Abstract
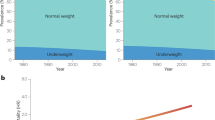
Obesity has now reached epidemic proportions. Epidemiological studies in the past decades have shown that adults gain weight and adiposity from the early twenties until their sixties. In the paediatric population, growing numbers of children and adolescents put on unhealthy weight. Many environmental, socio-economical and biological determinants that predispose to weight gain have been identified thus far. The aim of the present review is to summarize the current knowledge on the role of the circulating levels of adipokines and other entero-insular hormones and biological markers of obesity to predict weight gain in humans. The review focuses on relationship between hormonal and biochemical markers (insulin, insulin-like growth factors, gastrointestinal hormones, leptin, adiponectin, resistin, inflammatory proteins and cytokines) and weight gain in prospective studies. The complex relationships displayed by these hormonal factors with future weight gain in humans are critically reviewed and integrative models are proposed. Overall, most of the studies reported to date made adjustments for baseline body mass index but failed to consider dietary intake and physical activity as confounding factors. Outstanding questions are raised and new directions for future prospective studies are proposed in order to improve our understanding of the role of biological determinants of energy balance and development of obesity in humans.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Parsons TJ, Power C, Logan S, Summerbell CD . Childhood predictors of adult obesity: a systematic review. Int J Obes Relat Metab Disord 1999; 23 (Suppl 8): S1–S107.
Perusse L, Rankinen T, Zuberi A, Chagnon YC, Weisnagel SJ, Argyropoulos G et al. The human obesity gene map: the 2004 update. Obes Res 2005; 13: 381–490.
Lau DC, Dhillon B, Yan H, Szmitko PE, Verma S . Adipokines: molecular links between obesity and atheroslcerosis. Am J Physiol Heart Circ Physiol 2005; 288: H2031–H2041.
Ferrannini E, Camastra S . Relationship between impaired glucose tolerance, non-insulin-dependent diabetes mellitus and obesity. Eur J Clin Invest 1998; 28 (Suppl 2): 3–6.
Folsom AR, Jacobs Jr DR, Wagenknecht LE, Winkhart SP, Yunis C, Hilner JE et al. Increase in fasting insulin and glucose over seven years with increasing weight and inactivity of young adults. The CARDIA Study. Coronary artery risk development in young adults. Am J Epidemiol 1996; 144: 235–246.
Sinaiko AR, Donahue RP, Jacobs Jr DR, Prineas RJ . Relation of weight and rate of increase in weight during childhood and adolescence to body size, blood pressure, fasting insulin, and lipids in young adults. The Minneapolis Children's Blood Pressure Study. Circulation 1999; 99: 1471–1476.
Wynne K, Stanley S, McGowan B, Bloom S . Appetite control. J Endocrinol 2005; 184: 291–318.
Sandhu MS, Gibson JM, Heald AH, Dunger DB, Wareham NJ . Low circulating IGF-II concentrations predict weight gain and obesity in humans. Diabetes 2003; 52: 1403–1408.
Gould AJ, Williams DE, Byrne CD, Hales CN, Wareham NJ . Prospective cohort study of the relationship of markers of insulin resistance and secretion with weight gain and changes in regional adiposity. Int J Obes Relat Metab Disord 1999; 23: 1256–1261.
Zavaroni I, Zuccarelli A, Gasparini P, Massironi P, Barilli A, Reaven GM . Can weight gain in healthy, nonobese volunteers be predicted by differences in baseline plasma insulin concentration? J Clin Endocrinol Metab 1998; 83: 3498–3500.
Lakka HM, Salonen JT, Tuomilehto J, Kaplan GA, Lakka TA . Obesity and weight gain are associated with increased incidence of hyperinsulinemia in non-diabetic men. Horm Metab Res 2002; 34: 492–498.
Masuo K, Kawaguchi H, Mikami H, Ogihara T, Tuck ML . Serum uric acid and plasma norepinephrine concentrations predict subsequent weight gain and blood pressure elevation. Hypertension 2003; 42: 474–480.
Folsom AR, Vitelli LL, Lewis CE, Schreiner PJ, Watson RL, Wagenknecht LE . Is fasting insulin concentration inversely associated with rate of weight gain? Contrasting findings from the CARDIA and ARIC study cohorts. Int J Obes Relat Metab Disord 1998; 22: 48–54.
Hoag S, Marshall JA, Jones RH, Hamman RF . High fasting insulin levels associated with lower rates of weight gain in persons with normal glucose tolerance: the San Luis Valley Diabetes Study. Int J Obes Relat Metab Disord 1995; 19: 175–180.
Valdez R, Mitchell BD, Haffner SM, Hazuda HP, Morales PA, Monterrosa A et al. Predictors of weight change in a bi-ethnic population. The San Antonio Heart Study. Int J Obes Relat Metab Disord 1994; 18: 85–91.
Swinburn BA, Nyomba BL, Saad MF, Zurlo F, Raz I, Knowler WC et al. Insulin resistance associated with lower rates of weight gain in Pima Indians. J Clin Invest 1991; 88: 168–173.
Schwartz MW, Boyko EJ, Kahn SE, Ravussin E, Bogardus C . Reduced insulin secretion: an independent predictor of body weight gain. J Clin Endocrinol Metab 1995; 80: 1571–1576.
Hodge AM, Dowse GK, Alberti KG, Tuomilehto J, Gareeboo H, Zimmet PZ . Relationship of insulin resistance to weight gain in nondiabetic Asian Indian, Creole, and Chinese Mauritians. Mauritius Non-communicable Disease Study Group. Metabolism 1996; 45: 627–633.
Boyko EJ, Leonetti DL, Bergstrom RW, Newell-Morris L, Fujimoto WY . Low insulin secretion and high fasting insulin and C-peptide levels predict increased visceral adiposity. 5-year follow-up among initially nondiabetic Japanese-American men. Diabetes 1996; 45: 1010–1015.
Sigal RJ, El Hashimy M, Martin BC, Soeldner JS, Krolewski AS, Warram JH . Acute postchallenge hyperinsulinemia predicts weight gain: a prospective study. Diabetes 1997; 46: 1025–1029.
Johnson MS, Figueroa-Colon R, Huang TT, Dwyer JH, Goran MI . Longitudinal changes in body fat in African American and Caucasian children: influence of fasting insulin and insulin sensitivity. J Clin Endocrinol Metab 2001; 86: 3182–3187.
Odeleye OE, de Court, Pettitt DJ, Ravussin E . Fasting hyperinsulinemia is a predictor of increased body weight gain and obesity in Pima Indian children. Diabetes 1997; 46: 1341–1345.
Savoye M, Dziura J, Castle J, DiPietro L, Tamborlane WV, Caprio S . Importance of plasma leptin in predicting future weight gain in obese children: a two-and-a-half-year longitudinal study. Int J Obes Relat Metab Disord 2002; 26: 942–946.
Salbe AD, Weyer C, Lindsay RS, Ravussin E, Tataranni PA . Assessing risk factors for obesity between childhood and adolescence: I. Birth weight, childhood adiposity, parental obesity, insulin, and leptin. Pediatrics 2002; 110 (2 Part 1): 299–306.
Maffeis C, Moghetti P, Grezzani A, Clementi M, Gaudino R, Tato L . Insulin resistance and the persistence of obesity from childhood into adulthood. J Clin Endocrinol Metab 2002; 87: 71–76.
Srinivasan SR, Myers L, Berenson GS . Temporal association between obesity and hyperinsulinemia in children, adolescents, and young adults: the Bogalusa Heart Study. Metabolism 1999; 48: 928–934.
Byrnes SE, Baur LA, Bermingham M, Brock K, Steinbeck K . Leptin and total cholesterol are predictors of weight gain in pre-pubertal children. Int J Obes Relat Metab Disord 1999; 23: 146–150.
Lazarus R, Sparrow D, Weiss S . Temporal relations between obesity and insulin: longitudinal data from the Normative Aging Study. Am J Epidemiol 1998; 147: 173–179.
O'Dell SD, Day IN . Insulin-like growth factor II (IGF-II). Int J Biochem Cell Biol 1998; 30: 767–771.
Ong K, Kratzsch J, Kiess W, Dunger D, ALSPAC Study Team. Circulating IGF-I levels in childhood are related to both current body composition and early postnatal growth rate. J Clin Endocrinol Metab 2002; 87: 1041–1044.
Chang S, Wu X, Yu H, Spitz MR . Plasma concentrations of insulin-like growth factors among healthy adult men and postmenopausal women: associations with body composition, lifestyle, and reproductive factors. Cancer Epidemiol Biomarkers Prevent 2002; 11: 758–766.
Wynne K, Stanley S, Bloom S . The gut and regulation of body weight. J Clin Endocrinol Metab 2004; 89: 2576–2582.
Wu JT, Kral JG . Ghrelin: integrative neuroendocrine peptide in health and disease. Ann Surg 2004; 239: 464–474.
Bunt JC, Salbe AD, Tschop MH, DelParigi A, Daychild P, Tataranni PA . Cross-sectional and prospective relationships of fasting plasma ghrelin concentrations with anthropometric measures in pima Indian children. J Clin Endocrinol Metab 2003; 88: 3756–3761.
Small CJ, Bloom SR . Gut hormones as peripheral anti obesity targets. Curr Drug Targets CNS Neurol Disord 2004; 3: 379–388.
Naslund E, King N, Mansten S, Adner N, Holst JJ, Gutniak M et al. Prandial subcutaneous injections of glucagon-like peptide-1 cause weight loss in obese human subjects. Br J Nutr 2004; 91: 439–446.
Cohen MA, Ellis SM, Le Roux CW, Batterham RL, Park A, Patterson M et al. Oxyntomodulin suppresses appetite and reduces food intake in humans. J Clin Endocrinol Metab 2003; 88: 4696–4701.
Dirlewanger M, di VV, Guenat E, Battilana P, Seematter G, Schneiter P et al. Effects of short-term carbohydrate or fat overfeeding on energy expenditure and plasma leptin concentrations in healthy female subjects. Int J Obes Relat Metab Disord 2000; 24: 1413–1418.
Haffner SM, Mykkanen LA, Gonzalez CC, Stern MP . Leptin concentrations do not predict weight gain: the Mexico City Diabetes Study. Int J Obes Relat Metab Disord 1998; 22: 695–699.
Hodge AM, de Court, Dowse GK, Zimmet PZ, Collier GR, Gareeboo H et al. Do leptin levels predict weight gain? – A 5-year follow-up study in Mauritius. Mauritius Non-communicable Disease Study Group. Obes Res 1998; 6: 319–325.
Folsom AR, Jensen MD, Jacobs Jr DR, Hilner JE, Tsai AW, Schreiner PJ . Serum leptin and weight gain over 8 years in African American and Caucasian young adults. Obes Res 1999; 7: 1–8.
Lissner L, Karlsson C, Lindroos AK, Sjostrom L, Carlsson B, Carlsson L et al. Birth weight, adulthood BMI, and subsequent weight gain in relation to leptin levels in Swedish women. Obes Res 1999; 7: 150–154.
van Rossum CT, Hoebee B, van Baak MA, Mars M, Saris WH, Seidell JC . Genetic variation in the leptin receptor gene, leptin, and weight gain in young Dutch adults. [see comment]. Obes Res 2003; 11: 377–386.
Chu NF, Spiegelman D, Yu J, Rifai N, Hotamisligil GS, Rimm EB . Plasma leptin concentrations and four-year weight gain among US men. Int J Obes Relat Metab Disord 2001; 25: 346–353.
Chessler SD, Fujimoto WY, Shofer JB, Boyko EJ, Weigle DS . Increased plasma leptin levels are associated with fat accumulation in Japanese Americans. Diabetes 1998; 47: 239–243.
Nishida C, Uauy R, Kumanyika S, Shetty P . The joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: process, product and policy implications. Public Health Nutr 2004; 7 (1A): 245–250.
Ravussin E, Pratley RE, Maffei M, Wang H, Friedman JM, Bennett PH et al. Relatively low plasma leptin concentrations precede weight gain in Pima Indians. Nat Med 1997; 3: 238–240.
Lindroos AK, Lissner L, Carlsson B, Carlsson LM, Torgerson J, Karlsson C et al. Familial predisposition for obesity may modify the predictive value of serum leptin concentrations for long-term weight change in obese women. Am J Clin Nutr 1998; 67: 1119–1123.
Shalitin S, Phillip M . Role of obesity and leptin in the pubertal process and pubertal growth--a review. Int J Obes Relat Metab Disord 2003; 27: 869–874.
Johnson MS, Huang TT, Figueroa-Colon R, Dwyer JH, Goran MI . Influence of leptin on changes in body fat during growth in African American and white children. Obes Res 2001; 9: 593–598.
Ahmed ML, Ong KK, Morrell DJ, Cox L, Drayer N, Perry L et al. Longitudinal study of leptin concentrations during puberty: sex differences and relationship to changes in body composition. J Clin Endocrinol Metab 1999; 84: 899–905.
Mars M, de Graaf C, de Groot LC, Kok FJ . Decreases in fasting leptin and insulin concentrations after acute energy restriction and subsequent compensation in food intake. Am J Clin Nutr 2005; 81: 570–577.
Keller P, Keller C, Steensberg A, Robinson LE, Pedersen BK . Leptin gene expression and systemic levels in healthy men: effect of exercise, carbohydrate, interleukin-6, and epinephrine. J Appl Physiol 2005; 98: 1805–1812.
Gavrila A, Chan JL, Yiannakouris N, Kontogianni M, Miller LC, Orlova C et al. Serum adiponectin levels are inversely associated with overall and central fat distribution but are not directly regulated by acute fasting or leptin administration in humans: cross-sectional and interventional studies. J Clin Endocrinol Metab 2003; 88: 4823–4831.
Steffes MW, Gross MD, Schreiner PJ, Yu X, Hilner JE, Gingerich R et al. Serum adiponectin in young adults--interactions with central adiposity, circulating levels of glucose, and insulin resistance: the CARDIA study. Ann Epidemiol 2004; 14: 492–498.
Goldstein BJ, Scalia R . Adiponectin: a novel adipokine linking adipocytes and vascular function. J Clin Endocrinol Metab 2004; 89: 2563–2568.
Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE et al. Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 2001; 86: 1930–1935.
Vozarova B, Stefan N, Lindsay RS, Krakoff J, Knowler WC, Funahashi T et al. Low plasma adiponectin concentrations do not predict weight gain in humans. Diabetes 2002; 51: 2964–2967.
Fantuzzi G . Adipose tissue, adipokines, and inflammation. J Allergy Clin Immunol 2005; 115: 911–919.
Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM et al. The hormone resistin links obesity to diabetes. Nature 2001; 409: 307–312.
Kershaw EE, Flier JS . Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 2004; 89: 2548–2556.
Azuma K, Katsukawa F, Oguchi S, Murata M, Yamazaki H, Shimada A et al. Correlation between serum resistin level and adiposity in obese individuals. Obes Res 2003; 11: 997–1001.
Bajaj M, Suraamornkul S, Hardies LJ, Pratipanawatr T, DeFronzo RA . Plasma resistin concentration, hepatic fat content, and hepatic and peripheral insulin resistance in pioglitazone-treated type II diabetic patients. Int J Obes Relat Metab Disord 2004; 28: 783–789.
Vozarova de Court, Degawa-Yamauchi M, Considine RV, Tataranni PA . High serum resistin is associated with an increase in adiposity but not a worsening of insulin resistance in Pima Indians. Diabetes 2004; 53: 1279–1284.
Faraj M, Lu HL, Cianflone K . Diabetes, lipids, and adipocyte secretagogues. Biochem Cell Biol 2004; 82: 170–190.
Pomeroy C, Mitchell J, Eckert E, Raymond N, Crosby R, Dalmasso AP . Effect of body weight and caloric restriction on serum complement proteins, including factor D/adipsin: studies in anorexia nervosa and obesity. Clin Exper Immunol 1997; 108: 507–515.
Gabrielsson BG, Johansson JM, Lonn M, Jernas M, Olbers T, Peltonen M et al. High expression of complement components in omental adipose tissue in obese men. Obes Res 2003; 11: 699–708.
Hube F, Hauner H . The role of TNF-alpha in human adipose tissue: prevention of weight gain at the expense of insulin resistance? Horm Metab Res 1999; 31: 626–631.
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V . Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? Atherosclerosis 2000; 148: 209–214.
Vozarova B, Weyer C, Hanson K, Tataranni PA, Bogardus C, Pratley RE . Circulating interleukin-6 in relation to adiposity, insulin action, and insulin secretion. Obes Res 2001; 9: 414–417.
Fernandez-Real JM, Broch M, Vendrell J, Ricart W . Insulin resistance, inflammation, and serum fatty acid composition. Diabetes Care 2003; 26: 1362–1368.
Stenlof K, Wernstedt I, Fjallman T, Wallenius V, Wallenius K, Jansson JO . Interleukin-6 levels in the central nervous system are negatively correlated with fat mass in overweight/obese subjects. J Clin Endocrinol Metab 2003; 88: 4379–4383.
Gomez-Ambrosi J, Salvador J, Paramo JA, Orbe J, de Irala J, Diez-Caballero A et al. Involvement of leptin in the association between percentage of body fat and cardiovascular risk factors. Clin Biochem 2002; 35: 315–320.
Duncan BB, Schmidt MI, Chambless LE, Folsom AR, Carpenter M, Heiss G . Fibrinogen, other putative markers of inflammation, and weight gain in middle-aged adults--the ARIC study. Atherosclerosis risk in communities. Obes Res 2000; 8: 279–286.
Engstrom G, Stavenow L, Hedblad B, Lind P, Eriksson KF, Janzon L et al. Inflammation-sensitive plasma proteins, diabetes, and mortality and incidence of myocardial infarction and stroke: a population-based study. Diabetes 2003; 52: 442–447.
Byrne CD . Triglyceride-rich lipoproteins: are links with atherosclerosis mediated by a procoagulant and proinflammatory phenotype? Atherosclerosis 1999; 145: 1–15.
Aljada A, Mohanty P, Ghanim H, Abdo T, Tripathy D, Chaudhuri A et al. Increase in intranuclear nuclear factor kappaB and decrease in inhibitor kappaB in mononuclear cells after a mixed meal: evidence for a proinflammatory effect. Am J Clin Nutr 2004; 79: 682–690.
Acknowledgements
MFH is a post-doctoral fellow supported by the Merck-Frosst-Scherring-Université de Sherbrooke Fellowship Award. ACC is the recipient of a New Investigator Scholarship Award from the Canadian Institutes of Health Research (MSH 46799). MFL is the recipient of a Junior-2 clinician-researcher scholarship from the Fonds de la recherche en santé du Québec.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hivert, MF., Langlois, MF. & Carpentier, A. The entero-insular axis and adipose tissue-related factors in the prediction of weight gain in humans. Int J Obes 31, 731–742 (2007). https://doi.org/10.1038/sj.ijo.0803500
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803500
Keywords
This article is cited by
-
Leptin production capacity determines food intake and susceptibility to obesity-induced diabetes in Oikawa–Nagao Diabetes-Prone and Diabetes-Resistant mice
Diabetologia (2020)
-
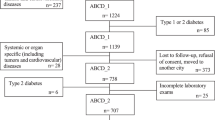
Prospective Investigation of Metabolic Characteristics in Relation to Weight Gain in Older Adults: The Hoorn Study
Obesity (2009)