Abstract
Angiotensin II receptor blockers (ARBs) represent a new class of effective and well tolerated orally active antihypertensive agents. Recent clinical trials have shown the added benefits of ARBs in hypertensive patients (reduction in left ventricular hypertrophy, improvement in diastolic function, decrease in ventricular arrhythmias, reduction in microalbuminuria, and improvement in renal function), and cardioprotective effect in patients with heart failure. Several large long-term studies are in progress to assess the beneficial effects of ARBs on cardiac hypertrophy, renal function, and cardiovascular and cerebrovascular morbidity and mortality in hypertensive patients with or without diabetes mellitus, and the value of these drugs in patients with heart disease and diabetic nephropathy.
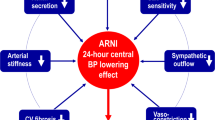
The ARBs specifically block the interaction of angiotensin II at the AT1 receptor, thereby relaxing smooth muscle, increasing salt and water excretion, reducing plasma volume, and decreasing cellular hypertrophy. These agents exert their blood pressure-lowering effect mainly by reducing peripheral vascular resistance usually without a rise in heart rate. Most of the commercially available ARBs control blood pressure for 24 h after once daily dosing. Sustained efficacy of blood pressure control, without any evidence of tachyphylaxis, has been demonstrated after long-term administration (3 years) of some of the ARBs. The efficacy of ARBs is similar to that of thiazide diuretics, beta-blockers, angiotensin-converting enzyme inhibitors or calcium channel blockers in patients with similar degree of hypertension. Higher daily doses, dietary salt restriction, and concomitant diuretic or ACE inhibitor administration amplify the antihypertensive effect of ARBs. The ARBs have a low incidence of adverse effects (headache, upper respiratory infection, back pain, muscle cramps, fatigue and dizziness), even in the elderly patients. After the approval of losartan, five other ARBs (candesartan cilexetil, eprosartan, irbesartan, telmisartan, and valsartan) and three combinations with hydrochlorothiazide (irbesartan, losartan and valsartan) have been approved as antihypertensive agents, and some 28 compounds are in various stages of development.
The ARBs are non-peptide compounds with varied structures; some (candesartan, losartan, irbesartan, and valsartan) have a common tetrazolo-biphenyl structure. Except for irbesartan, all active ARBs have a carboxylic acid group. Candesartan cilexetil is a prodrug, while losartan has a metabolite (EXP3174) which is more active than the parent drug. No other metabolites of ARBs contribute significantly to the antihypertensive effect.
The variation in the molecular structure of the ARBs results in differences in the binding affinity to the receptor and pharmacokinetic profiles. The differences observed in lipid solubility, absorption/distribution, plasma protein binding, bioavailability, biotransformation, plasma half-life, and systemic elimination influence the time of onset, duration of action, and efficacy of the ARBs. On the basis of the daily mg dose, the antihypertensive potency of the ARBs follows the sequence: candesartan cilexetil > telmisartan losartan > irbesartan valsartan > eprosartan.
After oral administration, the ARBs are rapidly absorbed (time for peak plasma levels = 0.5–4 h) but they have a wide range of bioavailability (from a low of 13% for eprosartan to a high of 60–80% for irbesartan); food does not influence the bioavailability, except for valsartan (a reduction of 40–50%) and eprosartan (increase). A limited dose-peak plasma levels/areas under the plasma level-time curve proportionality is observed for some of the ARBs. Most of these drugs have high plasma protein binding (95–100%); irbesartan has the lowest binding among the group (90%). The steady-state volumes of distribution vary from a low of 9 L (candesartan) to a high of 500 L (telmisartan). Plasma elimination half-life is short for candesartan cilexetil and losartan (1–4 h), intermediate for eprosartan and valsartan (5–10 h), and longer for candesartan, irbesartan and telmisartan (11–38 h); the active metabolite of losartan has a longer half-life than for the parent drug. The drugs and their active metabolites do not accumulate to a significant extent after repeated dosing, except for telmisartan (100%). Most of the orally administered dose of ARBs is excreted via bile into the faeces; from 2% (telmisartan) to 33% (candesartan) of the oral dose is excreted in the urine. In most cases, changes in pharmacokinetic parameters due to aging, mild to moderate renal disease and heart failure do not require dosage modification; dosage has to be individualised for eprosartan, losartan, telmisartan and valsartan in patients with hepatic disease. In general, pharmacokinetic drug–drug interactions are rare, with the exception of combination of digoxin and telmisartan.
The ARBs are an important treatment option for hypertension, being relatively safe and efficacious. The beneficial effects of the ARB therapy go beyond blood pressure control. They may prove to have beneficial haemodynamic and neurohormonal effects in heart failure and provide renoprotection in diabetic nephropathy. Journal of Human Hypertension
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Israili, Z. Clinical pharmacokinetics of angiotensin II (AT1) receptor blockers in hypertension. J Hum Hypertens 14 (Suppl 1), S73–S86 (2000). https://doi.org/10.1038/sj.jhh.1000991
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1000991
Keywords
This article is cited by
-
Implications of Sex Differences on the Treatment Effectiveness in Heart Failure with Reduced Ejection Fraction Related to Clinical Endpoints and Quality of Life
Current Heart Failure Reports (2024)
-
The Renin Angiotensin System as a Therapeutic Target in Traumatic Brain Injury
Neurotherapeutics (2023)
-
Current and Emerging Classes of Pharmacological Agents for the Management of Hypertension
American Journal of Cardiovascular Drugs (2022)
-
What have we learned so far from the sex/gender issue in heart failure? An overview of current evidence
Internal and Emergency Medicine (2022)
-
Pharmacodynamic model of slow reversible binding and its applications in pharmacokinetic/pharmacodynamic modeling: review and tutorial
Journal of Pharmacokinetics and Pharmacodynamics (2022)