Abstract
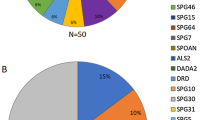
The SPAST gene has a major role in hereditary spastic paraplegias (HSPs). This is the first report mapping characteristics of the SPAST gene in a large cohort of Czech HSP patients. All 17 coding exons of the SPAST gene were Sanger sequenced in 327 patients from 263 independent families with suspected uncomplicated HSP. The selected 126 independent patients, without mutation in the SPAST gene after Sanger sequencing, were subsequently tested by Multiplex Ligation-dependent Probe Amplification (MLPA) assay for large deletions or copy number variations affecting the SPAST gene. Among the 263 independent patients, 35 different, small mutations in 44 patients were found. Twenty-one mutations are novel with the majority of frameshift mutations. Seven mutations were found in more than one family. The age at onset ranged between preschool childhood and the fifth decade with inter- and intra-familiar differences. SPAST small mutations were detected in 16.7% (44/263) of independent tested patients. Mutations in the SPAST gene were found more frequently in familial cases (with affected relatives). Mutation were found in 31.9% (29/91 familial tested) in the familial patient group, whereas in the sporadic patient group, mutations were found in only 4.7% of cases (5/106 sporadic cases). Among SPAST-positive patients, 65.9% (29/44) were familial but only 11.4% (5/44) were sporadic. MLPA testing revealed four large deletions in four independent patients, all in familial-positive cases. Mutations in the SPAST gene are 5.8 × more frequent in familial than in sporadic cases. Large deletions were found only in familial patients. Diagnostic testing of the SPAST gene is useful only in positive family history patients not in sporadic cases.
Similar content being viewed by others
Introduction
Hereditary spastic paraplegias (HSPs), also known as the Strümpell–Lorrain disease, are a group of clinically and genetically heterogeneous inherited neurodegenerative disorders. The obligatory clinical feature of the disease is progressive bilateral spasticity and weakness of the lower limbs. Histopathological studies have revealed selective degeneration of some of the longest axons of the pyramidal tract.
According to its clinical presentation, HSP patients are categorized as having uncomplicated form with isolated progressive spasticity and weakness of lower limbs or complicated form with other neurological signs such as ataxia, mental and cognitive changes, extrapyramidal disturbances, visual or auditory dysfunction and/or peripheral neuropathy. Uncomplicated HSP is the most common form comprising about 90% of all patients with HSP.1
HSP may follow all known types of Mendelian inheritance, including the autosomal-dominant form, which is observed most frequently (70–80%), as well as the autosomal-recessive and X-linked forms.2 To date, >50 causal genes have been identified for HSPs.2, 3
Mutations in the SPAST gene are by far the most frequent cause of HSP. The SPAST gene (previously referred as SPG4) is located on chromosome 2p24-p21, has 17 coding exons and encodes 616 amino-acid protein, which is a member of the AAA ATPase protein family and has an important role in the axonal transport as it regulates microtubule organization.4, 5 SPAST mutations were found in about 40% of uncomplicated autosomal-dominant HSP cases and 10% of sporadic cases in different populations.6, 7, 8, 9 More than 500 mutations have been identified in the SPAST gene (http://www.hgmd.cf.ac.uk) to date.
Cases of HSP that are caused by SPAST mutations usually present as uncomplicated form of the disease, which is often associated with a decreased perception of vibration in the lower limbs and urinary problems. However, the age at onset, severity of symptoms and progression of symptoms are highly variable, even within the same family.8, 9, 10
The prevalence and types of SPAST mutations among Czech patients with HSP are currently unknown. In this study, we aimed to determine the frequency of SPAST mutations in Czech subjects with the pure form of HSP and compare the frequencies among familial and sporadic cases. We present herein the genetic and clinical findings related to the SPAST gene mutations in a large cohort of Czech patients suspected of having pure HSP.
Material and methods
Patients
The SPAST gene was examined in 263 independent Czech patients with pure form of probable HSP—spastic paraplegia without any known cause. The final number of Sanger-sequenced patients was 327 (independent patients plus their affected/unaffected relatives). The Gennet Centre for Medical Genetics and Reproductive Medicine is the only DNA laboratory in the Czech Republic offering DNA testing for HSP. The 263 independent patient cohort consisted of 106 sporadic patients (40.3%) and 91 familial cases (34.6%) with affected relatives in a minimum of two successive generations. Because we followed an autosomal-dominant inheritance pattern for the SPAST gene, patients with apparently autosomal-recessive inheritance were not included. In the remaining 66 patients (25.1%), the family history could not be defined. Multiplex Ligation-dependent Probe Amplification (MLPA) assay targeting the SPAST gene was performed in 126 selected, unrelated patients, previously tested negative by Sanger sequencing: 66 of them were familial cases (52.4%), 41 sporadic (32.5%), and in 19 of them the family status was undefined (15.1%).
Patients were clinically diagnosed by different neurologists or geneticists. All patients in our cohort presented signs of pure/uncomplicated HSP according to the Harding criteria.1 Mild associated symptoms, such as sensory disturbance or bladder dysfunction, were allowed. Patients with complicated form of HSP (known associated with cognitive impairment, epilepsy, dystonia, optic atrophy, ataxia and so on) were not included/tested for SPAST mutations. Informed consent with DNA testing was obtained from all individual participants included in the study.
Mutation analysis
Genomic DNA was extracted from peripheral blood according to standard protocol and used to amplify all 17 coding exons and exon/intron boundaries of the SPAST gene. Primers were designed with the ExonPrimer Software (Helmholtz Center, Munich, Germany) according to NM_014946.3 (sequences available upon request). PCR products were purified (FastAP/ExoI, Thermo Scientific, Waltham, MA, USA). Sanger sequencing was performed with the BigDye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, Foster City, CA, USA). Primary MLPA testing was performed by the P-165 Kit (MRC Holland, Amsterdam, The Netherlands). The P-211 MLPA Kit (MRC Holland), which targets the SPAST termini as well as the neighboring genes DPY30 and SLC30A6, was applied to samples found positive for a large deletion. Products of Sanger sequencing and of MLPA were analyzed on a Genetic Analyzer ABI 3130 (Applied Biosystems). Coffalyzer software was used for evaluation of the MLPA chromatograms (MRC Holland). HGVS nomenclature and reference sequence NM_014946.3 were used for assigning the mutations. Novel mutations were analyzed in silico using the Alamut Software (Interactive Biosoftware, Rouen, France) with prediction programs incorporated (Polyphen 2, Mutation Taster and SIFT). Pathogenicity of all mutations not described previously was assessed only in silico (in case of missense mutations) by prediction programs Polyphen 2 (http://genetics.bwh.harvard.edu/pph2/), Mutation Taster (www.mutationtaster.org) and SIFT (http://sift.jcvi.org/). We also performed segregation analysis in all families where it was possible (additional family members were available for testing). We used frequency data from databases Exome Variant Server (EVS) (http://evs.gs.washington.edu), ExAC (http://exac.broadinstitute.org/), dbSNP (http://www.ncbi.nlm.nih.gov/SNP/) and 1000 Genomes (http://www.1000genomes.org) for comparison as the control group.
Results
Findings regarding mutation frequencies
Sanger sequencing. Fraction of small mutation-positive patients (per group defined by inheritance)
Our testing of 263 independent patients yielded 44 SPAST mutation-positive cases (44/263 (tot-Seq); 16.7%). Among these, 29 were familial (29/91 (fam-Seq); 31.9%), only 5 sporadic (5/106 (as-Seq); 4.7%) and 10 with no family data 10/66 (nd-Seq); 15.2%).
MLPA testing
We performed MLPA testing of the SPAST gene in the selected 126 patients previously tested negative by sequencing of the SPAST gene for detection of large deletions or copy number variations. These were 66 of familial origin (fam-MLPA), 41 apparently sporadic (as-MLPA) and 19 with no family data (nd-MLPA). First, we performed MLPA testing in all patients, either familial or sporadic. We detected only two patients with large deletion affecting the SPAST gene after 93 patients tested and both were familial. We further followed MLPA testing only in familial patients. We performed MLPA assay in a further 33 patients with positive family history and found two more large deletions in the SPAST gene. Subsequent testing of these four deletion-positive samples by an extended MLPA Kit (P211) revealed that neighboring genes are co-deleted in all but one case (Table 1).
Fraction of large deletion-positive patients (per group defined by inheritance)
We revealed four large deletions (4/126 (tot-MLPA); 3.2%). All four deletions were found in familial cases (4/66 (fam-MLPA); 6.1%). No large deletion was found in neither sporadic nor unknown family status patients (0/41 (as-MLPA); 0%, 0/19 (nd-MLPA), 0%).
Fraction of all kinds of mutations
We tried to estimate the contribution of small mutations vs large deletions separately in the group of sporadic and familial patients, in the group with no family data and in the total cohort of our patients. This fraction can only be estimated from the data above, as the groups screened were not identical (263 sequenced and 126 MLPA tested; Table 2).
In the group of familial patients, small mutations represent 84% of all mutations found; 16% are large deletions. In the groups of sporadic patients and in the group of patients with no family data history, 100% of mutations were small mutations. No large deletion was found in these groups. The total fraction of all mutations is 84% small mutations and 16% large deletions.
Findings regarding features of small mutation
We identified 35 different heterozygous mutations with possibly pathogenic effect in the SPAST gene in 44 unrelated patients by Sanger sequencing (Table 3).
Novelty
Among 35 mutations found in our cohort, 21 mutations were novel (12 frameshift, 4 missense, 4 splice site, 1 nonsense) and not listed in the HGMD Professional database (http://www.hgmd.cf.ac.uk) and 14 mutations were described previously (8 missense, 1 frameshift, 2 nonsense, 3 splice site).
Recurrent vs private
Seven mutations (4 novel, 3 described) were found in more than one family. Two of these mutations, c.80_98dup (novel) and c.1291C>T (described previously), were detected even in three patients from three unrelated families. Novel mutation c.110_123del was found in two unrelated families (numbers 5 and 6). We assume that these two families could be related, as they live in the same region.
Type of mutations
Overall, we found 13 frameshift, 12 missense, 3 nonsense and 7 splice site mutations. Detected SPAST small mutations are scattered in 13 of the 17 coding exons of the gene excluding exons 4, 7, 12 and 16.
Others
The age at onset of the SPAST mutation-positive patients (small mutations plus large deletions) ranged between 4 and 60 years. There was no correlation between age at onset and type of mutation. There were inter-familiar and even intra-familiar differences in age at onset for the same mutation (families 15 and 21, Table 3).
Polymorphisms
p.S44L
The variant c.131C>T previously described as a potential modifier,11, 12 was found in 7 cases among 263 examined independent patients (allele frequency 7/526; 1.3%). This finding is consistent with the figure of 0.9% of allele frequency among European Americans (EA) in the EVS. In one case, this variant was found in a patient with detected mutation in exon 6 (patient number 15). The age at onset in this patient was in childhood in comparison with the affected mother, who carries the same mutation c.973dup but not the variant c. 131C>T and the age at onset was in the early fifties.
p.P45Q
In one case, we detected the variant c.134C>A, which is described as a potential modifier too by Svenson et al.12 We did not find other pathogenic mutations in the SPAST gene in this patient. The patient’s afflictions could not be explained solely by this finding.
p.P293P
We found the silent variant c.879C>A (p.P293P) in seven cases (allele frequency 7/526; 1.3%). All were negative for SPAST pathogenic mutations. This is consistent with the figure of 1.5% of allele frequency among EA in EVS as well.
Intronic polymorphisms
We further detected three known polymorphisms in adjacent intron sequences. The variant (polymorphism) c.1322-38del was found in six cases (allele frequency 6/526; 1.1%) and c.1322-24G>C in two cases (allele frequency 2/526; 0.4%). These patients were SPAST mutation negative. Both these findings are consistent with the figures of 0.6% and 0.1%, respectively, of allele frequency among EA in EVS.
Discussion
We provide evaluation of long-time diagnostic DNA testing of the SPAST gene among a large cohort of Czech patients suspected of having an uncomplicated HSP.
We detected 21 novel point mutations. All these mutations seem to be pathogenic and causal. All novel/undescribed mutations have zero frequency in the EVS, ExAC, dbSNP and 1000 Genomes databases that were used as the control group next to other individuals of Czech origin sequenced for diagnostic purposes. A special group of control samples from only healthy subjects was not used as we find it redundant in view of the large number of tested persons in our center and mainly in the much larger control databases mentioned above. We found four novel missense and one novel nonsense mutations that we assume to be pathogenic. All these mutations were assessed as deleterious or disease causing with prediction programs. We conducted segregation in only one mutation c.1303C>A (patient number 29, Table 3). Both healthy parents were tested; no mutations were found. In another three novel missense mutations c.29A>G, c.1610T>C and c.1838A>G and in novel nonsense mutation c.928A>T, segregation analysis in the family could not be performed. We found a further 12 novel frameshift mutations. Eight of them we assume to be pathogenic and causal also because of a positive segregation analysis in the families. The mutation segregates with the uncomplicated HSP phenotype in patient (family) numbers 2, 3, 5, 6, 7, 13, 14, 15, 16, 19 and 42 (Table 3). In the remaining four novel frameshift mutations, segregation analysis could not be performed. The frameshift mutations in the SPAST gene predict a loss of function and were previously described as pathogenic.4, 7, 8, 9 Sauter et al.9 described a high number of frameshift mutations (14 from 27 described) in their cohort of patients.
We detected four novel mutations that affect splicing (three donor splice site, one acceptor splice site). As the mutations c.1173+2dup, c.1687+2_1687+6del and c.1688-1G>C segregate with the uncomplicated HSP phenotype in the families (family numbers 20, 38 and 40, Table 3), we assume them to be pathogenic beside the type of mutation according to segregation with the disease in the family. In family number 20 (Table 3; mutation c.1173+2dup), three healthy relatives were tested, all without mutation. In family number 38 (Table 3; mutation c.1687+2_1687+6del), eight relatives were tested: three affected with the same mutation and five healthy without mutation. In family number 40 (Table 3; mutation c.1688-1G>C), two affected relatives were tested, both with the same mutation. Novel donor splice site mutation c.1004+1G>C was found in one patient (family number 17) with no family data, but we assume this mutation to be pathogenic too as it affects the invariable nucleotide +1. We did not perform functional studies on the RNA level or exon skipping testing, so pathogenicity of this mutation could only be estimated theoretically. We assume that these intronic mutations, affecting the invariant nucleotides ±1 or 2 can alter the final protein product by exon skipping. The splice site mutation c.1245+1G>A was previously referred to by Svenson et al.13; they proved exon skipping for this mutation by RNA analysis.
In total, we have found 12 missense and 13 frameshift mutations among 35 detected SPAST point mutations, which represents 34.3% and 37.1% of all mutations detected by Sanger sequencing in the group of Czech patients. Missense and frameshift mutations account for the majority of SPAST mutation-positive Czech patients. These findings correspond with Sauter et al.9 They described frameshift mutations as the most frequent mutation type in the SPAST gene in German HSP patients.9
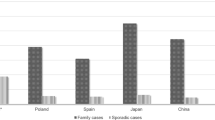
In the group of SPAST-positive patients with small mutations, those with positive family history were in the majority: 65.9% (29/44), compared with sporadic cases: 11.4% (5/44). For the remaining families with mutations, we have no family history details. Our findings with the high number of familial cases are comparable with other European and Asian studies. Dutch and Romanian studies revealed 72% and 70% of familial cases in patients with SPAST mutations.6, 14 Korean and Japanese studies describe 66.7% and 67.3%, respectively, of familial cases among autosomal-dominant HSP patients.15, 16
Five cases from 44 SPAST-positive (11.4%) seemed sporadic, but only in 2 cases (patient numbers 29 and 33, Table 3) we do have enough data about the family because we could test both parents for the presence of the mutation. The mutation, however, was not present, suggesting a de novo mutation origin in the patient. Another three apparently sporadic patients by family history (number 9, 28 and 43, Table 3) have incomplete clinical assessment and provided poor family information. Based only on verbal information, the patients were diagnosed as sporadic with negative family history, but DNA testing and clinical examination would be necessary for confirmation.
We detected four large deletions (all in familial patients) in the SPAST gene among the 126 MLPA-tested patients. The major risk of MLPA testing is the potential primer mismatch of MLPA probes leading to false positive results. False negativity is not an issue. In three of the four SPAST-large-deletion-positive patients in our cohort, all or most exons or several exons were affected. In one patient (number 4, Table 1), only exon 17 was deleted, but this exon is covered with two probes in MLPA P-165 Kit and both showed decreased intensity as in a deletion. The potential problem with allele drop-out could be excluded. The probability that two probes are primer mismatched is minimal. A second problem was the lack of positive controls available for testing. In patient number 4 (Table 1), we tested the affected father of our patient with the same result. In patient number 3 (Table 1), we performed two tests in two independent laboratories with the same result. Moreover, an extended MLPA assay confirmed the primary findings and revealed that three of the four deletions extend even into the neighboring genes. Finally, MLPA testing is generally considered a reliable and reproducible method, frequently used for clinical diagnostics, and we have found the results of our testing to be consistent, although we are aware of potential pitfalls.
Our findings represent only 3.2% large-deletion-positive cases of all the patients tested. Large deletions in the SPAST gene seem to be rarer than reported before.17, 18 Beetz et al.17 and Sulek et al.18 found large deletion/duplication in 18% and 14%, respectively, of examined patients. The majority of the positive patients had familial occurrence of HSP. Our findings support the usefulness of MLPA testing only in familial but not in sporadic cases.
We detected benign polymorphism c.131C>T (p.S44L) in one patient with frameshift mutation c.973dup in exon 6 (family number 15, Table 3). The age at onset in the patient was in childhood in comparison to her affected mother, who has the same causal pathogenic mutation c.973dup but does not have c.131C>T (p.S44L) polymorphism and age at onset was approximately at the age of 50 years. This variant c.131C>T (p.S44L) is not only known as a non-pathogenic variant in healthy subjects but was also reported as a phenotype-modifying variant in SPAST-positive patients with the first symptoms manifesting at a significantly earlier age.11, 12
In only a few cases among all examined patients, we detected non-pathogenic or benign variant in the coding region of the SPAST gene. Our findings are consistent with the allele frequencies for EA in The EVS. Similar findings were reported previously. Svenson et al.13 found polymorphism only in 1 patient among 15 families and no other polymorphisms. Sauter et al.9 found 3 different polymorphisms in coding exons of SPAST gene in 10 members from 161 families. Fonknechten et al.8 even failed to detect any polymorphisms in coding exons in 17 families. The sequence of the SPAST gene seems to be stable with a minimum of de novo mutations or variants. This assumption is supported with minimum number of sporadic de novo mutations or polymorphisms or benign variants found in our cohort. The majority of detected mutations is in patients with positive family history, which supports the suggestion that de novo mutations probably occur rarely in the SPAST gene.
We report the first genetic study of uncomplicated HSP patients from the Czech Republic. We found broad mutation spectrum in 13 from the 17 coding exons and adjacent regions of the SPAST gene. We detected 21 novel presumably pathogenic mutations. The high frequency of SPAST mutations was found only in familial patients. Mutations in the SPAST gene are 5.8 × more frequent in familial than in sporadic cases. Large deletions are rarer than originally reported from some other cohorts. Testing of the SPAST gene is much more useful in familial patients.
References
Harding, A. E. Classification of the hereditary ataxias and paraplegias. Lancet 1, 1151–1155 (1983).
Fink, J. K. Hereditary spastic paraplegia. Curr. Neurol. Neurosci. Rep. 6, 65–76 (2006).
Hensiek, A., Kirker, S. & Reid, E. Diagnosis, investigation and management of hereditary spastic paraplegias in the era of next-generation sequencing. J. Neurol. 262, 1601–1612 (2015).
Hazan, J., Fonknechten, N., Mavel, D., Paternotte, C., Samson, D., Artiguenave, F. et al. Spastin, a new AAA protein, is altered in the most frequent form of autosomal dominant spastic paraplegia. Nat. Genet. 23, 296–303 (1999).
Kasher, P. R., De Vos, K. J., Wharton, S. B., Manser, C., Bennett, E. J., Bingley, M. et al. Direct evidence for axonal transport defects in a novel mouse model of mutant spastin-induced hereditary spastic paraplegia (HSP) and human HSP patients. J. Neurochem. 110, 34–44 (2009).
de Bot, S. T., van den Elzen, R. T., Mensenkamp, A. R., Schelhaas, H. J., Willemsen, M. A., Knoers, N. V. et al. Hereditary spastic paraplegia due to SPAST mutations in 151 Dutch patients: new clinical aspects and 27 novel mutations. J. Neurol. Neurosurg. Psychiatry 81, 1073–1078 (2010).
Erichsen, A. K., Inderhaug, E., Mattingsdal, M., Eiklid, K. & Tallaksen, C. M. Seven novel mutations and four exon deletions in a collection of Norwegian patients with SPG4 hereditary spastic paraplegia. Eur. J. Neurol. 14, 809–814 (2007).
Fonknechten, N., Mavel, D., Byrne, P., Davoine, C. S., Cruaud, C., Bonsch, D. et al. Spectrum of SPG4 mutations in autosomal dominant spastic paraplegia. Hum. Mol. Genet. 9, 637–644 (2000).
Sauter, S., Miterski, B., Klimpe, S., Bonsch, D., Schols, L., Visbeck, A. et al. Mutation analysis of the spastin gene (SPG4) in patients in Germany with autosomal dominant hereditary spastic paraplegia. Hum. Mutat. 20, 127–132 (2002).
Proukakis, C., Moore, D., Labrum, R., Wood, N. W. & Houlden, H. Detection of novel mutations and review of published data suggests that hereditary spastic paraplegia caused by spastin (SPAST) mutations is found more often in males. J. Neurol. Sci. 306, 62–65 (2011).
Solowska, J. M., Garbern, J. Y. & Baas, P. W. Evaluation of loss of function as an explanation for SPG4-based hereditary spastic paraplegia. Hum. Mol. Genet. 19, 2767–2779 (2010).
Svenson, I. K., Kloos, M. T., Gaskell, P. C., Nance, M. A., Garbern, J. Y., Hisanaga, S. et al. Intragenic modifiers of hereditary spastic paraplegia due to spastin gene mutations. Neurogenetics 5, 157–164 (2004).
Svenson, I. K., Ashley-Koch, A. E., Gaskell, P. C., Riney, T. J., Cumming, W. J., Kingston, H. M. et al. Identification and expression analysis of spastin gene mutations in hereditary spastic paraplegia. Am. J. Hum. Genet. 68, 1077–1085 (2001).
Orlacchio, A., Patrono, C., Borreca, A., Babalini, C., Bernardi, G. & Kawarai, T. Spastic paraplegia in Romania: high prevalence of SPG4 mutations. J. Neurol. Neurosurg. Psychiatry 79, 606–607 (2008).
Kim, T. H., Lee, J. H., Park, Y. E., Shin, J. H., Nam, T. S., Kim, H. S. et al. Mutation analysis of SPAST, ATL1, and REEP1 in Korean patients with hereditary spastic paraplegia. J. Clin. Neurol. 10, 257–261 (2014).
Ishiura, H., Takahashi, Y., Hayashi, T., Saito, K., Furuya, H., Watanabe, M. et al. Molecular epidemiology and clinical spectrum of hereditary spastic paraplegia in the Japanese population based on comprehensive mutational analyses. J. Hum. Genet. 59, 163–172 (2014).
Beetz, C., Nygren, A. O., Schickel, J., Auer-Grumbach, M., Burk, K., Heide, G. et al. High frequency of partial SPAST deletions in autosomal dominant hereditary spastic paraplegia. Neurology 67, 1926–1930 (2006).
Sulek, A., Elert, E., Rajkiewicz, M., Zdzienicka, E., Stepniak, I., Krysa, W. et al. Screening for the hereditary spastic paraplaegias SPG4 and SPG3A with the multiplex ligation-dependent probe amplification technique in a large population of affected individuals. Neurol. Sci. 34, 239–242 (2013).
Magariello, A., Tortorella, C., Patitucci, A., Tortelli, R., Liguori, M., Mazzei, R. et al. First mutation in the nuclear localization signal sequence of spastin protein identified in a patient with hereditary spastic paraplegia. Eur. J. Neurol. 20, e22–e23 (2013).
Meijer, I. A., Hand, C. K., Cossette, P., Figlewicz, D. A. & Rouleau, G. A. Spectrum of SPG4 mutations in a large collection of North American families with hereditary spastic paraplegia. Arch. Neurol. 59, 281–286 (2002).
Falco, M., Scuderi, C., Musumeci, S., Sturnio, M., Neri, M., Bigoni, S. et al. Two novel mutations in the spastin gene (SPG4) found by DHPLC mutation analysis. Neuromuscul. Disord. 14, 750–753 (2004).
Park, S. Y., Ki, C. S., Kim, H. J., Kim, J. W., Sung, D. H., Kim, B. J. et al. Mutation analysis of SPG4 and SPG3A genes and its implication in molecular diagnosis of Korean patients with hereditary spastic paraplegia. Arch. Neurol. 62, 1118–1121 (2005).
Acknowledgements
We thank all the patients and their families for their participation in this study. Ethical standards of experiments comply with the current laws of the country of origin. This study was supported by Ministry of Health of the Czech Republic, grant numbers 15-33041A and DRO 00064203.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Mészárosová, A., Putzová, M., Čermáková, M. et al. SPAST mutation spectrum and familial occurrence among Czech patients with pure hereditary spastic paraplegia. J Hum Genet 61, 845–850 (2016). https://doi.org/10.1038/jhg.2016.73
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2016.73