Abstract
Genetic variants of enzymes involved in the folate pathway might be expected to have an impact on neural tube defect (NTD) risk. Given its key role in folate metabolism, the methylenetetrahydrofolate dehydrogenase 1 (MTHFD1) gene could represent an attractive candidate in NTD aetiology. In this study, the impact of the MTHFD1 1958G>A polymorphism on NTD risk in the Italian population was examined both by hospital-based case-control and family-based studies. The MTHFD1 1958G>A polymorphism was genotyped in 142 NTD cases, 125 mothers, 108 fathers and 523 controls. An increased risk was found for the heterozygous 1958G/A (OR=1.69; P=0.04) and homozygous 1958A/A (OR=1.91; P=0.02) genotypes in the children. Significant association was also found when combined 1958G/A and 1958A/A genotypes of cases were compared with the 1958G/G genotype (OR=1.76; P=0.02). The risk of an NTD-affected pregnancy of the mothers was increased 1.67-fold (P=0.04) only when a dominant effect (1958G/A or 1958A/A vs 1958G/G) of the 1958A allele was analysed. The combined TDT/1-TDT (Z=2.11; P=0.03) and FBAT (Z=2.4; P=0.01) demonstrated a significant excess of transmission of the 1958A allele to affected individuals. In summary, our results indicate that heterozygosity and homozygosity for the MTHFD1 1958G>A polymorphism are genetic determinants of NTD risk in the cases examined.
Similar content being viewed by others
Introduction
Neural tube defects (NTDs) are one of the most common human congenital malformations in newborn children, affecting annually approximately 1 in 1,000 newborns in Italy (Mastroiacovo and Bianchi 1991) and 200,000 newborns or more worldwide (Moore et al. 1997). Myelomeningocele, commonly called Spina Bifida, is the most common form of NTD. Periconceptional supplementation with folic acid reduces a women’s risk of an NTD-affected pregnancy by up to 75% (MRC Vitamin Study Research Group 1991; Czeizel and Dudas 1992). There have been numerous investigations into genes involved in folate metabolism, yielding at least one polymorphism—677C>T in the methylenetetrahydrofolate reductase (MTHFR) gene—that has been associated with an approximate doubling of the risk of NTDs (Botto and Yang 2000). However, these associations remain controversial, with several studies finding no association (Papapetrou et al. 1996; Mornet et al. 1997; Speer et al. 1997). Several other genes have been studied, including those encoding folate receptors, cystathionine-β-synthase, methionine synthase, methionine synthase reductase, and reduced folate carrier-1 (Lucock 2000; Melvin et al. 2000; Gelineau-van Waes and Finnell 2001), but many of these studies still await confirmation and warrant further investigation.
Given its central role in folate metabolism, the 5,10-methenyltetrahydrofolate-cyclohydrolase, 10-formyltetrahydrofolate synthetase (methylenetetrahydrofolate dehydrogenase: MTHFD1) could represent an attractive candidate gene in NTD aetiology. MTHFD1 is a trifunctional protein catalysing three sequential reactions in the interconversion of 1-carbon derivatives of tetrahydrofolate (THF) that are substrates for methionine, thymidylate and de novo purine biosynthesis (Tan et al. 1997). Both NAD- and NADP-dependent MTHFD have been identified (Mejia and Mackenzie 1985). MTHFD1 is an NADP-dependent cytoplasmic enzyme (often referred to as C1-THF synthase) encoded by a gene on chromosome 14q24 (Rozen et al. 1989); the MTHFD1 cDNA contains an open reading frame of 2,805 bp that encodes a protein of 935 amino acids (Hum et al. 1988). A mitochondrial trifunctional C1-THF synthase has been recently identified by Prasannan et al. (2003). The gene spans 236 kb on chromosome 6 and encodes a protein of 978 amino acids, including an N-terminal mitochondrial signal sequence. The mitochondrial isozyme is 61% identical to the human cytoplasmic isoform (Prasannan et al. 2003).
Hol et al. (1998) have analysed MTHFD1 cDNA sequences of familial and sporadic cases of NTDs for the presence of mutations. Two amino acid substitutions were identified. The first (R293H) was detected in a patient with familial Spina Bifida and not in 300 control individuals. The second change, a 1958G>A substitution polymorphism resulting in replacement of the arginine residue at position 653 by glutamine (R653Q), turned out to be present in both patients and controls with similar frequencies. More recently, Brody et al. (2002) demonstrated that MTHFD1 1958G>A polymorphism is a maternal risk factor for NTD risk in the Irish population. Mothers who possess two copies of the MTHFD1 1958A allele have an increased risk of an NTD-affected pregnancy. There was also a suggestion that the MTHFD1 1958A allele decreases fetal viability (Brody et al. 2002).
In the present study, we have attempted to replicate this finding by studying the impact of the MTHFD1 1958G>A polymorphism on NTD risk in the Italian population in hospital-based case-control and family-based studies.
Materials and methods
Study population
The NTD study population consisted of children and their parents seeking treatment at the Spina Bifida Centre of the Gaslini Children’s Hospital in Genoa, from May 2004 to the present. The Spina Bifida Centre of Gaslini Hospital has recruited children with NTDs from throughout Italy since 1976, and it sees about 150 new cases annually from both the north and the south of Italy. Of the 165 NTD families ascertained for the 1-year period, 142 (86%) agreed to participate and were enrolled. For the purposes of this study, 91 complete NTD triads and 51 incomplete triads, in which DNA was not available from all three family members (51 additional children with NTD, 34 mothers, 17 fathers) were eligible. Information about the type of defect was available for all the children with NTDs, and the cases group included 117 (82%) children (59% females; median age 12 years, range 1–26 years) affected by lumbar and sacral myelomeningocele (L1–S2 levels), 8 (6%) children with lipomyeloschisis, and 17 (12%) children with spina bifida occulta.
Of the 523 control subjects, 208 (40%) were randomly selected children who were admitted to the Gaslini Children’s Hospital for miscellaneous illnesses (orthopaedic, otolaryngeal, dental disorders, acute surgical conditions, and trauma). The other 315 control subjects (60%) were healthy young adults who had contributed samples to the blood donor bank of the Gaslini Institute. None had a first-degree relative with an NTD. The samples from all control subjects were anonymous; information associated with these samples (children and adults alike) included sex, region of birth, and age. All participants were Italian with antecedents from all parts of the country. Individuals born in Sardinia were excluded.
The local ethical committee approved the protocol and written consent was obtained from all patients, parents, and control individuals.
Genetic analysis
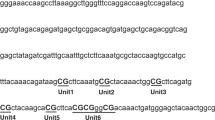
Genomic DNA was extracted from fresh blood samples using the GenEluteTM mammalian genomic DNA miniprep kit (Sigma, Taufkirchen, Germany). The presence of the MTHFD1 1958G>A polymorphism was investigated by restriction fragment length polymorphism (RFLP) assay as described by Hol et al. (1998). The digested PCR fragments were analysed by ethidium bromide-stained 4% MetaPhor agarose (FMC BioProducts, Rockland, ME) gel electrophoresis. Repeat genotyping assays were performed on all samples that gave equivocal genotypes.
Statistical analysis
Allele frequencies in the NTD patients, mothers, fathers, and controls were determined by counting alleles and calculating proportions. Differences in genotype and allele frequency were evaluated by χ2 analysis. The Hardy–Weinberg equilibrium (HWE) analysis was tested using χ2 statistics for goodness of fit (1 degree of freedom). Logistic regression analysis was used to estimate the odds ratio (OR) for the presence of mutation MTHFD1 1958G>A in patients and controls. The OR was calculated with 95% confidence interval (CI) and the wild-type pattern was used as a reference. A codominant (the three genotypes studied separately), a dominant (1958A/A or 1958G/A genotypes compared with 1958G/G genotype) and a recessive (1958A/A genotype compared with 1958G/G or 1958G/A genotype) model for the effect of the 1958G>A variant was examined. Statistical analysis was performed using SPSS for Windows (SPSS, Chicago, IL).
The attributable fraction, representing the proportion of cases in the target population that is attributable to the presence of the mutation(s), was estimated using the equation proposed by Miettinen (1974): (AF=[fCa (OR-1)]/OR), where fCais the fraction of cases with the genotype(s) under study (1958G/A or 1958A/A) and OR is the associated OR. Power computations were performed employing the calculator available at http://calculators.stat.ucla.edu/powercalc/.
Three different statistical tests were applied for family-based studies: classical transmission disequilibrium test (TDT) (Spielman et al. 1993), combined TDT/1-TDT (Sun et al. 1999), and the family-based association test (FBAT) (Rabinowitz and Laird 2000). For TDT, we used 91 completed triads. Moreover, owing to 51 incomplete families, we applied the combined TDT/1-TDT test, which combines data from families in which both parental genotypes are available and families in which only one parental genotype is available. We also used the FBAT program (version 1.5.5; http://www.biostat.harvard.edu/~fbat/fbat.htm), which allows testing for association even if no parental genotype data are available. Based on the results of the unrelated case-control analysis, a biallelic test was performed using dominant inheritance model.
Results
Case-control study
Table 1 shows the MTHFD1 genotype distributions, allele frequencies, and the results of HWE analysis. The genotype distribution for the MTHFD1 1958G>A mutation in the controls was as expected according to the HWE (P=0.41). The frequency of the A allele of the MTHFD1 1958G>A mutation was 0.487 among control individuals. No statistically significant heterogeneity was found in the allelic frequencies by type of controls (children or young adults) (P =0.66) or by sex (P =0.54). Moreover, we found that the genotype distribution obeyed the constraints of HWE also in NTD cases and their parents. Chi squared analysis revealed that allele frequencies were significantly different between cases and controls (P =0.02; data not shown).
To evaluate the impact of the MTHFD1 1958G>A variant on NTD risk, we calculated the OR and 95% CI (Table 2). We found a significant increased risk for both heterozygous (OR=1.69; 95% CI: 1–2.77; P =0.04) and homozygous (OR=1.91; 95% CI: 1.1–3.29; P =0.02) genotypes in the children. Moreover, when the dominant model was applied (1958G/A or 1958A/A vs 1958G/G), there was a nominally significant increase in NTD risk (OR=1.76; 95% CI: 1.1–2.82; P =0.02). A recessive effect of the 1958A variant (1958A/A vs 1958G/G or 1958G/A) in cases was not significant (OR=1.32; P =0.21). In cases homozygous for the 1958A allele, the power to detect an OR of 1.91 was 85% (α<0.05, frequency of the risk allele=0.487, two-sided); thus, the likelihood of a type II error in our data set is low. We calculated that the proportion of NTD cases that could be attributed under a dominant effect model of the 1958A variant was about 35.6% (population attributable fraction).
A significantly elevated risk of NTD was observed in mothers who were heterozygous for the MTHFD1 G1958>A variant (OR=1.73; 95% CI: 1.04–2.89; P =0.04). A maternal 1958A/A homozygous genotype was not a significant independent contributor to NTD risk (OR=1.54; 95% CI: 0.86–2.77; P =0.15). Nevertheless, when a dominant effect (1958G/A or 1958A/A vs 1958G/G) of the 1958A allele of the mothers was considered, we found a 1.67-fold increased risk (P =0.04). On the contrary, no significant association was seen when the recessive model of the 1958A variant of the mothers was applied (1958A/A vs 1958G/G or 1958G/A; OR=1.05; 95% CI:0.67–1.64; P =0.91).
No increased risk was found for the genotype of the fathers, regardless of the genetic model applied (codominant, dominant or recessive).
Family-based study
The results of family-based studies are presented in Table 3. The 142 NTD families included 91 for whom maternal and paternal DNA samples were available and 51 for whom only maternal or only paternal samples were obtained (incomplete families). We investigated whether there was any bias in the transmission of the A allele using a classical TDT test (Spielman et al. 1993), which tests allele transmission from heterozygous parents regardless of case genotype outcome. TDT indicated that, from 96 heterozygous parents, the A allele was transmitted 55 times (57%), whereas the G allele was transmitted 41 times (43%). This bias in A allele transmission is only suggestive of an effect (P =0.06). Given the high number of incomplete families, we applied the combined TDT/1-TDT test, which combines data from families in which both parental genotypes are available and families in which only one parental genotype is available (Sun et al. 1999). In total, 51 families in which only one parent was available, and 91 triads were used for analysis by the combined TDT/1-TDT test. A significant excess of transmission of the A allele to affected individuals was found (Z score=2.11; P =0.03). More significant association was found by FBAT analysis (Z=2.4; P=0.01, for a dominant model).
Discussion
The aim of this study was to evaluate the role of a common polymorphism of the MTHFD1 gene, the 1958G>A variant, on the risk of NTD in the Italian population. The degree of risk was assessed both by hospital-based case-control and family-based studies.
The frequency of the 1958A allele in our controls was 0.487, which is comparable to the frequencies of 0.450 found in the control populations in Ireland and Germany (Hol et al. 1998; Brody et al. 2002). The frequency reported here is higher than that (0.39) found in a small sample of Italian DNAs from a CEPH diversity panel (Shi et al. 2003). This discrepancy may be due to the small size of the individual groups included in that panel compared to the current study.
The case-control study has indicated that cases carrying one (1958G/A) or two (1958A/A) alleles for the MTHFD1 1958G>A polymorphism have a significantly increased risk of NTD in comparison with individuals who have no copies of this polymorphism (1958G/G homozygotes). The magnitude of this association, i.e. the OR, was similar both when the genotypes were analysed separately (codominant model; 1958G/A=1.69; 1958A/A=1.91) and under a dominant model of action (1958G/A or 1958A/A=1.76). However, the significance of the association studies is not impressive enough to allow definitive conclusions regarding whether this polymorphism is a risk factor for NTD. We found no association between any of the fathers’ genotypes and NTDs. When we analysed maternal genotypes, a significant dominant maternal effect was observed (1.67-fold increased risk in mothers carrying 1958G/A or 1958A/A genotypes vs 1958G/G); no significant association was found when homozygosity of the mothers was considered separately (1958A/A vs 1958GG), or when a recessive model within mothers (1958A/A vs 1958G/A or 1958G/G) was analysed.
Furthermore, the results of the present case-control study are not in agreement with the report of Brody et al. (2002). In fact, in the Irish study the authors conclude that maternal MTHFD1 1958A/A homozygosity is a risk factor for NTDs, but they did not observe any difference in allele or genotype frequencies between the case and control groups.
Our finding of an association between the MTHFD1 1958G>A genotype of children and NTDs appears to be reasonably powered. Thus, a possible reason for the discrepancy between our results and the Irish study may be due to population heterogeneity and, therefore, our results apply only to the Italian population. It is also possible that environmental differences can explain the discrepancies between the Irish and Italian case frequencies.
Three different statistical tests were applied to the family-based studies, only two of which, TDT/1-TDT and FBAT, yielded significant evidence for association between the MTHFD1 G1958A polymorphism and NTDs. Despite their significance, these results should be interpreted with caution since the family-based studies were less powerful than the case-controls studies and need to be confirmed in further studies.
Although association studies demonstrated that the maternal MTHFD1 1958A/A genotype has no appreciable influence on NTD risk as an independent risk factor, it could be important when other factors are present, including the 1958A/A of the child. On the basis of the data presented here (association studies), the question of the extent, if any, to which maternal MTHFD1 1958A/A genotype contributes independently to NTD outcome, should be addressed by studies including much larger numbers of mother-child pairs, or by application of TDT to three-generation families that include heterozygous maternal grandparents, as suggested by Mitchell (1997).
The rationale for a possible association between MTHFD1 genotype and NTD risk is based on the important role of the MTHFD1 protein in folate pool maintenance. The MTHFD1 1958G>A substitution affects the synthetase domain of the enzyme, possibly altering nucleotide pools available for DNA synthesis and, thus, affect cell division. No specific biochemical phenotype has been associated with this genetic variant. The MTHFD1 1958G>A polymorphism is unlikely to have a direct effect on folate and homocysteine levels (Brody et al. 2002). Nevertheless, this polymorphism may produce an effect at the cellular level without causing perturbations in plasma metabolites.
In summary, our results indicate that the MTHFD1 1958G/A and 1958A/A genotypes in NTD cases are genetic determinants of NTD risk with dominant action. Further investigations are warranted to clarify if maternal genotype may confer risk, independently, or in the presence of a mutant MTHFD1 genotype in the children. Clearly, our understanding of the role of the MTHFD1 gene in NTD risk is incomplete, and studies of other variants in this gene that were not examined here are required.
References
Botto LD, Yang Q (2000) 5,10-Methylenetetrahydrofolate reductase gene variants and congenital anomalies: a HuGE review. Am J Epidemiol 151:862–877
Brody LC, Conley M, Cox C, Kirke PN, McKeever MP, Mills JL, Molloy AM, O’Leary VB, Parle-McDernott A, Scott JM, Swanson DA (2002) A polymorphism, R653Q, in the trifunctional enzyme methylenetetrahydrofolate dehydrogenase-methenyltetrahydrofolate cyclohydrolase-formyl-tetrahydrofolate synthetase is a maternal genetic risk factor for neural tube defects. Report of the Birth Defects Research Group. Am J Hum Genet 71:1207–1215
Czeizel A, Dudas I (1992) Prevention of the first occurence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 327:1832–1835
Gelineau-van Waes J, Finnell RH (2001) Genetics of neural tube defects. Semin Pediatr Neurol 8:160–164
Hol FA, van der Put NM, Geurds MP, Heil SG, Trijbels FJ, Harnel BC, Mariman EC, Blom HJ (1998) Molecular genetic analysis of the gene encoding the trifunctional enzyme MTHFD (methylenetetrahydrofolate dehydrogenase-methenyltetrahydrofolate cyclohydrolase-formyl-tetrahydrofolate synthetase) in patients with neural tube defects. Clin Genet 53:119–125
Hum DW, Bell AW, Rozen R, Mackenzie RE (1988) Primary structure of a human trifunctional enzyme. Isolation of a cDNA encoding methylenetetrahydrofolate dehydrogenase-methenyltetrahydrofolate cyclohydrolase-formyl-tetrahydrofolate synthetase. J Biol Chem 263:15946–15950
Lucock M (2000) Folic acid: nutritional biochemistry, molecular biology, and role in disease processes. Mol Genet Metab 71:121–138
Mastroiacovo PP, Bianchi F (1991) The descriptive epidemiology of congenital defects at birth in Italy. Epidemiol Prev 13:94–103
Mejia NR, Mackenzie RE (1985) NAD-dependent methylenetetrahydrofolate dehydrogenase is expressed by mortal cells. J Biol Chem 260:14616–14620
Melvin EC, George TM, Worley G, Franklin A, Mackey J, Viles K, Shah N, Drake CR, Enterline DS, McLone D, Nye J, Oakes WJ, McLaughlin C, Walker ML, Peterson P, Brei T, Buran C, Aben J, Ohm B, Bermans I, Qumsiyeh M, Vance J, Pericak-Vance MA, Speer MC (2000) Genetic studies in neural tube defects. NTD Collaborative Group. Pediatr Neurosurg 32:1–9
Miettinen OS (1974) Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol 99:325–332
Mithchell LE (1997) Differentiating between fetal and maternal genotypic effects, using the transmission test for linkage disequilibrium. Am J Hum Genet 60:1006–1007
Moore CA, Li S, Li Z, Hong SX, Gu HQ, Berry RJ, Mulinare J, Erickson JD (1997) Elevated rates of severe neural tube defects in a high prevalence area in northen China. Am J Med Genet 73:113–118
Mornet E, Muller F, Lenvoisè-Furet A, Delezoide AL, Col JY, Simon-Bouy B, Serre JL (1997) Screening of the C677T mutation on the methylenetetrahydrofolate reductase gene in French patients with neural tube defects. Hum Genet 100:512–514
MRC Vitamin Study Research Group (1991) Prevention of neural tube defects. Results of the MRC Vitamin Study. Lancet 2:131–137
Papapetrou C, Linch SA, Burn J, Edwards YH (1996) Methylenetetrahydrofolate reductase and neural tube defects. Lancet 348:58
Prasannan P, Pike S, Peng K, Shane B, Appling D (2003) Human mitochondrial C1-tetrahydrofolate synthase: gene structure, tissue distribution of the mRNA, and immunolocalization in Chinese hamster ovary cells. J Biol Chem 278:43178–43187
Rabinowitz D, Laird N (2000) A unified approach to adjusting association tests for population admixture with arbitrary pedigree structure and arbitrary missing marker information. Hum Heredity 50:211–223
Rozen R, Barton D, Du J, Hum DW, MacKenzie RE, Francke U (1989) Chromosomal localization of the gene for the human trifunctional enzyme, methylenetetrahydrofolate dehydrogenase-methenyltetrahydrofolate cyclohydrolase-formyl-tetrahydrofolate synthetase. Am J Hum Genet 44:781–786
Shi M, Caprau D, Romitti P, Christensen K, Murray JC (2003) Genotype frequencies and linkage disequilibrium in the CEPH human diversity panel for variants in folate pathway genes MTHFR, MTHFD, MTRR, RFC1, and GCP2. Birth Defects Res A 67:545–549
Speer MC, Worley G, Mackey JF, Melvin E, Oakes WJ, George TM (1997) The thermolabile variant of methylenetetrahydrofolate reductase (MTHFR) is not a major risk factor for neural tube defect in American Caucasians. Neurogenetics 1:149–150
Spielman RS, McGinnis RE, Ewens WJ (1993) Transmission test for linkage disequilibrium: the insulin gene region and insulin-dependent diabetes mellitus (IDDM). Am J Hum Genet 52:506–516
Sun F, Flanders WD, Yang Q, Khoury MJ (1999) Transmission disequilibrium test (TDT) when only one parent is available: the 1-TDT. Am J Epidemiol 150:97–104
Tan LU, Drury EJ, Mackenzie RE (1997) Methylenetetrahydrofolate dehydrogenase-methenyltetrahydrofolate cyclohydrolase-formyl-tetrahydrofolate synthetase; a multifunctional protein from porcine liver. J Biol Chem 252:1117–1122
Acknowledgements
The authors are grateful to the patients and their families, whose collaboration and understanding have made this work possible. We also thank the G.A.S.B.I. (Genitori Associati Spina Bifida Italia ONLUS) and Ruiu Ilaria for technical support. This study was supported by grants from the Ministry of Health of Italy: Ricerca Corrente 2003; Ricerca Finalizzata Ministeriale 2003; grant number: 128. The experiments described in this manuscript comply with the current laws of Italy.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Marco, P., Merello, E., Calevo, M.G. et al. Evaluation of a methylenetetrahydrofolate-dehydrogenase 1958G>A polymorphism for neural tube defect risk . J Hum Genet 51, 98–103 (2006). https://doi.org/10.1007/s10038-005-0329-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-005-0329-6
Keywords
This article is cited by
-
MTHFD1 polymorphism as maternal risk for neural tube defects: a meta-analysis
Neurological Sciences (2015)
-
Replication and exploratory analysis of 24 candidate risk polymorphisms for neural tube defects
BMC Medical Genetics (2014)
-
Genetic evidence in planar cell polarity signaling pathway in human neural tube defects
Frontiers of Medicine (2014)
-
Polymorphisms in FZD3 and FZD6 genes and risk of neural tube defects in a northern Han Chinese population
Neurological Sciences (2014)
-
Evaluation of common genetic variants in 82 candidate genes as risk factors for neural tube defects
BMC Medical Genetics (2012)