Abstract
Objective:
To compare the efficacy of a phone vs a traditional face-to-face clinic approach to achieve 10% weight loss and weight maintenance.
Design:
Twenty-six week, randomized, controlled trial.
Subjects:
Twenty-four men and 72 women, ages 25–68 years, with a body mass index (BMI) of 33.2±3.8.
Measurements:
Weight loss at 12 weeks and weight maintenance at 26 weeks were the primary outcomes. Attendance, meal replacements (MRs), fruits/vegetables (F/V), and physical activity (PA) were measured weekly for process evaluation.
Results:
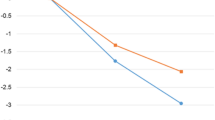
Median weight loss (range) from baseline at 12 weeks was significantly different for phone at 10.6 kg (16.6) or 10.4% and clinic at 12.7 kg (19.9) or 13.7%, and both were significantly different when compared with the control group with a weight loss of 0.25 kg (5.6) or 0.24%. Median weight loss at 26 weeks was 12.8 kg (23.4) or 13.0% from baseline for the phone group and 12.5 kg (35.2) or 12.6% from baseline for the clinic group (P>0.05).
Conclusion:
The median weight loss for both phone and clinic groups at 12 and 26 weeks exceeded the NHLBI guideline of 10% weight loss from baseline. The phone approach may be a viable option to the traditional weight management clinic for both service providers and participants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM . Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 2004; 291: 2847–2850.
National Heart, Lung, and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults; the Evidence Report. US Department of Health and Human Services, National Institutes of Health, 1998, pp 1–228.
Thompson D, Wolf A . The medical-care cost burden of obesity. Obes Rev 2001; 2: 189–197.
Sullivan PW, Morrato EH, Ghushchyan V, Wyatt HR, Hill JO . Obesity, inactivity, and the prevalence of diabetes and diabetes-related cardiovascular comorbidities in the US, 2000–2002. Diabetes Care 2005; 28: 1599–1603.
Katz DL . Competing dietary claims for weight loss: finding the forest through truculent trees. Annu Rev Public Health 2005; 26: 61–88.
Jeffery RW, Epstein L, Wilson G, Drewnowski A, Stunkard AJ, Wing R . Long-term maintenance of weight loss: current status. Health Psychol 2000; 19: 5–16.
Jerant AF, von Friederichs-Fitzwater MM, Moore M . Patients' perceived barriers to active self-management of chronic conditions. Patient Educ Couns 2005; 57: 300–307.
French SA, Neumark-Sztainer D, Story M, Jeffery RW . Reducing barriers to participation in weight-loss programs in low-income women. J Am Diet Assoc 1998; 98: 198–200.
Wadden TA, Crerand CE, Brock J . Behavioral treatment of obesity. Psychiatr Clin North Am 2005; 28: 151–170, ix.
Weinstein PK . A review of weight loss programs delivered via the internet. J Cardiovasc Nurs 2006; 21: 251–258 ; quiz 259–260.
Sherwood NE, Jeffery RW, Pronk NP, Boucher JL, Hanson A, Boyle R et al. Mail and phone interventions for weight loss in a managed-care setting: weigh-to-be 2-year outcomes. Int J Obes (Lond) 2006; 30: 1565–1573.
Marcus BH, Owen N, Forsyth LH, Cavill NA, Fridinger F . Physical activity interventions using mass media, print media, and information technology. Am J Prev Med 1998; 15: 362–378.
Tate DF, Jackvony EH, Wing RR . A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an internet weight loss program. Arch Intern Med 2006; 166: 1620–1625.
US Census Bureau. Computer and Internet Use in the United States: 2003 Current Population Survey (CPS) Reports. http://www.census.gov/prod/2005pubs/p23-208.pdf.2005.
Federal Communication Commission. Trends in Telephone Service. http://www.fcc.gov/Bureaus/Common_Carrier/Reports/FCC-State_Link/IAD/trend605.pdf.2005.
Castro CM, King AC, Brassington GS . Telephone versus mail interventions for maintenance of physical activity in older adults. Health Psychol 2001; 20: 438–444.
VanWormer JJ, Boucher JL, Pronk NP, Thoennes JJ . Lifestyle behavior change and coronary artery disease: effectiveness of a telephone-based counseling program. J Nutr Educ Behav 2004; 36: 333–334.
Jeffery RW, Sherwood NE, Brelje K, Pronk NP, Boyle R, Boucher JL et al. Mail and phone interventions for weight loss in a managed-care setting: weigh-to-be one-year outcomes. Int J Obes Relat Metab Disord 2003; 27: 1584–1592.
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 2000; 32: S498–S504.
The DCCT Research Group. Reliability and validity of a diabetes quality of life measure for the diabetes control and complications trial (DCCT). Diabetes Care 1988; 11: 725–732.
Jeffery RW, Wing RR, Sherwood NE, Tate DF . Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr 2003; 78: 684–689.
Kassirer J, Angell M . Losing weight – an ill-fated new year's resolution. N Engl J Med 1998; 338: 52–54.
Stern JO, Hirsch J, Blair SN, Foreyt JP, Frank A, Kumanyika SK et al. Weighing the options: criteria for evaluating weight-management programs. Obes Res 1995; 3: 591–604.
Keogh JB, Clifton PM . The role of meal replacements in obesity treatment. Obes Rev 2005; 6: 229–234.
Acknowledgements
This work was supported in part by Health Management Resources, Boston, MA.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Donnelly, J., Smith, B., Dunn, L. et al. Comparison of a phone vs clinic approach to achieve 10% weight loss. Int J Obes 31, 1270–1276 (2007). https://doi.org/10.1038/sj.ijo.0803568
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803568
Keywords
This article is cited by
-
Participant perspectives of a telehealth trial investigating the use of telephone and text message support in obesity management: a qualitative evaluation
BMC Health Services Research (2021)
-
Adding Telephone and Text Support to an Obesity Management Program Improves Behavioral Adherence and Clinical Outcomes. A Randomized Controlled Crossover Trial
International Journal of Behavioral Medicine (2019)
-
Telecoaching plus a portion control plate for weight care management: a randomized trial
Trials (2015)
-
Healthy eating and lifestyle in pregnancy (HELP): a protocol for a cluster randomised trial to evaluate the effectiveness of a weight management intervention in pregnancy
BMC Public Health (2014)
-
Lifestyle Interventions for Cardiovascular Disease Risk Reduction: A Systematic Review of the Effects of Diet Composition, Food Provision, and Treatment Modality on Weight Loss
Current Atherosclerosis Reports (2014)