Abstract
Introduction:
Birth of very low birth weight (VLBW) infants outside subspecialty perinatal centers increases risk for death and major morbidities.
Objective:
The purpose of this study is to evaluate barriers to utilizing a regional perinatal center for the birth of VLBW infants to mothers not living in the immediate vicinity of the center.
Methods:
We conducted a retrospective cohort study of VLBW infants residing in the catchment area of a community level II, Specialty Neonatal Unit (SN) admitted to a Regional Subspecialty Neonatal Intensive Care Unit (RC) between January 1999 and December 31, 2004. Maternal demographics and prenatal care as well as outcomes were compared by place of birth.
Results:
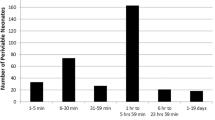
Out of 98 VLBW infants admitted to the RC, 49 (50%) were delivered outside the RC (out-born) and 49 (50%) were born at the RC (in-born). There was no statistical difference in insurance coverage, race, gestational age, severity of illness or maternal demographic factors between out-born and in-born infants. Less than adequate prenatal care rather than distance of maternal residence from the RC was associated with birth outside the RC. Adjusting for prenatal care, distance of residence from the RC increased the risk for delivering outside the center in the subset of mothers insured by Medicaid.
Conclusions:
Mothers of VLBW infants who received less than adequate prenatal care and did not live in the vicinity of a subspecialty center had an increased risk for delivery outside that center compared to those with adequate care. Appropriate place of birth for VLBW infants to low-income mothers may be influenced by the distance of their residence to an RC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American Academy of Pediatrics and the American College of Obstetrics and Gynecology. Guidelines for Perinatal Care, 5th edn. American Academy of Pediatrics: Elk Grove Village, IL; American College of Obstetrics and Gynecology: Washington, DC, 2002.
Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M et al. Trends in mortality and morbidity for very low birth weight infants, 1991–1999. Pediatrics 2002; 110: 143–151.
Bode MM, O’Shea TM, Metzguer KR, Stiles AD . Perinatal regionalization and neonatal mortality in North Carolina, 1968–1994. Am J Obstet Gynecol 2001; 184: 1302–1307.
Cifuentes J, Bronstein J, Phibbs CS, Phibbs RH, Schmitt SK, Carlo WA . Mortality in low birth weight infants according to level of neonatal care at hospital of birth. Pediatrics 2002; 109: 745–751.
Sanderson M, Sappenfield WM, Jespersen KM, Liu Q, Baker SL . Association between level of delivery hospital and neonatal outcomes among South Carolina Medicaid recipients. Am J Obstet Gynecol 2000; 183: 1504–1511.
Chien LY, Whyte R, Aziz K, Thiessen P, Matthew D, Lee SK . Improved outcome of preterm infants when delivered in tertiary care centers. Obstet Gynecol 2001; 98: 247–252.
Warner B, Musial MJ, Chenier T, Donovan E . The effect of birth hospital type on the outcome of very low birth weight infants. Pediatrics 2004; 113: 35–41.
Menard MK, Liu Q, Holgren EA, Sappenfield WM . Neonatal mortality for very low birth weight deliveries in South Carolina by level of hospital perinatal service. Am J Obstet Gynecol 1998; 179: 374–381.
Hogue CJ, Vasquez C . Toward a strategic approach for reducing disparities in infant mortality. Am J Public Health 2002; 92: 552–556.
Palmer KG, Kronsberg SS, Barton BA, Hobbs CA, Hall RW, Anand KJ . Effect of inborn versus outborn delivery on clinical outcomes in ventilated preterm neonates: secondary results from the NEOPAIN trial. J Perinatol 2005; 25: 270–275.
Healthy People 2010. US Department of Health and Human Services: Washington, DC, 2000, http://www.healthypeople.gov/document/.
D’Ascoli PT, Alexander GR, Petersen DJ, Kogan MD . Parental factors influencing patterns of prenatal care utilization. J Perinatol 1997; 17: 283–287.
Sinkin RA, Fisher SG, Dozier A, Dye TD . Effect of managed care on perinatal transports for the publicly funded in upstate New York. J Perinatol 2005; 25: 79–85.
Adams EK, Gavin NI, Benedict MB . Access for pregnant women on Medicaid: variation by race and ethnicity. J Health Care Poor Underserved 2005; 16: 74–95.
Samuelson JL, Buehler JW, Norris D, Sadek R . Maternal characteristics associated with place of delivery and neonatal mortality rates among very-low-birthweight infants, Georgia. Paediatr Perinat Epidemiol 2002; 16: 305–313.
Bronstein JM, Capilouto E, Carlo WA, Haywood JL, Goldenberg RL . Access to neonatal intensive care for low-birthweight infants: the role of maternal characteristics. Am J Public Health 1995; 85: 357–361.
Gould JB, Sarnoff R, Liu H, Bell DR, Chavez G . Very low birth weight births at non-NICU hospitals: the role of sociodemographic, perinatal, and geographic factors. J Perinatol 1999; 19: 197–205.
Carmona R . Access to Quality Health Services. Progress Review. US Department of Health & Human Services, 2002, http://www.healthypeople.gov/data/2010prog/focus01/.
Attar MA, Lang SW, Gates MR, Iatrow AM, Bratton SL . Back transport of neonates: effect on hospital length of stay. J Perinatol 2005; 25: 731–736.
Richardson DK, Corcoran JD, Escobar GJ, Lee SK . SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores. J Pediatr 2001; 138: 92–100.
Kessner DM, Kalk CE, Singer J . Assessing health quality — the case for tracers. N Engl J Med 1973; 288: 189–194.
Hosmer DW, Lemeshow S . Applied Logistic Regression. John Wiley & Sons Inc.: New York, 1989.
Howell EM, Vert P . Neonatal intensive care and birth weight-specific perinatal mortality in Michigan and Lorraine. Pediatrics 1993; 91: 464–469.
Dubay L, Joyce T, Kaestner R, Kenney GM . Changes in prenatal care timing and low birth weight by race and socioeconomic status: implications for the Medicaid expansions for pregnant women. Health Serv Res 2001; 36: 373–398.
Kogan MD, Martin JA, Alexander GR, Kotelchuck M, Ventura SJ, Frigoletto FD . The changing pattern of prenatal care utilization in the United States, 1981–1995, using different prenatal care indices. JAMA 1998; 279: 1623–1628.
Misra DP, Guyer B . Benefits and limitations of prenatal care: from counting visits to measuring content. JAMA 1998; 279: 1661–1662.
DiGiuseppe DL, Aron DC, Ranbom L, Harper DL, Rosenthal GE . Reliability of birth certificate data: a multi-hospital comparison to medical records information. Matern Child Health J 2002; 6: 169–179.
Acknowledgements
This work was financially supported by a grant from Michigan Department of Community Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Attar, M., Hanrahan, K., Lang, S. et al. Pregnant mothers out of the perinatal regionalization's reach. J Perinatol 26, 210–214 (2006). https://doi.org/10.1038/sj.jp.7211488
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211488
Keywords
This article is cited by
-
Rural-urban differences in access to hospital obstetric and neonatal care: how far is the closest one?
Journal of Perinatology (2018)
-
Travel Time to Hospital for Childbirth: Comparing Calculated Versus Reported Travel Times in France
Maternal and Child Health Journal (2018)
-
Pregnancy and Birth Outcome Improvements for American Indians in the Healthy Start Project of the Inter-Tribal Council of Michigan, 1998–2008
Maternal and Child Health Journal (2013)
-
Prenatal Care Utilization in Mississippi: Racial Disparities and Implications for Unfavorable Birth Outcomes
Maternal and Child Health Journal (2011)