Abstract
Background:
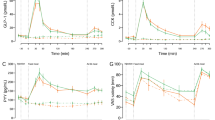
Patients show an elevated postprandial satiety gut hormone release after Roux-en-Y Gastric bypass (gastric bypass). The altered gut hormone response appears to have a prominent role in the reduction of appetite and body weight (BW) after gastric bypass. Patients with insufficient BW loss after gastric bypass have an attenuated postprandial gut hormone response in comparison with patients who lost an adequate amount of BW. The effects of additional gut hormone administration after gastric bypass are unknown.
Methods:
The effects of peripheral administration of peptide YY3-36 (PYY3-36; 300 nmol kg−1), glucagon-like peptide-1 (GLP-1) analogue Exendin-4 (20 nmol kg−1) and somatostatin analogue octreotide (10 μg kg−1) on feeding and BW were evaluated in rats after gastric bypass.
Results:
Gastric bypass rats weighed (P<0.01) and ate less on postoperative day 5 (P<0.001) and thereafter, whereas postprandial plasma PYY and GLP-1 levels were higher compared with sham-operated controls (P<0.001). Administration of both PYY3-36 and Exendin-4 led to a further decrease in food intake in bypass rats compared with saline treatment (P=0.02 and P<0.0001, respectively). Similar reduction in food intake was observed in sham rats (P=0.02 and P<0.001, respectively). Exendin-4 treatment resulted in a significant BW loss in bypass (P=0.03) and sham rats (P=0.04). Subsequent treatment with octreotide led to an increase in food intake in bypass (P=0.007), but not in sham rats (P=0.87).
Conclusion:
Peripheral administration of PYY3-36 and Exendin-4 reduces short-term food intake, whereas octreotide increases short-term food intake in rats after gastric bypass. The endogenous gut hormone response after gastric bypass can thus potentially be further enhanced by additional exogenous therapy with pharmacological doses of gut hormones in patients with insufficient weight loss or weight regain after surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Sjostrom L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007; 357: 741–752.
Ashrafian H, le Roux CW . Metabolic surgery and gut hormones—a review of bariatric entero-humoral modulation. Physiol Behav 2009; 97: 620–631.
Tadross JA, le Roux CW . The mechanisms of weight loss after bariatric surgery. Int J Obes (Lond) 2009; 33 (Suppl 1): S28–S32.
Bueter M, Löwenstein C, Olbers T, Wang M, Cluny NL, Bloom SR et al. Gastric bypass increases energy expenditure in rats. Gastroenterology 2010; 138: 1845–1853.
Orlando FA, Goncalves CG, George ZM, Halverson JD, Cunningham PR, Meguid MM . Neurohormonal pathways regulating food intake and changes after Roux-en-Y gastric bypass. Surg Obes Relat Dis 2005; 1: 486–495.
le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg 2007; 246: 780–785.
le Roux CW, Borg C, Wallis K, Vincent RP, Bueter M, Goodlad R et al. Gut hypertrophy after gastric bypass is associated with increased glucagon-like peptide 2 and intestinal crypt cell proliferation. Ann Surg 2010; 252: 50–56.
le Roux CW, Aylwin SJ, Batterham RL, Borg CM, Coyle F, Prasad V et al. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg 2006; 243: 108–114.
Pittner RA, Moore CX, Bhavsar SP, Gedulin BR, Smith PA, Jodka CM et al. Effects of PYY[3-36] in rodent models of diabetes and obesity. Int J Obes Relat Metab Disord 2004; 28: 963–971.
Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, Dakin CL et al. Gut hormone PYY(3-36) physiologically inhibits food intake. Nature 2002; 418: 650–654.
Talsania T, Anini Y, Siu S, Drucker DJ, Brubaker PL . Peripheral exendin-4 and peptide YY(3-36) synergistically reduce food intake through different mechanisms in mice. Endocrinology 2005; 146: 3748–3756.
Reidelberger RD, Haver AC, Apenteng BA, Anders KL, Steenson SM . Effects of exendin-4 alone and with peptide YY(3-36) on food intake and body weight in diet-induced obese rats. Obesity (Silver Spring) 2011; 19: 121–127.
Steinert RE, Poller B, Castelli MC, Drewe J, Beglinger C . Oral administration of glucagon-like peptide 1 or peptide YY 3-36 affects food intake in healthy male subjects. Am J Clin Nutr 2010; 92: 810–817.
Field BC, Wren AM, Peters V, Baynes KC, Martin NM, Patterson M et al. PYY3-36 and oxyntomodulin can be additive in their effect on food intake in overweight and obese humans. Diabetes 2010; 59: 1635–1639.
Bueter M, Löwenstein C, Ashrafian H, Hillebrand J, Bloom SR, Olbers T et al. Vagal sparing surgical technique but not stoma size affects body weight loss in rodent model of gastric bypass. Obes Surg 2010; 20: 616–622.
Batterham RL, Cohen MA, Ellis SM, le Roux CW, Withers DJ, Frost GS et al. Inhibition of food intake in obese subjects by peptide YY3-36. N Engl J Med 2003; 349: 941–948.
Savage AP, Adrian TE, Carolan G, Chatterjee VK, Bloom SR . Effects of peptide YY (PYY) on mouth to caecum intestinal transit time and on the rate of gastric emptying in healthy volunteers. Gut 1987; 28: 166–170.
Kreymann B, Williams G, Ghatei MA, Bloom SR . Glucagon-like peptide-1 7-36: a physiological incretin in man. Lancet 1987; 2: 1300–1304.
Adrian TE, Bloom SR, Bryant MG, Polak JM, Heitz P . Proceedings: radioimmunoassay of a new gut hormone-human pancreatic polypeptide. Gut 1976; 17: 393–394.
Chelikani PK, Haver AC, Reidelberger RD . Intermittent intraperitoneal infusion of peptide YY(3-36) reduces daily food intake and adiposity in obese rats. Am J Physiol Regul Integr Comp Physiol 2007; 293: R39–R46.
Reidelberger RD, Haver AC, Apenteng BA, Anders KL, Steenson SM . Effects of Exendin-4 alone and with peptide YY(3-36) on food intake and body weight in diet-induced obese rats. Obesity (Silver Spring) 2011; 19: 121–127.
Vrang N, Madsen AN, Tang-Christensen M, Hansen G, Larsen PJ . PYY(3-36) reduces food intake and body weight and improves insulin sensitivity in rodent models of diet-induced obesity. Am J Physiol Regul Integr Comp Physiol 2006; 291: R367–R375.
Koegler FH, Enriori PJ, Billes SK, Takahashi DL, Martin MS, Clark RL et al. Peptide YY(3-36) inhibits morning, but not evening, food intake and decreases body weight in rhesus macaques. Diabetes 2005; 54: 3198–3204.
Mack CM, Moore CX, Jodka CM, Bhavsar S, Wilson JK, Hoyt JA et al. Antiobesity action of peripheral exenatide (exendin-4) in rodents: effects on food intake, body weight, metabolic status and side-effect measures. Int J Obes (Lond) 2006; 30: 1332–1340.
Kwak HH, Shim WS, Hwang S, Son MK, Kim YJ, Kim TH et al. Pharmacokinetics and efficacy of a biweekly dosage formulation of exenatide in Zucker diabetic fatty (ZDF) rats. Pharm Res 2009; 26: 2504–2512.
Heine RJ, Van Gaal LF, Johns D, Mihm MJ, Widel MH, Brodows RG et al. Exenatide versus insulin glargine in patients with suboptimally controlled type 2 diabetes: a randomized trial. Ann Intern Med 2005; 143: 559–569.
Nauck MA, Duran S, Kim D, Johns D, Northrup J, Festa A et al. A comparison of twice-daily exenatide and biphasic insulin aspart in patients with type 2 diabetes who were suboptimally controlled with sulfonylurea and metformin: a non-inferiority study. Diabetologia 2007; 50: 259–267.
Magro DO, Geloneze B, Delfini R, Pareja BC, Callejas F, Pareja JC . Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg 2008; 18: 648–651.
Christou NV, Look D, Maclean LD . Weight gain after short- and long-limb gastric bypass in patients followed for longer than 10 years. Ann Surg 2006; 244: 734–740.
Gumbs AA, Pomp A, Gagner M . Revisional bariatric surgery for inadequate weight loss. Obes Surg 2007; 17: 1137–1145.
Buchwald H, Estok R, Fahrbach K, Banel D, Sledge I . Trends in mortality in bariatric surgery: a systematic review and meta-analysis. Surgery 2007; 142: 621–632; discussion 632–635.
Astrup A, Rössner S, Van Gaal L, Rissanen A, Niskanen L, Al Hakim M et al. Effects of liraglutide in the treatment of obesity: a randomised, double-blind, placebo-controlled study. Lancet 2009; 374: 1606–1616.
Kolterman OG, Kim DD, Shen L, Ruggles JA, Nielsen LL, Fineman MS et al. Pharmacokinetics, pharmacodynamics, and safety of exenatide in patients with type 2 diabetes mellitus. Am J Health Syst Pharm 2005; 62: 173–181.
Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV et al. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med 2005; 353: 249–254.
Alvarez GC, Faria EN, Beck M, Girardon DT, Machado AC . Laparoscopic spleen-preserving distal pancreatectomy as treatment for nesidioblastosis after gastric bypass surgery. Obes Surg 2007; 17: 550–552.
Clancy TE, Moore Jr FD, Zinner MJ . Post-gastric bypass hyperinsulinism with nesidioblastosis: subtotal or total pancreatectomy may be needed to prevent recurrent hypoglycemia. J Gastrointest Surg 2006; 10: 1116–1119.
Parkinson C, Drake WM, Roberts ME, Meeran K, Besser GM, Trainer PJ . A comparison of the effects of pegvisomant and octreotide on glucose, insulin, gastrin, cholecystokinin, and pancreatic polypeptide responses to oral glucose and a standard mixed meal. J Clin Endocrinol Metab 2002; 87: 1797–1804.
Rudholm T, Wallin B, Theodorsson E, Näslund E, Hellström PM . Release of regulatory gut peptides somatostatin, neurotensin and vasoactive intestinal peptide by acid and hyperosmolal solutions in the intestine in conscious rats. Regul Pept 2009; 152: 8–12.
Neary NM, Small CJ, Druce MR, Park AJ, Ellis SM, Semjonous NM et al. Peptide YY3-36 and glucagon-like peptide-17-36 inhibit food intake additively. Endocrinology 2005; 146: 5120–5127.
Proulx K, Cota D, Castañeda TR, Tschöp MH, D'Alessio DA, Tso P et al. Mechanisms of oleoylethanolamide-induced changes in feeding behavior and motor activity. Am J Physiol Regul Integr Comp Physiol 2005; 289: R729–R737.
Seeley RJ, Blake K, Rushing PA, Benoit S, Eng J, Woods SC et al. The role of CNS glucagon-like peptide-1 (7−36) amide receptors in mediating the visceral illness effects of lithium chloride. J Neurosci 2000; 20: 1616–1621.
Acknowledgements
WKF and MB were supported by the German Research Society (DFG), CleR by a Department of Health clinician scientist award, and ADM was supported by the Medical Research Council. Imperial College London receives support from the National Institute for Health Research Biomedical Research Centre funding scheme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fenske, W., Bueter, M., Miras, A. et al. Exogenous peptide YY3-36 and Exendin-4 further decrease food intake, whereas octreotide increases food intake in rats after Roux-en-Y gastric bypass. Int J Obes 36, 379–384 (2012). https://doi.org/10.1038/ijo.2011.126
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2011.126
Keywords
This article is cited by
-
Primary weight loss failure after Roux-en-Y gastric bypass is characterized by impaired gut-hormone mediated regulation of food intake
International Journal of Obesity (2023)
-
Chimeric peptide EP45 as a dual agonist at GLP-1 and NPY2R receptors
Scientific Reports (2018)
-
Changes in Reward after Gastric Bypass: the Advantages and Disadvantages
Current Atherosclerosis Reports (2015)