Abstract
The link between environmental chemicals and human health has emerged, but has not been completely examined in terms of its risk factors. Therefore, we aimed to study the relationships of different sets of urinary environmental chemical concentrations and high blood pressure (BP) in a national, population-based study. Data were retrieved from the United States National Health and Nutrition Examination Surveys, 2009–2012, including demographics, BP readings and urinary environmental chemical concentrations. Analyses included χ2-test, t-test, survey-weighted logistic regression models and population attributable risk estimation. Urinary cesium (odds ratio (OR) 1.52, 95% confidence interval (CI) 1.06–2.18, P=0.026), molybdenum (OR 1.45, 95% CI 1.04–2.02, P=0.029), lead (OR 1.49, 95% CI 1.12–1.98, P=0.009), platinum (OR 1.66, 95% CI 1.14–2.21, P=0.002), antimony (OR 1.44, 95% CI 1.12–1.86, P=0.008) and tungsten (OR 1.48, 95% CI 1.22–1.79, P<0.001) concentrations were observed to be associated with high BP. Similar results were observed for mono-2-ethyl-5-carboxypentyl (OR 1.29, 95% CI 1.04–1.59, P=0.024), mono-n-butyl (OR 1.36, 95% CI 1.11–1.67, P=0.005), mono-2-ethyl-5-hydroxyhexyl (OR 1.21, 95% CI 1.01–1.46, P=0.041), mono-n-methyl (OR 1.24, 95% CI 1.01–1.46, P=0.014), mono-2-ethyl-5-oxohexyl (OR 1.21, 95% CI 1.01–1.45, P=0.036), mono-benzyl (OR 1.41, 95% CI 1.15–1.74, P=0.002), dimethylarsonic acid (OR 1.38, 95% CI 1.08–1.76, P=0.012) and trimethylarsine oxide (OR 2.56, 95% CI 1.29–5.07, P=0.010) concentrations. Each chemical could account for 3–19% of the population attributable risk for high BP. A small sex difference was found. However, there are no associations between environmental parabens and pesticides and high BP. Urinary heavy metal, phthalate and arsenic concentrations were associated with high BP, although a causal effect cannot be established. Elimination of environmental chemical exposure in humans still needs to be pursued.
Similar content being viewed by others
Introduction
The burden of high blood pressure (BP) has remained high in the United States, affecting approximately one-third of American adults in the current century.1 The economic costs associated with hypertension are high for individuals and society. Exposure to environmental chemicals may induce atherosclerosis by increasing oxidative stress or produce reactive oxygen species, such as superoxide ion, hydrogen peroxide and hydroxyl radicals, according to experimental research.2, 3 Previous epidemiological investigations focused on arterial disease, heart disease and cardiovascular disease as end points,4, 5, 6 but the relationship with BP, a strong risk factor for many human chronic diseases as mentioned above, is unclear. Previously, an adverse intrauterine environment was found to be associated with an increased risk for future cardiovascular disease and hypertension. Recent animal models have shown that an elevated BP in offspring could be induced by maternal exposure to toxins.7 In this context, we aimed to examine the relationships of different sets of urine environmental chemical concentrations and high BP in a national, population-based setting.
Methods
Study sample
As described elsewhere,8 the United States National Health and Nutrition Examination Surveys (NHANES) has been a national, population-based, multi-year, cross-sectional study. The study sample is representative of the civilian, non-institutionalized US population. Information on demographics, lifestyle factors and self-reported medical conditions was obtained by household interview using questionnaires. In the current analysis, the 2009–2012 cohorts, the two most recent cohorts, were selected and combined. Informed consent was obtained from participating subjects. BP was measured on all examinees 8 years and older at the household interview and three times (details via: http://www.cdc.gov/nchs/nhanes/nhanes2009-2010/BPX_F.htm). The standard measuring protocol can be found in: http://www.cdc.gov/nchs/nhanes/nhanes20092010/BPX_F.htm#Protocol_and_Procedure. Participants with any of the following on both arms were excluded from the exam according to the standard protocol: rashes, gauze dressings, casts, edema, paralysis, tubes, open sores or wounds, withered arms, a–v shunts and radical mastectomy or if the BP cuff does not fit on the arm. The measurements were taken three times, and in the present study, we used the second BP measurement for the analysis. People with a ⩾140 mm Hg systolic BP and ⩾90 mm Hg diastolic BP were classified as having a high BP.
Biomonitoring
Urine was only collected for selected people (approximately 20–30% of the whole cohort, still representative) to measure environmental chemical concentrations. Urine specimens were processed, stored and shipped to the Division of Laboratory Sciences, National Center for Environmental Health, National Centers for Disease Control and Prevention, Atlanta, Georgia. Urinary environmental chemical concentrations for heavy metals, bisphenols and phthalates were determined by ICP-DRC-MS (inductively coupled plasma dynamic reaction cell mass spectroscopy) or detected using online solid-phase extraction, isotope dilution and high-performance liquid chromatography separation, followed by electrospray ionization and tandem mass spectrometry on those aged 6 years and above.9, 10, 11 Species of parabens in 100 μl urine were hydrolyzed and conjugated using β-glucuronidase/sulfatase (Helix pomatia, H1; Sigma Aldrich Laboratories, St Louis, MO, USA) and were preconcentrated by online solid-phase extraction, separated from other urine components by reversed-phase high-performance liquid chromatography, and detected by atmospheric pressure chemicaionization–isotope dilution/tandem mass spectrometry with peak focusing.12 Pesticides were measured using the isotope dilution technique and tandem mass spectrometry, and details can be found in Hill et al.13, 14 Because urinary environmental chemical concentrations were highly right skewed, they were all log transformed in the analyses.
Statistical analysis
Adults aged 20 years and above were included in the analysis. The effects of urinary environmental chemical concentrations on risk of high BP were examined by t-test and a logistic regression model, with P<0.05 considered to be statistically significant. Covariates including urinary creatinine, age, sex, ratio of family income to poverty (proxy of socioeconomic status) and body mass index (BMI)15 were adjusted. Models were also weighted for the survey design because urinary environmental chemical concentrations were measured in subsamples. The population attributable risk from an indoor temperature below a certain degree, which was to be determined, was calculated based on the formula introduced by Fleiss in 1979.16 In the subsequent analysis, sex differences were assessed. Statistical software STATA version 13.0 (STATA, College Station, TX, USA) was used to perform all of the analyses. Because the present study was only a secondary data analysis, no further ethics approval was required.
Results
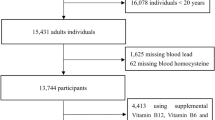
The study cohort in 2009–2012 contained 20 293 participants with 6191 people being classified as having a high BP (30%). Table 1 presents the characteristics of the included participants. The average age was 32 years old (range: 20–80 years); 4380 (21.6%) were identified as overweight (BMI 25–30), while 6879 (33.9%) were classified as obese (BMI 30+). Table 2 shows the associations of urinary heavy metals and high BP. After full adjustments, urinary cesium (odds ratio (OR) 1.52, 95% confidence interval (CI) 1.06–2.18, P=0.026), molybdenum (OR 1.45, 95% CI 1.04–2.02, P=0.029), lead (OR 1.49, 95% CI 1.12–1.98, P=0.009), platinum (OR 1.66, 95% CI 1.14–2.21, P=0.002), antimony (OR 1.44, 95% CI 1.12–1.86, P=0.008) and tungsten (OR 1.48, 95% CI 1.22–1.79, P<0.001) concentrations were observed to be associated with high BP. They accounted for 7.2, 6.3, 6.8, 9.0, 6.2 and 6.7% of the population attributable risk, respectively.
Similarly, in Table 3, associations between industry-associated chemicals and high BP are displayed. To be specific, mono-2-ethyl-5-carboxypentyl (OR 1.29, 95% CI 1.04–1.59, P=0.024), mono-n-butyl (OR 1.36, 95% CI 1.11–1.67, P=0.005), mono-2-ethyl-5-hydroxyhexyl (OR 1.21, 95% CI 1.01–1.46, P=0.041), mono-n-methyl (OR 1.24, 95% CI 1.01–1.46, P=0.014), mono-2-ethyl-5-oxohexyl (OR 1.21, 95% CI 1.01–1.45, P=0.036) and mono-benzyl (OR 1.41, 95% CI 1.15–1.74, P=0.002) phthalate metabolites were found to be related to high BP. They accounted for 4.2, 5.1, 3.1, 3.5, 3.1 and 5.8% of population attributable risks, respectively. In Table 4, only dimethylarsonic acid (OR 1.38, 95% CI 1.08–1.76, P=0.012) and trimethylarsine oxide (OR 2.56, 95% CI 1.29–5.07, P=0.010) were associated with high BP, and they accounted for 5.4 and 19.0% of the population attributable risks.
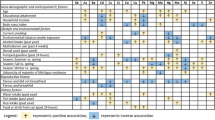
Tables 5 and 6 indicate the potential sex differences associated with urinary heavy metals, phthalate and arsenic and high BP. In men, urinary cobalt, cesium, lead, platinum, antimony, tungsten, mono-n-methyl, mono-benzyl and dimethylarsonic acid concentrations were associated with high BP, while in women, urinary molybdenumm, lead, platinum, antimony, tungsten, mono(carboxynonyl), mono-n-butyl, mono-(3-carboxypropyl), mono-ethyl, mono-benzyl, mono-isobutyl and trimethylarsine oxide concentrations were associated with high BP.
Discussion
Main findings
In the present national, population-based, multi-year, cross-sectional study, the relationships of different sets of urinary environmental chemical concentrations and high BP were examined. Higher urinary cesium, molybdenum, lead, platinum, antimony, tungsten, mono-2-ethyl-5-carboxypentyl phthalate, mono-n-butyl phthalate, mono-2-ethyl-5-hydroxyhexyl phthalate, mono-n-methyl phthalate, mono-2-ethyl-5-oxohexyl phthalate, mono-benzyl phthalate, dimethylarsonic acid and trimethylarsine oxide concentrations were associated with high BP. Each chemical could account for 3–18% of the population attributable risks for high BP. A small sex difference was found. However, there were no associations between environmental parabens and pesticides and high BP. Several more significant associations were found after covariate adjustments. However, those significant associations disappeared after additionally adjusting for subsample weighting, implying a failure to generalize those potential significant associations to the entire US population.
Previous studies and possible mechanisms
Cobalt is widely distributed in the environment, accounting for 0.001% of the Earth’s crust. Cobalt forms bivalent and trivalent compounds, those of biological interest being bivalent.17 In animal models, exposure to excess cobalt was found to have a toxic effect on the heart, including an elevated BP and may result in cardiomyopathy, although one study in rats showed the opposite.18, 19, 20, 21 Cesium was previously found in people exposed to Chernobyl radiation,22 and animal models in rats, dogs, rabbits, and in vivo have also observed that the cardiovascular system or coronary blood flow could be impaired after long-term contamination with cesium in drinking water.23, 24, 25, 26, 27 Lead was previously observed to enhance B-cell activity, impair host resistance to several bacterial and viral infections, and differentially modify cytokine production in vitro and in vivo.28 Lead exposure was found to result in a marked elevation in BP, a significant reduction in urinary nitric oxide metabolites (NO(chi)) excretion, and upregulation of endothelial and inducible nitric oxide synthase in the kidneys (which could impact filtration rate and normalization using creatinine), aorta, and heart and neuronal nitric oxide synthase in the cerebral cortex and brain stem in animals.29 Tungsten is thrombogenic and proinflammatory, but its toxicity and carcinogenicity in cardiovascular health is not well examined.30, 31 Tungsten coils were prevalent in clinical use for occluding intracranial aneurysms, varicocele veins and other abnormal vascular connections.32 Therefore, people with intracranial aneurysms after the treatment may experience higher tungsten volumes in the body than people without them. In subsequent analysis, after additionally excluding people with a history of a stroke, its effect on the risk for high BP has remained significant (data not shown). Antimony has long been related to pneumoconiosis and dermatitis (acute effect)33 and previously was also found to be correlated with cardiovascular end points in smelter workers and those with gastrointestinal disorders (chronic effect by inhalation).34, 35, 36
Phthalates, considered to be chemical estrogens, are widely used in the food packaging industry, leaching from the polymers into food and water under normal conditions37 and can be detected in human urine. They can migrate out of the plastic product and into the environment and are suspected to act as hormone mimics and endocrine-disrupting compounds.38, 39 Animal studies have shown that chronic exposure to these compounds, even at a low dose, can alter some biological end points.40, 41 Other evidence further showed that mono-butyl phthalate disturbs the glycolytic pathway and can suppress other proteins that are involved in DNA transcription, RNA biogenesis and protein synthesis.6 These compounds have been hypothesized to contribute to cardiovascular disease and highlight the need to eliminate these potential risks to prevent disease prevention. In recent meta-analyses, the pooled effect estimates of arsenic concentrations were found to be from 1.19 (95% CI 1.2–3.0) to 1.27 (95%CI 1.09–1.47).42, 43 In the present study, although the total arsenic concentration was not significantly associated with the risk of high BP, dimethylarsonic acid and trimethylarsine oxide concentrations were observed to be related to an increased risk of high BP, which is similar to a previous study using NHANES 2003–2008 data.44 Animal studies have also suggested that the chemical propensity of arsenic to oxidize vicinal thiols could potentially affect a number of cellular proteins with reactive thiols, including endothelial nitric oxide synthase.45 In the current analysis, there was somewhat of a sex difference, indicating that men might be more prone to exposure to heavy metals, while women might be more vulnerable to phthalates. The biological mechanism is unclear and requires future research.
Strengths and limitations
There are a few strengths and limitations worthy of being discussed. First, this study was conducted in a large, nationally representative human sample with mixed ethnicities. Moreover, different sets of chemicals were able to be included for examination. However, there could be still other chemicals in the environment that we might not yet be known and would need future research to identify and examine. Causality cannot be established in the present study due to the cross-sectional study design. Future studies with a longitudinal study design to confirm or refute the current findings and to understand the persisting risk throughout life from the above-mentioned environmental chemicals should be considered.
Conclusion
In summary, we have provided evidence for the association of urinary cesium, molybdenum, lead, platinum, antimony, tungsten, phthalates, and arsenic concentrations and high BP using a very recent, national, population-based human study sample with multiple ethnicities. Each chemical could account for 3–18% of the population attributable risk for high BP. There was also a small sex difference. Elimination of environmental chemicals should still be prioritized to aim for disease prevention and benefit population health in the coming decades. Future research with a longitudinal design to understand the persisting risk from the above-mentioned environmental chemicals is also recommended.
References
Gottlieb S . Nearly a third of US adults have high blood pressure. Br Med J 2004; 329: 531.
Revis NW, Zinsmeister AR, Bull R . Atherosclerosis and hypertension induction by lead and cadmium ions: an effect prevented by calcium ion. Proc Natl Acad Sci USA 1981; 78: 6494–6498.
Carter DE, Aposhian HV, Gandolfi AJ . The metabolism of inorganic arsenic oxides, gallium arsenide, and arsine: a toxicochemical review. Toxicol Appl Pharmacol 2003; 193: 309–334.
Navas-Acien A, Silbergeld EK, Sharrett R, Calderon-Aranda E, Selvin E, Guallar E . Metals in urine and peripheral arterial disease. Environ Health Perspect 2005; 113: 164–169.
Shiue I . Urine phthalate concentrations are higher in people with stroke: United States National Health and Nutrition Examination Surveys (NHANES), 2001-2004. Eur J Neurol 2013; 20: 728–731.
Olsén L, Lind L, Lind PM . Associations between circulating levels of bisphenol A and phthalate metabolites and coronary risk in the elderly. Ecotoxicol Environ Saf 2012; 80: 179–183.
Rogers JM, Ellis-Hutchings RG, Grey BE, Zucker RM, Norwood J Jr, Grace CE, Gordon C, Lau C . Elevated blood pressure in offspring of rats exposed to diverse chemicals during pregnancy. Toxicol Sci 2013; 137: 436–446.
Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention (2012) http://www.cdc.gov/nchs/nhanes.htm.
Silva MJ, Barr DB, Reidy JA, Malek NA, Hodge CC, Caudill SP, Brock JW, Needham LL, Calafat AM . Urinary levels of seven phthalate metabolites in the U.S. population from the National Health and Nutrition Examination Survey (NHANES) 1999–2000. Environ Health Perspect 2004; 112: 331–338.
Mulligan KJ, Davidson TM, Caruso JA . Feasibility of the direct analysis of urine by inductively coupled argon plasma mass-spectrometry for biological monitoring of exposure to metals. J Anal At Spectrom 1990; 5: 301–306.
Brock JW, Yoshimura Y, Barr JR, Maggio VL, Graiser SR, Nakazawa H, Needham LL . Measurement of bisphenol A levels in human urine. J Expo Anal Environ Epidemiol 2001; 11: 323–328.
Calafat AM, Ye X, Wong LY, Bishop AM, Needham LL . Urinary concentrations of four parabens in the U.S. population: NHANES 2005-2006. Environ Health Perspect 2010; 118: 679–685.
Hill RH Jr, Shealy DB, Head SL, Williams CC, Bailey SL, Gregg M, Needham LL . Pesticide residues in urine of adults living in the United States: reference range concentrations. Environ Res 1995; 71: 99–108.
Hill RH Jr, Shealy DB, Head SL, Williams CC, Bailey SL, Gregg M, Baker SE, Needham LL . Determination of pesticide metabolites in human urine using an isotope dilution technique and tandem mass spectrometry. J Anal Toxicol 1995; 19: 323–329.
BMI Classification. World Health Organization. http://www.who.int/mediacentre/factsheets/fs311/en/.
Fleiss JL . Inference about population attributable risk from cross-sectional studies. Am J Epidemiol 1979; 110: 103–104.
LaKind JS, Goodman M, Naiman DQ . Use of NHANES data to link chemical exposures to chronic diseases: a cautionary tale. PLoS ONE 2012; 7: e51086.
Expert Group on Vitamins and Minerals. Food Standard Agency, 2003. http://cot.food.gov.uk/cotreports/cotjointreps/evmreport/.
Dalhamn T . The effect of cobalt on blood pressure, respiration and mortality, and the use of dimercaprol (BAL) as antidote. Acta Pharmacol Toxicol (Copenh) 1953; 9: 259–266.
Morvai V, Szakmáry É, Tátrai E, Ungváry G, Folly G . The effects of simultaneous alcohol and cobalt chloride administration on the cardiovascular system of rats. Acta Physiol Hung 1993; 81: 253–261.
Sandusky GE, Henk WG, Roberts ED . Histochemistry and ultrastructure of the heart in experimental cobalt cardiomyopathy in the dog. Toxicol Appl Pharmacol. 1981; 61: 89–98.
Cwikel J, Abdelgani A, Goldsmith JR, Quastel M, Yevelson II . Two-year follow up study of stress-related disorders among immigrants to Israel from the Chernobyl area. Environ Health Perspect 1997; 105 (Suppl 6): 1545–1550.
Guéguen Y, Lestaevel P, Grandcolas L, Baudelin C, Grison S, Jourdain JR, Gourmelon P, Souidi M . Chronic contamination of rats with 137 cesium radionuclide: impact on the cardiovascular system. Cardiovasc Toxicol 2008; 8: 33–40.
Patterson E, Szabo B, Scherlag BJ, Lazzara R . Early and delayed afterdepolarizations associated with cesium chloride-induced arrhythmias in the dog. J Cardiovasc Pharmacol 1990; 15: 323–331.
Fish FA, Prakash C, Roden DM . Suppression of repolarization-related arrhythmias in vitro and in vivo by low-dose potassium channel activators. Circulation 1990; 82: 1362–1369.
Ooie T, Takahashi N, Saikawa T, Iwao T, Hara M, Sakata T . Suppression of cesium-induced ventricular tachyarrhythmias by atrial natriuretic peptide in rabbits. J Card Fail 2000; 6: 250–256.
D'Alonzo AJ, Hess TA, Darbenzio RB, Sewter JC . Effects of intracoronary cromakalim, pinacidil, or diltiazem on cesium chloride-induced arrhythmias in anesthetized dogs under conditions of controlled coronary blood flow. J Cardiovasc Pharmacol 1993; 21: 677–683.
Heo Y, Parsons PJ, Lawrence DA . Lead differentially modifies cytokine production in vitro and in vivo. Toxicol Appl Pharmacol 1996; 138: 149–157.
Vaziri ND, Ding Y, Ni Z . Compensatory up-regulation of nitric-oxide synthase isoforms in lead-induced hypertension; reversal by a superoxide dismutase-mimetic drug. J Pharmacol Exp Ther 2001; 298: 679–685.
Byrne JV, Hope JK, Hubbard N, Morris JH . The nature of thrombosis induced by platinum and tungsten coils in saccular aneurysms. AJNR Am J Neuroradiol 1997; 18: 29–33.
ATSDR. Toxicological Profile for Tungsten. Draft. GA:Agency for Toxic Substances and Disease Registry: Atlanta. 2003.
Peuster M, Fink C, von Schnakenburg C, Hausdorf G . Dissolution of tungsten coils does not produce systemic toxicity, but leads to elevated levels of tungsten in the serum and recanalization of the previously occluded vessel. Cardiol Young 2002; 12: 229–235.
McCallum RI . The industrial toxicology of antimony. The Ernestine Henry lecture 1987. J R Coll Physicians Lond 1989; 23: 28–32.
Schnorr TM, Steenland K, Thun MJ, Rinsky RA . Mortality in a cohort of antimony smelter workers. Am J Ind Med 1995; 27: 759–770.
Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Antimony. U.S. Public Health Service, U.S. Department of Health and Human Services: Altanta, GA. 1992.
U.S. Department of Health and Human Services. Hazardous Substances Data Bank (HSDB, online database). National Toxicology Information Program, National Library of Medicine: Bethesda, MD. 1993.
Brotons JA, Olea-Serrano MF, Villalobos M, Pedraza V, Olea N . Xenoestrogens released from lacquer coatings in food cans. Environ Health Perspect 1995; 103: 608–612.
Halden RU . Plastics and Health Risks. Annu Rev Public Health 2010; 31: 179–194.
Heudorf U, Mersch-Sundermann V, Angerer J . Phthalates: toxicology and exposure. Int J Hyg Environ Health 2007; 210: 623–634.
Bisset KM, Dhopeshwarkar AS, Liao C, Nicholson RA . The G protein-coupled cannabinoid-1 (CB1) receptor of mammalian brain: Inhibition by phthalate esters in vitro. Neurochem Int 2011; 59: 706–713.
Osman AM, van Dartel DA, Zwart E, Blokland M, Pennings JL, Piersma AH . Proteome profiling of mouse embryonic stem cells to define markers for cell differentiation and embryotoxicity. Reprod Toxicol 2010; 30: 322–332.
Abir T, Rahman B, D’Este C, Farooq A, Milton AH . The association between chronic arsenic exposure and hypertension: a meta-analysis. J Toxicol 2012; 2012: 198793.
Abhyankar L, Jones MR, Guallar E, Navas-Acien A . Arsenic exposure and hypertension: a systematic review. Environ Health Perspect 2012; 120: 494–500.
Jones MR, Tellez-Plaza M, Sharrett AR, Guallar E, Navas-Acien A . Urine arsenic and hypertension in US adults: the 2003-2008 National Health and Nutrition Examination Survey. Epidemiology 2011; 22: 153–161.
Kumagai Y, Pi J . Molecular basis for arsenic-induced alternation in nitric oxide production and oxidative stress: implication of endothelial dysfunction. Toxicol Appl Pharmacol 2004; 198: 450–457.
Acknowledgements
IS is supported by the Global Platform for Research Leaders scheme.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shiue, I., Hristova, K. Higher urinary heavy metal, phthalate and arsenic concentrations accounted for 3–19% of the population attributable risk for high blood pressure: US NHANES, 2009–2012. Hypertens Res 37, 1075–1081 (2014). https://doi.org/10.1038/hr.2014.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.121
Keywords
This article is cited by
-
Association between multiple metal(loid)s exposure and renal function: a cross-sectional study from southeastern China
Environmental Science and Pollution Research (2023)
-
Relationships Between Urinary Metals and Diabetes Traits Among Mexican Americans in Starr County, Texas, USA
Biological Trace Element Research (2023)
-
Combined exposure to multiple metals on hypertension in NHANES under four statistical models
Environmental Science and Pollution Research (2023)
-
The association between environmental cadmium exposure, blood pressure, and hypertension: a systematic review and meta-analysis
Environmental Science and Pollution Research (2022)
-
Environmental exposure to metals and the risk of high blood pressure: a cross-sectional study from NHANES 2015–2016
Environmental Science and Pollution Research (2022)