Abstract
Background:
Obesity is one of the leading causes of preventable death worldwide. Circadian rhythms are known to control both sleep timing and energy homeostasis, and disruptions in circadian rhythms have been linked with metabolic dysfunction and obesity-associated disease. In previous research, social jetlag, a measure of chronic circadian disruption caused by the discrepancy between our internal versus social clocks, was associated with elevated self-reported body mass index, possibly indicative of a more generalized association with obesity and metabolic dysfunction.
Methods:
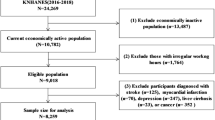
We studied participants from the population-representative Dunedin Longitudinal Study (N=1037) to determine whether social jetlag was associated with clinically assessed measurements of metabolic phenotypes and disease indicators for obesity-related disease, specifically, indicators of inflammation and diabetes.
Results:
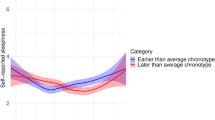
Our analysis was restricted to N=815 non-shift workers in our cohort. Among these participants, we found that social jetlag was associated with numerous clinically assessed measures of metabolic dysfunction and obesity. We distinguished between obese individuals who were metabolically healthy versus unhealthy, and found higher social jetlag levels in metabolically unhealthy obese individuals. Among metabolically unhealthy obese individuals, social jetlag was additionally associated with elevated glycated hemoglobin and an indicator of inflammation.
Conclusions:
The findings are consistent with the possibility that ‘living against our internal clock’ may contribute to metabolic dysfunction and its consequences. Further research aimed at understanding that the physiology and social features of social jetlag may inform obesity prevention and have ramifications for policies and practices that contribute to increased social jetlag, such as work schedules and daylight savings time.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Barness LA, Opitz JM, Gilbert-Barness E . Obesity: genetic, molecular, and environmental aspects. Am J Med Genet 2007; 143A: 3016–3034.
Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB . Annual deaths attributable to obesity in the United States. JAMA 1999; 282: 1530–1538.
Mitchell NS, Catenacci VA, Wyatt HR, Hill JO . Obesity:overview of an epidemic. Psychiatr Clin North Am 2011; 34: 717–732.
Taheri S, Lin L, Austin D, Young T, Mignot E . Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med 2004; 1: e62.
Bjorvatn B, Sagen IM, Øyane N, Waage S, Fetveit A, Pallesen S et al. The association between sleep duration, body mass index and metabolic measures in the Hordaland Health Study. J Sleep Res 2007; 16: 66–76.
Lauderdale DS, Knutson KL, Rathouz PJ, Yan LL, Hulley SB, Liu K . Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index: the CARDIA Sleep Study. Am J Epidemiol 2009; 170: 805–813.
Watson NF, Buchwald D, Vitiello MV, Noonan C, Goldberg J . A twin study of sleep duration and body mass index. J Clin Sleep Med 2010; 6: 11–17.
Nielsen LS, Danielsen KV, Sørensen TI . Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes Rev 2011; 12: 78–92.
Borbély AA . A two process model of sleep regulation. Hum Neurobiol 1982; 1: 195–204.
Marcheva B, Ramsey KM, Buhr ED, Kobayashi Y, Su H, Ko CH et al. Disruption of the clock components CLOCK and BMAL1 leads to hypoinsulinaemia and diabetes. Nature 2010; 466: 627–631.
Bass J, Takahashi JS . Circadian integration of metabolism and energetics. Science 2010; 330: 1349–1354.
Green CB, Takahashi JS, Bass J . The meter of metabolism. Cell 2008; 134: 728–742.
Scheer FAJL Hilton MF, Mantzoros CS, Shea SA . Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc Natl Acad Sci USA 2009; 106: 4453–4458.
Roenneberg T, Allebrandt KV, Merrow M, Vetter C . Social jetlag and obesity. Curr Biol 2012; 22: 939–943.
Reutrakul S, Van Cauter E . Interactions between sleep, circadian function, and glucose metabolism: implications for risk and severity of diabetes. Ann N Y Acad Sci 2014; 1311: 151–173.
Wittmann M, Dinich J, Merrow M, Roenneberg T . Social jetlag: misalignment of biological and social time. Chronobiol Int 2006; 23: 497–509.
Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M et al. Epidemiology of the human circadian clock. Sleep Med Rev 2007; 11: 429–438.
Keith SW, Redden DT, Katzmarzyk PT, Boggiano MM, Hanlon EC, Benca RM et al. Putative contributors to the secular increase in obesity: exploring the roads less traveled. Int J Obes 2006; 30: 1585–1594.
McAllister EJ, Dhurandhar NV, Keith SW, Aronne LJ, Barger J, Baskin M et al. Ten putative contributors to the obesity epidemic. Crit Rev Food Sci Nutr 2009; 49: 868–913.
Visser M, Bouterm LM, McQuillan GM, Wener MH, Harris TB . Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999; 282: 2131–2135.
Kip KE, Marroquin OC, Kelley DE, Johnson BD, Kelsey SF, Shaw LJ et al. Clinical importance of obesity versus the metabolic syndrome in cardiovascular risk in women: a report from the Women's Ischemia Syndrome Evaluation (WISE) study. Circulation 2004; 109: 706–713.
Gregor MF, Hotamisligil GS . Inflammatory mechanisms in obesity. Annu Rev Immunol 2011; 29: 415–445.
Phillips CM, Perry IJ . Does inflammation determine metabolic health status in obese and nonobese adults? J Clin Endocrinol Metab 2013; 98: E1610–E1619.
Blüher M . The distinction of metabolically 'healthy' from 'unhealthy' obese individuals. Curr Opin Lipidol 2010; 21: 38–43.
Hamer M, Stamatakis E . Metabolically healthy obesity and risk of all-cause and cardiovascular disease mortality. J Clin Endocrinol Metab 2012; 97: 2482–2488.
Kramer CK, Zinman B, Retnakaran R . Are metabolically healthy overweight and obesity benign conditions?: a systematic review and meta-analysis. Ann Intern Med 2013; 159: 758–769.
Moffitt TE, Caspi A, Rutter M, Silva PA. (eds) Sex Differences in Antisocial Behavior: Conduct Disorder, Delinquency, and Violence in the Dunedin Longitudinal Study. Cambridge University Press: Cambridge, UK, 2001.
Juda M, Vetter C, Roenneberg T . Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J Biol Rhythms 2013; 28: 141–151.
Roenneberg T, Wirz-Justice A, Merrow M . Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms 2003; 18: 80–90.
Belsky DW, Caspi A, Goldman-Mellor S, Meier MH, Poulton R, Moffitt TE . Is obesity associated with a decline in intelligence quotient during the first half of the life course? Am J Epidemiol 2013; 178: 1461–1468.
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009; 120: 1640–1645.
Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, Criqui M et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 2003; 107: 499–511.
American Diabetes Association. Standards of medical care in diabetes—2012. Diabetes Care. 2012; 35: S11–63.
Grunberg NE . Nicotine as a psychoactive drug: appetite regulation. Psychopharmacol Bull 1986; 22: 875–881.
Jo YH, Talmage DA, Role LW . Nicotinic receptor-mediated effects on appetite and food intake. J Neurobiol 2002; 53: 618–632.
Milne B, Byun U, Lee A. New Zealand Socio-economic Index 2006 (NZSEI-06). An update and revision of the New Zealand Socio-economic Index of Occupational Status 2013. Available from www.stats.govt.nz.
Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL et al. Socioeconomic status and health. The challenge of the gradient. Am Psychol 1994; 49: 15–24.
McLaren L . Socioeconomic status and obesity. Epidemiol Rev 2007; 29: 29–48.
Buxton OM, Cain SW, O'Connor SP, Porter JH, Duffy JF, Wang W et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. Sci Transl Med 2012; 4: 129ra43.
Karatsoreos IN, Bhagat S, Bloss EB, Morrison JH, McEwen BS . Disruption of circadian clocks has ramifications for metabolism, brain, and behavior. Proc Natl Acad Sci USA 2011; 108: 1657–1662.
Barclay JL, Husse J, Bode B, Naujokat N, Meyer-Kovac J, Schmid SM et al. Circadian desynchrony promotes metabolic disruption in a mouse model of shiftwork. PLoS One 2012; 7: e37150.
Feng D, Liu T, Sun Z, Bugge A, Mullican SE, Alenghat T et al. A circadian rhythm orchestrated by histone deacetylase 3 controls hepatic lipid metabolism. Science 2011; 331: 1315–1319.
Xu H, Li H, Woo SL, Kim SM, Shende VR, Neuendorff N et al. Myeloid cell-specific disruption of period1 and period2 exacerbates diet-induced inflammation and insulin resistance. J Biol Chem 2014; 289: 16374–16388.
Archer SN, Laing EE, Möller-Levet CS, van der Veen DR, Bucca G, Lazar AS et al. Mistimed sleep disrupts circadian regulation of the human transcriptome. Proc Natl Acad Sci USA 2014; 111: E682–E691.
Acknowledgements
We would like to acknowledge Dr Celine Vetter for her advice on the Munich Chronotype questionnaire. We thank Phil Silva, Dunedin Study founder, data-collection staff and study members. The work was supported by the followings grants: US National Institute of Aging grant AG032282 and the UK Medical Research Council grant MR/K00381X. The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council. SG-M is supported by a postdoctoral fellowship provided by the National Institute of Child Health and Human Development (T32-HD07376). MJP was supported by a Medical Research Council Core Grant (Nolan).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Supplementary information
Rights and permissions
About this article
Cite this article
Parsons, M., Moffitt, T., Gregory, A. et al. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int J Obes 39, 842–848 (2015). https://doi.org/10.1038/ijo.2014.201
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2014.201
This article is cited by
-
Pressure Building Against the Clock: The Impact of Circadian Misalignment on Blood Pressure
Current Hypertension Reports (2024)
-
Association between night shift work and NAFLD: a prospective analysis of 281,280 UK Biobank participants
BMC Public Health (2023)
-
How can social jetlag affect health?
Nature Reviews Endocrinology (2023)
-
Acute social jetlag augments morning blood pressure surge: a randomized crossover trial
Hypertension Research (2023)
-
The role of insufficient sleep and circadian misalignment in obesity
Nature Reviews Endocrinology (2023)