Abstract
Infectious diseases caused by chlamydia or schistosomes are a major health problem worldwide, and particularly so in developing countries. The lack of appropriate vaccines renders the search for potent natural products against these disease-causing agents an urgent endeavor. Sponge-associated actinomycetes represent a rich reservoir for natural products. Among them, members of the genus Streptomyces are capable of synthesizing an impressive array of diverse natural products with a wide variety of biological activities. The naphthacene glycoside SF2446A2 was isolated from the calcium alginate beads culture of Streptomyces sp. strain RV15 that had originally been obtained from the Mediterranean sponge Dysidea tupha. Its structure was identified by spectroscopic analysis and MS and comparison with the literature data. SF2446A2 showed inhibitory activity against Chlamydia trachomatis and was able to inhibit the primary infection in a dose-dependent manner, as well as progeny formation. Moreover, it caused disruptive effects on the surface area of Schistosoma mansoni and affected the gonads by impairing oogenesis and spermatogenesis. Our current study demonstrates that sponge-associated actinomycetes are capable of providing compounds with new pharmacological activities and with relevance to drug discovery.
Similar content being viewed by others
Introduction
Chlamydia trachomatis is a gram-negative, obligate, intracellular, human pathogen and is one of the main causative agents of sexually transmitted infections and infections of the upper inner eyelid (trachoma).1, 2 The developmental cycle of Chlamydia occurs in a specialized vacuole, the so-called ‘inclusion’. Upon infection, Chlamydia suppresses host-cell apoptosis to escape the immune response.3 The infection is initiated by the elementary bodies (EBs), an infectious and metabolically inert chlamydial form. Within the inclusion the EBs differentiate into a replicative form, the reticulate bodies (RBs). At the end of the cycle, a differentiation of the RBs back to the EBs occurs, thus enabling the new progeny to be released and initiating a new infectious cycle. RBs are also able to convert to a persistent non-replicative state, which leads to a long-term relationship with the host cell.4 Re-infection and persistence are the reasons for prolonged therapy of chlamydial infections, in which different antibiotics including tetracyclines, azithromycin or erythromycin are applied. An incorrect administration of antimicrobial therapy is known to induce persistence of Chlamydia.5 Additionally, a vaccine against human Chlamydia is not available, which makes it a relevant model organism in the search for novel classes of antimicrobial agents.
Parasites of the genus Schistosoma cause schistosomiasis, an infectious disease of humans and animals. Eggs produced by schistosome couples are mainly responsible for the pathologic consequences of the disease. The number of patients suffering from schistosomiasis ranks second only to malaria with more than 240 million people being affected in the tropical and subtropical regions.6, 7 A vaccine is not available yet and Praziquantel (PZQ) is the only widely used medicine to treat patients. Since it is used for a long time also in mass treatment programs, there is future concern regarding emerging resistance.8 Therefore, there is a need for new treatment options, which requires the identification of candidate targets and/or new compounds affecting survival and/or egg production.
Members of the bacterial clade Actinomycetes have been contributed significantly to the discovery of clinically useful antibiotics.9 More recently, sponge-associated actinomycetes have shown to be a rich source for biomedically relevant natural products.10, 11 Biological activities such as antibacterial, antifungal, antiparasitic, antimalarial, immunomodulatory, anti-inflammatory, antioxidant and anticancer activities were reported from sponge-associated actinomycetes.12, 13, 14, 15, 16 These bioactivities are mediated by diverse groups of chemical compounds including polyketides, alkaloids, peptides and terpenes.14, 15, 17, 18, 19 The compound SF2446A2, a naphthacene glycoside previously reported from soil-derived Streptomyces sp. strain SF2446, was found to exhibit strong activity against Gram-positive bacteria and several mycoplasma strains including the macrolide-resistant strain Mycoplasma gallisepticum.20 Here, we report the isolation of SF2446A2 from the calcium alginate bead culture of a marine sponge-derived Streptomyces sp. strain RV1521 and present evidence of new anti-chlamydial and anti-schistosomal activities of SF2446A2 (Figure 1).
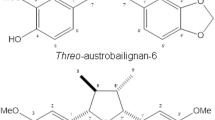
Structure of SF2446A2.26
Materials and Methods
Bacterial fermentation
Streptomyces sp. strain RV15 had originally been isolated from the marine sponge Dysidea tupha offshore Rovinj, Croatia.21 Cells of well-grown culture (5 days) of Streptomyces sp. strain RV15 (8 l) were collected by centrifugation at 8000 r.p.m. for 10 min and the pellet was mixed with 4% (w/v) sodium alginate, containing HEPES buffer (1%). Sodium alginate mixture was slowly dropped with a 5-ml syringe into 1.5% (w/v) CaCl2 at 4 °C with stirring. The produced beads were then washed three times with sterile distilled water. In all, 2.4 l of calcium alginate beads with immobilized bacteria was transferred to eight Erlenmeyer flasks (2 l) each containing 1.2 l of ISP2 medium and incubated at 30 °C with shaking (150 r.p.m.) for 7 days. After filtration, the beads were extracted by shaking with methanol for 3 h, and then filtered. The supernatant was extracted with 7 l ethyl acetate.
Extraction and isolation
Bioassay-guided fractionation of the ethyl acetate extract (6.5 g) against Chlamydia trachomatis was performed by normal phase silica gel chromatography and the bioactive fraction (765 mg) eluted with 45% chloroform in methanol was further chromatographed on sephadex LH 20 using gradient of methanol:water from 5 to 100% water. The antichlamydially active fraction (48 mg) eluted with 65% methanol in water was further purified by preparative HPLC using an acetonitrile (MeCN) and water solvent mixture complemented by 0.05% trifluoroacetic acid (10% MeCN:H2O to 100% MeCN over 20 min at a flow rate of 10 ml min−1) to yield the compound SF2446A2.
Cell culture
HeLa cells were cultured in RPMI-1640 media (Gibco/Life Technologies, Paisley, UK) supplemented with 10% (v/v) h.i. fetal bovine serum (Biochrom, Berlin, Germany) at 37 °C under 5% CO2. Chlamydia trachomatis C2 (L2/434/BU), a green fluorescent protein-expressing strain, was generated essentially as described in Wang et al.22
Antibodies
β-Tubulin antibody was purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA) and the OmpA antibody was raised in rabbits against the cytosolic domain of OmpA carrying a His tag. Phalloidin647 was obtained from Life Technologies (Carlsbad, CA, USA) and DAPI (4′,6-diamidino-2-phenylindole) from Sigma-Aldrich Co. (St Louis, MO, USA).
Bioactivity testing against Chlamydia trachomatis
The assay was performed in black bottom 96-well plates (Greiner/Sigma-Aldrich Co., St Louis, MO, USA). In all, 1.2 × 104 HeLa cells were seeded per well. Compounds solubilized in dimethyl sulfoxide (DMSO) were added to final concentrations ranging from 1.6 μm to 40 μm. The same amount of DMSO and 11.25 μm tetracycline were added to control samples. After 1 h incubation, cells were infected with C. trachomatis at multiplicity of infection 1 for 24 h at 35 °C in media supplemented with 5% h.i. fetal bovine serum in the presence of the compounds. The cells were then washed with phosphate-buffered saline and fixed with 4% PFA. After washing, cell nuclei were stained with DAPI (0.2 ng ml−1) and the actin cytoskeleton with Phalloidin647. The analysis has been performed with the Operetta high content imaging system (Perkin Elmer, Waltham, MA, USA) at six pictures per well and × 20 magnification. The ratio between HeLa cell surface and the C. trachomatis inclusion area was calculated by the system. In all, 11 × 103 cells have been analyzed on average.
EB progeny assay
In total, 4 × 105 HeLa cells were seeded in two 12-well plates (plates A and B), which were treated in the same manner. Treatment of the cells with the compounds and infection with bacteria were performed as described in the bioactivity assay. Plate A (primary infection) was harvested after 24 h using Laemmli buffer. Forty-eight hours after infection, to allow C. trachomatis to finalize the developmental cycle, host cells of plate B were lysed with glass beads. The progeny infectious particles were released and 2 μl of the suspension was used to infect fresh HeLa monolayers in a 12-well plate (plate C, progeny infection). After 24 h of infection, the plate C was harvested in the same manner as the plate A. Cell lysates were analyzed by western blot, using antibodies against β-Tubulin and the chlamydial protein OmpA.
Bioactivity testing against Schistosoma mansoni
All animal experiments have been approved by the Regional Council (Regierungspraesidium) Giessen (V54-19 c 20/15 c GI 18/10) and were performed in accordance with the European Convention for the Protection of Vertebrate Animals used for experimental and other scientific purposes.23 Schistosoma mansoni couples were obtained from Syrian hamsters (Mesocricetus auratus) by hepatoportal perfusion 46 days after infection with cercariae. They were then maintained in groups of 20 couples at 37 °C with 5% CO2 in 60 mm diameter Petri dishes (Greiner, Frickenhausen, Germany) with M199 medium (Gibco) supplemented with 10% Newborn Calf Serum (NCS, Sigma), 1% HEPES (Roth, Karlsruhe, Germany; [1M]) and 1% ABAM (GE Healthcare, Darmstadt, Germany; [10 000 units penicillin, 10 mg streptomycin, 25 mg amphotericin B per ml]) as described before.24 The inhibitor experiments were carried out in 6-well plates (Greiner bio-one) with 10 couples per well and a volume of 5 ml (medium+substance SF2446A2). The concentrations used were 1, 10, 50 and 100 μm. The substance was dissolved and diluted in DMSO (Sigma-Aldrich). As the negative control, the same volume of DMSO was added as in the test wells. Praziquantel (PZQ, TCI Chemicals, Eschborn, Germany) was used as a positive control in a concentration of 100 μm for reasons of better comparability to the effect of SF2446A2. SF2446A2 was completely dissolved in DMSO but upon addition to the medium the 100 μm concentration took on a rubber-like consistency. After a few minutes it dissolved in the medium. Every 24 h, medium and substance were renewed. For this purpose, the worms were transferred to newly prepared 6-well plates and the eggs produced during the preceding 24 h were counted. An evaluation was done every 24 h via bright-field microscopy. Pairing stability, gut peristalsis, vitality, motility and egg production were examined. Any dead worms were immediately fixed in AFA fixative (ethanol (70%) 95%, formalin 3%, glacial acetic acid 2%) for subsequent confocal laser scanning microscopy. The rest of the treated worms were fixed after 72 h. All of the worms were stained for 30 min in carmine red (Merck, Darmstadt, Germany). Destaining took place in acidic ethanol (70% ethanol+2.5% hydrogen chloride) and dehydration happened in ascending ethanol concentrations (70, 90, 100%). Worms were embedded in Canada balsam solution (Sigma-Aldrich) on glass slides for confocal laser scanning microscopy (Leica TSC SP2; Leica Microsystems, Wetzlar, Germany) analysis as described before.25
Results and discussion
To see the effect of different fermentation approaches on bioactivity profile, Streptomyces sp. RV15 strain was fermented in calcium alginate beads, solid agar as well as in broth ISP 2 medium and the secondary metabolites were collected with ethyl acetate. Ethyl acetate extracts were tested against a wide range of bacteria, fungi, parasites, adult Schistosoma and Chlamydia. The ethyl acetate extract of calcium alginate beads was found to be active against Gram-positive bacteria, Schistosoma and Chlamydia. Bioassay-guided fractionation of the calcium alginate ethyl acetate extract was performed against adult Schistosoma and C. trachomatis, on normal-phase silica gel chromatography followed by gel filtration on Sephadex LH-20 and final purification on reversed-phase HPLC to afford SF2446A2 with a molecular formula of C34H35NO15 by high-resolution electrospray ionisation time-of-flight mass spectrometry (HR-ESI-TOF-MS) analysis (m/z 698.208 for [M+H]+). A database search using AntiMarin, a merger database of Antibase (Laatsch H. Antibase Version 4.0—The Natural Compound Identifier. Wiley-VCH Verlag GmbH & Co. KGaA, Weinheim, Germany, 2012) for microbial secondary metabolites as well as higher fungi and MarinLit for marine natural products (Blunt J. MarinLit. University of Canterbury, New Zealand, 2012) suggested that this mass coincided with that of SF2446A2 or its isomer SF2446A1. After checking the spectroscopic data (see SI, 1H, 13C, COSY, HMBC and ROESY), the compound was confirmed to be SF2446A2.26 The compound was tested against Staphylococcus aureus 8325 and showed activity with IC50 of 8 μm which was previously reported.26 Cytotoxicity was also tested against J774.1 macrophages and no cytotoxicity was found (IC50 of >200 μm).
Inhibitory activity of SF2446A2 against Chlamydia trachomatis
SF2446A2 was tested for its antichlamydial activity using infection of epithelial HeLa cells with Chlamydia trachomatis. The infection was performed in the presence of 1.6, 8.0 and 40.0 μm of SF2446A2 and the size of chlamydial inclusions was determined using an automated microscopy assay. Tetracycline at the concentration of 11.25 μm was used to confirm the reliability of the assay. The compound inhibited the formation and growth of chlamydial inclusions in a dose-dependent manner. The inclusion size was reduced with increasing compound concentration (Figures 2a and b), but there was no fragmentation of inclusions, such as was observed with other anti-chlamydial agents (data not shown). Similar to the effect of the tetracycline (Tet) control, inclusions were also not observed at the highest concentration of 40 μm (Figure 2a). We then tested the effect of the SF2446A2 for the concentrations ranging between 8 and 40 μm, but we observed that the maximum effect of the substance was obtained already at slightly above 10 μm (data not shown). Therefore, we tested the substance concentrations between 0.5 and 10 μm and determined the IC50 value (Figures 2c and d). The IC50 value, defined as the concentration at which the size of chlamydial inclusion relative to the cell surface was reduced by 50%, was 4.03±0.35 μm (Figure 2c).
SF2446A2 inhibited chlamydia infection in a dose-dependent manner. (a) HeLa cells were infected with C. trachomatis expressing green fluorescent protein (GFP) at an multiplicity of infection of 1 for 24 h in the presence of DMSO and 40 μm SF2446A2. The chlamydial inclusions appear in the green channel (arrow), cell nuclei were stained with DAPI (blue channel) and the actin cytoskeleton with Phalloidin647 (red channel). Scale bars are 25 μm. (b, c) HeLa cells were infected with C. trachomatis for 24 h in the presence of 1.6, 8.0 and 40.0 μm (b) or 0.5, 1, 2, 4, 6, 8 and 10 μm (c) of SF2446A2. DMSO was used as a negative control, and tetracycline (Tet) as a positive control at 11.25 μm. The graph represents mean values±s.d. of the surface of inclusions relative to the cell surface from at least three independent repetitions of the experiment. (d) The calculated percentage of inclusion area of the bioactivity assay from (c) was used to determine the IC50 of SF2446A2. A logarithmic trend line was used to calculate the agent concentration at 50% inclusion surface. A full color version of this figure is available at The Journal of Antibiotics journal online.
Besides the effect of SF2446A2 on the inclusion formation, the compound showed an impact on the ability of C. trachomatis to create viable progeny (Figures 3a and b). This effect of the compound on the developmental cycle of Chlamydia was analyzed via the EB progeny assay. For this purpose, HeLa cells were infected with C. trachomatis in the presence of DMSO and tetracycline (Tet) controls and in the presence of 1.6, 8 and 40 μm SF2446A2, respectively. For the analysis of the EB primary infection, infected cells were harvested after 24 h. A set of parallel samples was infected for 48 h, and new cells were infected with the EB progeny without any treatment. After 24 h, these cells were harvested. A western blot was performed with the cell lysates using an anti-β-tubulin antibody as a loading control. For the determination of the chlamydial content, an antibody was applied against the chlamydial protein OmpA.
SF2446A2 affects the primary and progeny chlamydia infection in a dose-dependent manner. (a) Western blot resulting from the EB progeny assay showing the EB primary (Prim) and progeny (Prog) infection of C. trachomatis in the presence of the DMSO and Tetracycline (Tet) controls and depicted SF2446A2 concentrations. β-Tubulin antibody staining served as a loading control and an antibody staining against the chlamydial protein OmpA was used to determine the chlamydial content. (b) The signals from the western blot as described in (a) were quantified using Image J. The measured OmpA intensities were normalized with the β-tubulin intensities, where the normalization factor was calculated by dividing the β-tubulin intensities with the intensity of the β-tubulin DMSO control. The graph represents mean values±s.d. from three independent experiments.
The results showed that the compound affected the primary infection in a dose-dependent manner, which confirmed our previous results (Figures 3a and b). Higher compound concentration correlated with a reduction of detected chlamydial protein OmpA. Additionally, the progeny was less infectious after SF2446A2 treatment and its formation was affected. At the highest compound concentration of 40 μm almost no viable progeny was formed. Thus, the compound not only inhibited the formation of chlamydial inclusions, but also affected the developmental cycle of chlamydia.
SF2446A2 effects on adult Schistosoma mansoni in vitro
To test the effect of SF2446A2 on adult S. mansoni in vitro, concentrations between 1 and 100 μm were applied. Below 50 μm, obvious changes were not observed compared with an untreated control. Schistosoma mansoni couples treated with 50 μm SF2446A2 produced 351 eggs after 24 h, which was in the range of DMSO-treated control worms. The percentage of distorted eggs within the control was 6%, however, in treated worms it was more than twice as high (13%) (Table 1). The number of deposited eggs in the control experiments slightly increased within 72 h up to 462, whereas the percentage of malformed eggs remained constant at 5%. In contrast, egg deposition was dramatically reduced down to five eggs already after 48 h, and in parallel an increase in distorted eggs up to 30% was observed in treated couples. After 72 h of treatment at the same concentration, egg production was completely abolished, which was also observed following treatment with 100 μm after 24 h (Table 1). The same effect was observed using 100 μm of PZQ as a positive control. With respect to the quantity and quality of deposited eggs, the effects of 50 μm SF2446A2 were paralleled by the appearance of remarkable phenotypic changes (Figure 4). In contrast to the controls, all treated couples were separated, mostly detached from the Petri dish, and showed reduced physical activity as well as gut peristalsis already after 24 h. This indicated a significant reduction of worm fitness following treatment. SF2446A2-treated male worms appeared cloddish (shortened, swollen and more compact), (data not shown). In the course of treatment, males and females appeared progressively ruffled, showed tegument damages (detachment of the tegument), and blebs (Figure 4, asterisks and black arrows), and finally seemed to be mostly lifeless. In general, the cellular content as well as the boundaries of testes and ovaries appeared disintegrated. Furthermore, testes and ovaries of SF2446A2-treated worms contained pore-like areas (Figure 4, white arrows) and comprised less immature oocytes at the anterior part of the ovary. Thus, SF2446A2 negatively influenced the vitality of treated schistosomes and caused dramatic effects on their surface area but also on the gonads affecting oogenesis and spermatogenesis. PZQ-treated control couples appeared to be lifeless and much darker due to immediate contraction without separation. In contrast to SF2446A2-treated worms, the integrity of the tegument seemed to be unaffected and ovaries as well as testes looked similar as in the DMSO-negative controls (Figure 4). This was expected since to our knowledge no effect of PZQ on the gonads of schistosomes has ever been reported.
Morphological effects of SF2446A2 on adult S. mansoni in vitro. The effects of SF2446A2 (50 μm) administered over 72 h right panels) on S. mansoni males and females were investigated by light microscopy (LM) and confocal laser scanning microscopy (CLSM magnification: × 400) in comparison with PZQ-treated controls (middle panels) and DMSO-treated (left panels) controls; gc, gynecophoral canal; gu, gut; hs, head sucker; ov, ovary; io, immature oocytes; mo, mature oocytes; te, testis; tg, tegument; tu, tubercle; sv, seminal vesicle; asterisk, detached tegument; black arrow, tegumental bleb; white arrow, pore-like structures. Scale bars: 200 μm.
Conclusions
SF2446A2 was isolated and identified from Streptomyces sp. RV15 calcium alginate beads culture that was active against C. trachomatis and S. mansoni. Our results showed that SF2446A2 exhibited anti-chlamydial potential and was able to inhibit the primary infection as well as the progeny formation in a dose-dependent manner. This implies that SF2446A2 not only inhibits the infection, but also affects the developmental cycle of chlamydia. SF2446A2 also impaired the vitality of schistosomes and induced dramatic effects on their morphology, including disruption of tegumental integrity, as well as impairment of oogenesis and spermatogenesis. These pleiotropic effects indicate the possibility of different targets of SF2446A2 in S. mansoni. These results highlight the variation in the fermentation approaches is a worthwhile procedure to find novel bioactivities. Future experiments will involve exploration on the mechanism of action of SF2446A2 in impairing development and lifecycle of the human parasites C. trachomatis and S. mansoni.
References
Somani, J., Bhullar, V. B., Workowski, K. A., Farshy, C. E. & Black, C. M. Multiple drug-resistant Chlamydia trachomatis associated with clinical treatment failure. J. Infect. Dis. 181, 1421–1427 (2000).
Stephens, R. S. The cellular paradigm of chlamydial pathogenesis. Trends Microbiol. 11, 44–51 (2003).
Sharma, M. & Rudel, T. Apoptosis resistance in Chlamydia-infected cells: a fate worse than death? FEMS Immunol. Med. Microbiol. 55, 154–161 (2009).
Beatty, W. L., Morrison, R. P. & Byrne, G. I. Persistent chlamydiae: from cell culture to a paradigm for chlamydial pathogenesis. Microbiol. Rev. 58, 686–699 (1994).
Hogan, R. J., Mathews, S. A., Mukhopadhyay, S., Summersgill, J. T. & Timms, P. Chlamydial persistence: beyond the biphasic paradigm. Infect. Immun. 72, 1843–1855 (2004).
World Health Organization Schistosomiasis. Fact sheet N° 115, (2013). Available from http://www.who.int/mediacentre/factsheets/fs115/en/ (accessed February 2014).
Fallon, P. G. Immunopathology of schistosomiasis: a cautionary tale of mice and men. Immunol. Today 21, 29–35 (2000).
Doenhoff, M. J., Cioli, D. & Utzinger, J. Praziquantel: mechanisms of action, resistance and new derivatives for schistosomiasis. Curr. Opin. Infect. Dis. 21, 659–667 (2008).
Fenical, W. & Jensen, P. R. Developing a new resource for drug discovery: marine actinomycete bacteria. Nat. Chem. Biol. 2, 666–673 (2006).
Abdelmohsen, U. R., Bayer, K. & Hentschel, U. Diversity, abundance and natural products of marine sponge-associated actinomycetes. Nat. Prod. Rep. 31, 381–399 (2014).
Eltamany, E. E. et al. New antibacterial xanthone from the marine sponge-derived Micrococcus sp. EG45. Bioorg. Med. Chem. Lett. 24, 4939–4942 (2014).
Pimentel-Elardo, S. M. et al. Anti-parasitic compounds from Streptomyces sp. strains isolated from Mediterranean sponges. Mar. Drugs 8, 373–380 (2010).
Mayer, A. M. & Hamann, M. T. Marine pharmacology in 2001—2002: marine compounds with anthelmintic, antibacterial, anticoagulant, antidiabetic, antifungal, anti-inflammatory, antimalarial, antiplatelet, antiprotozoal, antituberculosis, and antiviral activities; affecting the cardiovascular, immune and nervous systems and other miscellaneous mechanisms of action. Comp. Biochem. Physiol. Toxicol. Pharmacol. 140, 265–286 (2005).
Blunt, J. W., Copp, B. R., Keyzers, R. A., Munro, M. H. & Prinsep, M. R. Marine natural products. Nat. Prod. Rep. 30, 237–323 (2013).
Abdelmohsen, U. R. et al. Antioxidant and anti-protease activities of diazepinomicin from the sponge-associated Micromonospora strain RV115. Mar. Drugs 10, 2208–2221 (2012).
Bull, A. T. & Stach, J. E. Marine actinobacteria: new opportunities for natural product search and discovery. Trends Microbiol. 15, 491–499 (2007).
Solanki, R., Khanna, M. & Lal, R. Bioactive compounds from marine actinomycetes. Indian J. Microbiol. 48, 410–431 (2008).
Subramani, R. & Aalbersberg, W. Marine actinomycetes: an ongoing source of novel bioactive metabolites. Microbiol. Res. 167, 571–580 (2012).
Tiwari, K. & Gupta, R. K. Rare actinomycetes: a potential storehouse for novel antibiotics. Crit. Rev. Biotechnol. 32, 108–132 (2012).
Takeda, U. et al. SF2446, new benzo[a]naphthacene quinone antibiotics. I. Taxonomy and fermentation of the producing strain, isolation and characterization of antibiotics. J. Antibiot. (Tokyo) 41, 417–424 (1988).
Abdelmohsen, U. R. et al. Isolation, phylogenetic analysis and anti-infective activity screening of marine sponge-associated actinomycetes. Mar. Drugs 8, 399–412 (2010).
Wang, Y. et al. Development of a transformation system for Chlamydia trachomatis: restoration of glycogen biosynthesis by acquisition of a plasmid shuttle vector. PLoS Pathog. 7, e1002258 (2011).
Appendix A to the European Convention for the Protection of Vertebrate Animals used for the Protection of Vertebrate Animals used for Experimental and other Scientific Purposes ETS No.123) Guidelines for accommodation and care of animals (Article 5 of the Convention) http://conventions.coe.int/Treaty/EN/Treaties/Html/123-A.htm (accessed 24 April 2015).
Grevelding, C. G. The female-specific W1 sequence of the Puerto Rican strain of Schistosoma mansoni occurs in both genders of a Liberian strain. Mol. Biochem. Parasitol. 71, 269–272 (1995).
Beckmann, S., Leutner, S., Gouignard, N., Dissous, C. & Grevelding, C. G. Protein kinases as potential targets for novel anti-schistosomal strategies. Curr. Pharm. Des 18, 3579–3594 (2012).
Gomi, S., Sasaki, T., Itoh, J. & Sezaki, M. SF2446, new benzo[a]naphthacene quinone antibiotics. II. The structural elucidation. J. Antibiot. (Tokyo) 41, 425–432 (1988).
Acknowledgements
We thank Dr M Grüne for the NMR experiments and C Scheld for technical support (both University of Würzburg). Financial support was provided by Deutsche Forschungsgemeinschaft (SFB 630: ‘Recognition, Preparation, and Functional Analysis of Agents against Infectious Diseases’, projects A2 and A5).
Author Contributions
AR and VK-P contributed to antichlamydial activity testing, manuscript preparation; URA contributed to isolation and structure elucidation of SF2446A2, manuscript preparation; AB and TQ contributed to antischistosomal activity testing, manuscript drafting; TR, CGG and UH contributed to manuscript preparation, analysis of assay results, revising the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on The Journal of Antibiotics website
Supplementary information
Rights and permissions
About this article
Cite this article
Reimer, A., Blohm, A., Quack, T. et al. Inhibitory activities of the marine streptomycete-derived compound SF2446A2 against Chlamydia trachomatis and Schistosoma mansoni. J Antibiot 68, 674–679 (2015). https://doi.org/10.1038/ja.2015.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2015.54
This article is cited by
-
RETRACTED ARTICLE: Rhodozepinone, a new antitrypanosomal azepino-diindole alkaloid from the marine sponge-derived bacterium Rhodococcus sp. UA13
Medicinal Chemistry Research (2017)