantly higher Hb, iron and ferritin levels; sTfR levels were lower at 4 and 8 weeks (all indices, P<0.05). At 8 weeks, the median ferritin levels of our transfused group were lower than that of normative reference cord-blood value (115 (50th percentile) vs 79 (43 to 107) μg l–1, respectively). Vitamin E levels and the incidence of morbidities associated with prematurity of the transfused and non-transfused groups were not different (both indices, P>0.18).
Conclusion:
Adding iron supplementation to preterm infants receiving restrictive blood transfusions has shown to be a judicious and safe practice in terms of iron status for VLBW preterm infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Rao R, Georgieff MK . Iron therapy for preterm infants. Clin Perinatol 2009; 36: 27–42.
Bifano EM, Curran TR . Minimizing donor blood exposure in the neonatal intensive care unit: current trends and future prospects. Clin Perinatol 1995; 22: 657–669.
Shafir T, Angulo-Barroso R, Jing Y, Angelilli ML, Jacobson SW, Lozoff B . Iron deficiency and infant motor development. Early Hum Dev 2008; 84: 479–485.
Grantham-McGregor S, Ani C . A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr 2001; 131: S649–S668.
Fleming RE . Cord serum ferritin levels, fetal iron status, and neurodevelopmental outcomes: correlations and confounding variables. J Pediatr 2002; 140: 145–148.
Armony-Sivan R, Eidelman AI, Lanir A, Sredni D, Yehuda S . Iron status and neurobehavioral development of premature infants. J Perinatol 2004; 24: 757–762.
Steinmacher J, Pohlandt F, Bode H, Sander S, Kron M, Franz AR . Randomized trial of early versus late enteral iron supplementation in infants with a birth weight of less than 1301 grams: neurocognitive development at 5.3 years’ corrected age. Pediatrics 2007; 120: 538–546.
Franz AR, Mihatsch WA, Sander S, Kron M, Pohlandt F . Prospective randomized trial of early versus late enteral iron supplementation in infants with a birth weight of less than 1301 grams. Pediatrics 2000; 106: 700–706.
Arnon S, Shiff Y, Litmanovitz I, Regev RH, Bauer S, Shainkin-Kestenbaum R et al. The efficacy and safety of early supplementation of iron polymaltose complex in preterm infants. Am J Perinatol 2007; 24: 95–100.
Arnon S, Regev RH, Bauer S, Shainkin-Kestenbaum R, Shiff Y, Bental Y et al. Vitamin E levels during early iron supplementation in preterm infants. Am J Perinatol 2009; 26: 387–392.
Ng PC, Lam CW, Lee CH, To KF, Fok TF, Chan IH et al. Hepatic iron storage in very low birth weight infants after multiple blood transfusions. Arch Dis Child Fetal Neonatal Ed 2001; 84: F101–F105.
Hesse L, Eberl W, Schlaud M, Poets CF . Blood transfusion: iron load and retinopathy of prematurity. Eur J Pediatr 1997; 156: 465–470.
Inder TE, Clemett RS, Austin NC, Graham P, Darlow BA . High iron status in very low birth weight infants is associated with an increased risk of retinopathy of prematurity. J Pediatr 1997; 131: 541–544.
Cooke RW, Drury JA, Yoxall CW, James C . Blood transfusion and chronic lung disease in preterm infants. Eur J Pediatr 1997; 156: 47–50.
Kaur D, Peng J, Chita SJ, Rajagopalan S, Di Monte DA, Cherny RA et al. Increased murine neonatal iron intake results in Parkinson-like neurodegeneration with age. Neurobiol Aging 2007; 28: 907–913.
Kirpalani H, Whyte R, Andersen C, Asztalos EV, Heddle N, Blajchman MA et al. The premature infants in need of transfusion (PINT) study: a randomized, controlled trial of a restrictive (low) versus liberal (high) transfusion threshold for extremely low birth weight infants. J Pediatr 2006; 149: 301–307.
Murray NA, Roberts IA . Neonatal transfusion practice. Arch Dis Child Fetal Neonatal Ed 2004; 89: F101–F107.
Siddappa AM, Rao R, Long JD, Widness JA, Georgieff MK . The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations. Neonatology 2007; 92: 73–82.
Sweet DG, Savage GA, Tubman R, Lappin TR, Halliday HL . Cord blood transferrin receptors to assess fetal iron status. Arch Dis Child Fetal Neonatal Ed 2001; 85: F46–F48.
Bard H, Widness JA . The life span of erythrocytes transfused to preterm infants. Pediatr Res 1997; 42: 9–11.
Hirano K, Morinobu T, Kim H, Hiroi M, Ban R, Ogawa S et al. Blood transfusion increases radical promoting non-transferrin bound iron in preterm infants. Arch Dis Child Fetal Neonatal Ed 2001; 84: F188–F193.
Brooks SE, Marcus DM, Gillis D, Pirie E, Johnson MH, Bhatia J . The effect of blood transfusion protocol on retinopathy of prematurity: a prospective, randomized study. Pediatrics 1999; 104 (3 Part 1): 514–518.
Braekke K, Bechensteen AG, Halvorsen BL, Blomhoff R, Haaland K, Staff AC . Oxidative stress markers and antioxidant status following oral iron supplementation to very low birth weight infants. J Pediatr 2007; 151: 23–28.
American Academy of Pediatrics. Committee on nutrition: nutritional needs of the preterm infant (1998). In: Kleinman RE (ed). Pediatric Nutrition Handbook. 5th edn. American Academy of Pediatrics: Chapel Hill, NC, 2004. pp 23–54.
Miller SM, McPherson RJ, Juul SE . Iron sulfate supplementation decreases zinc protoporphyrin to heme ratio in premature infants. J Pediatr 2006; 148: 44–48.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Arnon, S., Dolfin, T., Bauer, S. et al. Iron supplementation for preterm infants receiving restrictive red blood cell transfusions: reassessment of practice safety. J Perinatol 30, 736–740 (2010). https://doi.org/10.1038/jp.2010.33
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.33