Abstract
Arterial stiffness is a significant predictor of cardiovascular disease (CVD), the risk of which is modified by medications for atherosclerotic risk factors and life-style changes. Cardio-ankle vascular index (CAVI) provides noninvasive, objective information on arterial stiffness, independent of blood pressure. This study aimed to investigate changes in CAVI after management of atherosclerotic risk factors, and the impact of these changes on future CVD outcomes in patients with coronary artery disease (CAD). The study consisted of 211 CAD patients (65±10 years, 118 men) with impaired CAVI. CAVI examination was repeated 6 months later. Impaired CAVI was defined as greater than the mean plus 1 s.d. of the age- and gender-specific normal CAVI values, according to results obtained in 5188 healthy subjects. All patients were followed for >1 year or until the occurrence of a CVD event. Of the 211 patients, CAVI improved in 106 (50%) patients after 6 months, but remained high in 105 (50%) patients. During follow-up (2.9±1.0 years), CVD events occurred in 28 (13%) patients. Persistently impaired CAVI was an independent predictor of future CVD events (P=0.01), independent of baseline CAVI. CVD outcomes were worse in patients with persistently impaired CAVI than in those with improved CAVI (P<0.001). Among patients with a normalized CAVI after treatment (n=22) only one suffered a CVD event. This study was the first to demonstrate that persistent impairment of arterial stiffness was an independent risk factor of future CVD events. Serial measurements of CAVI provide important prognostic information regarding patients with CAD in clinical practice.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in most developed countries. Among markers of CVD, arterial stiffness has proven to be an important parameter in the assessment of cardiovascular risk and an independent strong predictor of future CVD events. Arterial stiffness correlates primarily with arterial structural changes, including elastin fragmentation and degeneration, collagen accumulation, thickening of the arterial wall and progressive arterial dilation.1, 2 A number of investigations have reported the reversibility of arterial stiffness after reduction of atherosclerotic risk factors by pharmacological intervention and life-style modifications.3, 4, 5, 6 We hypothesized that serial assessments of arterial stiffness after comprehensive treatment of atherosclerotic risk factors, rather than a one-time assessment, provide an accurate estimate of the risk of future CVD events. This study was designed to investigate improvement in impaired arterial stiffness induced by treatment of atherosclerotic risk factors in association with future CVD events in patients with coronary artery disease (CAD).
Among the different methods currently available for assessing arterial stiffness, the cardio-ankle vascular index (CAVI) was used in this study for its noninvasive, quantitative and objective nature, and its independence from arterial blood pressure.7, 8 This study also used measurement of carotid artery intima-media thickness (IMT) as a surrogate marker for the early stage of structural changes of atherosclerosis.
Methods
A total of 371 consecutive patients with newly diagnosed CAD who underwent coronary computed tomographic angiography (CCTA) between March 2008 and April 2011 were initially enrolled in this study. The presence of CAD was defined as coronary artery segments exhibiting plaque with a luminal diameter stenosis of 50% or more on CCTA. Patients with a history of percutaneous coronary intervention were not enrolled in this study. Of the 371 patients, 184 patients (50%) were referred for exercise or pharmacological stress myocardial perfusion imaging. One hundred and twenty patients (65%) were found to have normal perfusion imaging, and 64 patients (35%) were referred for invasive coronary angiography. The other 32 patients (8.6%) were referred for subsequent invasive coronary angiography without stress myocardial perfusion imaging because of the presence of severe CAD. The remaining 155 patients (42%) received medical therapy without stress myocardial perfusion imaging, defined by the patient’s attending physician after taking into consideration the patient’s condition, including age, comorbid diseases and severity of CAD. A total of 96 patients (26%) underwent invasive coronary angiography and 15 patients (4.0%) underwent subsequent coronary revascularization. These patients had their first CAVI examination at the time of diagnosis, and patients with an impaired CAVI (defined as greater than the mean plus 1 s.d. of the age- and gender-specific normal CAVI values) were included. The exclusion criteria were follows: (1) CVD event within 4 weeks of enrollment and during the 6-month period between the first and second CAVI tests; (2) left ventricular ejection fraction <30% on echocardiography; (3) history of peripheral arterial disease; (4) chronic kidney disease (estimated glomerular filtration rate <60 ml min–1 per 1.73 m2), including maintenance hemodialysis; (5) atrial fibrillation and (6) the presence of other serious systemic diseases.
Among the 371 patients with CAD, 160 patients were excluded: 132 patients were excluded because of an unimpaired CAVI (⩽ age- and gender-specific cutoff value of control subjects): 6 patients suffered a CVD event between their first and second CAVI tests, and 22 patients met one of the other exclusion criteria. Therefore, the final population was 211 patients (65±10 years, 118 men). The second CAVI test was performed 6 months after the first, and patients were then classified as having improved CAVI (the second CAVI was better than the first), or persistently impaired CAVI. Blood pressure, body mass index, serum cholesterol, C-reactive protein, fasting glucose, hemoglobin (Hb)-A1c and carotid ultrasound examination for IMT measurements were also assessed at the times of the first and second CAVI tests.
This study also included 5188 healthy subjects (43±11 years, 1872 men) with no history of CVD and no risk factors based on a cardiovascular screening program to define the age- and gender-specific normal CAVI values: 4988 subjects were selected from an epidemiological study9 and 200 subjects were chosen from a cardiovascular screening program at Osaka Ekisaikai Hospital. Written informed consent was obtained from all patients and control subjects before the study. This study was approved by the Institutional Review Board of Osaka Ekisaikai Hospital. Informed consent was obtained from each patient, and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee.
CAVI was measured after 12 h of fasting, 3 days (first CAVI) before the CCTA examination and repeated 6 months after the first CAVI test (second CAVI) in all study patients. After the first CAVI test, all patients received optimized therapy for atherosclerotic risk factors and life-style modifications according to AHA/ACC guidelines.10, 11 The target values were as follows: (1) hypertension (blood pressure of <140/90 mm Hg or 130/80 mm Hg in the presence of diabetes or CAD); (2) low-density lipoprotein cholesterol <100 mg dl–1 (2.6 mmol l–1); (3) HbA1c <7.0% for diabetes control. Framingham risk score (FRS) was calculated at the time of the second examination.12 Patients were encouraged to quit smoking and to continue an appropriate balance of physical activity and caloric intake.10
After the second CAVI test, all 211 patients were followed every month at our institution for >1 year or until the occurrence of one of the following CVD events: cardiac death, non-fatal myocardial infarction, unstable angina pectoris, recurrent angina pectoris requiring coronary revascularization or stroke. Non-fatal myocardial infarction was defined by the European Society of Cardiology/American College of Cardiology Committee, and unstable angina was defined according to the Braunwald classification. The diagnosis of stroke was made by neurological examination and brain magnetic resonance imaging. The same medications prescribed during the 6 months between the first and second CAVI tests, as well the as the recommended diet and life-style modifications, were continued in each patient throughout the follow-up period.
CAVI, a measure of arterial stiffness, was calculated with the patient in the supine position. CAVI was assessed with an automatic device, the VaSera (Fukuda Denshi, Tokyo, Japan), which measures the time delay between the rapid upstroke of simultaneously recorded pulse waves in the brachial and ankle arteries. The distance between the recording sites on the brachial and ankle arteries was measured with a tape over the body surface. CAVI was calculated by substituting the stiffness parameter, β, into the following equation.7, 8, 13 Stiffness parameter β, recognized as a blood pressure-independent parameter of arterial stiffness, was calculated as follows:

On the other hand, pulse wave velocity (PWV) was derived from Bramwell–Hill’s equation as follows:

On the basis of these two equations, CAVI was calculated as follows:

(D, diameter; Ps, systolic blood pressure; Pd, diastolic blood pressure; ΔP, pulse pressure (Ps–Pd); ρ, blood density).

The values of a and b are constants in order to make the units of CAVI comparable to those of PWV.
Carotid IMT was measured by B-mode ultrasonography using a 7.5-MHz linear array transducer.14 The beginning of the dilatation of the distal common carotid artery served as a reference point for the start of each measurement. The average of IMT of each of three frozen images was calculated. For each individual, IMT was determined as the average of near- and far-wall measurements of both the left and right common carotid arteries.
CCTA was performed using a SOMATOM Sensation 64 system (Siemens Medical Systems, Forchheim, Germany), with the following scan parameters: 64 × 0.6 mm collimation, tube voltage of 120 kV, gantry rotation time of 330 ms and tube current rotation time of 770–850 mAs. CCTA was performed in accordance with the protocol in our previous reports.15, 16
All CCTA data sets were analyzed on a per-segment basis by two experienced readers. Coronary arteries were divided into 15 separate segments that were 1.5 mm or more in diameter as measured by CCTA. Coronary atherosclerotic lesions were quantified for stenosis by visual estimation. The severity of luminal-diameter stenosis was divided into non-obstructive plaques (<50% luminal stenosis) and obstructive plaques (>50% luminal stenosis). Two vessels, three vessels and left main CAD were defined as a multi-vessel CAD.
Categorical variables are presented as a number (%), and continuous variables, as the mean±s.d. The χ2 test was used for comparison of categorical variables. Continuous variables were compared by unpaired t-test or Mann–Whitney U-test, according to the data distribution. The baseline characteristics for patients with and without impaired CAVI, and for those excluded because of other exclusion criteria, were compared using one-way analysis of variance for parametric data distribution or Kruskal–Wallis test for nonparametric data distribution. The values of CAVI before and 6 months after optimized therapy were compared between groups with improved CAVI and persistently impaired CAVI using two-way repeated-measures analysis of variance. Cox proportional hazard analysis was performed to identify predictors of CVD events. Baseline variables that were considered clinically relevant or showed a univariate relationship with outcome were entered into the analysis. The Kaplan–Meier survival method was used to compare survival during follow-up, using the log-rank test. A P-value <0.05 was considered statistically significant.
Results
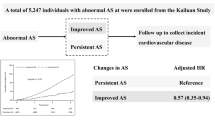
The characteristics and age- and gender-specific CAVI values of the control subjects are shown in Table 1. Age-specific CAVI values became higher in both genders as their ages increased by 10-year intervals. Table 2 shows baseline characteristics, which compared the clinical variables of patients with and without impaired CAVI, as well as those patients who were excluded because of other exclusion criteria, including the six patients with a CVD event between their first and second CAVI tests. There were no significant differences in clinical characteristics among the three groups, except for CAVI value (P=0.002), estimated glomerular filtration rate (P=0.04) and left ventricular ejection fraction (P<0.001) by the definition. The CAD vessel number was similar among the three groups. The characteristics of the study patients at study enrollment are shown in Table 3. Among 211 patients with impaired CAVI, CAVI improved in 106 (50%) patients after 6 months, whereas impaired CAVI persisted in the remaining 105 (50%) patients (Figure 1). CAVI was normalized in 22 (10%) patients.
The baseline characteristics, including blood pressure, body mass index and cholesterol profiles, were comparable between the two groups (Table 3). At the second CAVI examination, HbA1c was higher in patients with persistently impaired CAVI than in patients with improved CAVI (P=0.006; Table 4). However, the two groups demonstrated equal improvement in atherosclerotic risk factors, including blood pressure and cholesterol profiles, at the second CAVI test, and the percent change in risk status between the first and second CAVI tests was comparable. We performed univariate and multivariate analyses to determine the regression of CAVI. There were no significant differences in any variables between patients with or without regression of CAVI (Tables 3 and 4). In addition, we performed a multivariate analysis including the following variables that were considered clinically relevant: age, male gender, hypertension, hyperlipidemia, diabetes, heart rate and changes in heart rate. As a result, multivariate analysis failed to show an independent determinant for the regression of CAVI (P-values did not reach statistical significance).
All medications used at baseline and at the second CAVI test (for example, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, beta-blockers, calcium channel blockers, statins, antiplatelet drugs, oral antidiabetic drugs and insulin) were comparable between the two groups (Table 5). In addition, 53 patients were prescribed one or more of these medications between first and second CAVI tests. CAVI values at the first (10.17 vs. 9.92, P=0.07) and second CAVI tests (10.16 vs. 9.95, P=0.09), as well as the changes in these values (−0.01 vs. 0.03, P=0.7), were similar between patients who started using statins and other medications.
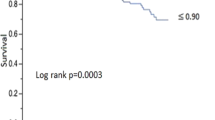
During a mean follow-up period of 2.9±1.0 years, which ranged from 6 months to 4.9 years (median 3.4 years) after second CAVI examination, 28 of the following CVD events were registered: cardiac death in 2 patients, non-fatal myocardial infarction in 4 patients, unstable angina in 12 patients, recurrent angina pectoris requiring coronary revascularization in 5 patients and stroke in 5 patients. Initial CAVI values were not predictive of event occurrence in the univariate analysis (Table 6). In addition, there was no significant prognostic difference between patients with CAVI values above or below the median in the first CAVI test (P=0.32), as shown in Figure 2a. By contrast, patients with persistently impaired CAVI had 21 (20%) CVD events, whereas patients with improved CAVI had only 7 (6.6%) CVD events (P<0.001). Kaplan–Meier analysis demonstrated significantly worse CVD outcomes for patients with persistently impaired CAVI compared with the other group (P<0.001; Figure 2b). Only 1 of 21 patients in whom CAVI normalized after treatment developed a CVD event during the follow-up period.
(a) Comparison of Kaplan–Meier curves of event-free survival between patients above the median and below the median CAVI value in the first CAVI test. (b) Comparison of Kaplan–Meier curves of event-free survival between patients with persistently impaired CAVI and improved CAVI. CAVI, cardio-ankle vascular index.
Table 6 shows the results of a comparison of patient clinical characteristics at the first CAVI test and the percent change in risk status from the first to the second test in patients with and without CVD events. Patients with CVD events were more likely to have diabetes (P=0.01), multi-vessel CAD (P=0.03) and persistently impaired CAVI (P=0.002) than patients without CVD events. Other atherosclerotic risk factors such as blood pressure, body mass index and cholesterol profiles were comparable between the two groups.
Patients with persistently impaired CAVI tended to have higher FRS compared with patients with improved CAVI (15.0±4.4 vs. 14.1±4.7, P=0.13). Patients who suffered a CVD event also tended to have higher FRS compared with patients who did not (15.7±2.7 vs. 14.3±4.8, P=0.14), but these values were not statistically significant. Furthermore, we performed a multivariate Cox proportional hazard analysis, which included diabetes, multi-vessel disease, second brachial-ankle PWV, persistently impaired CAVI and FRS, in order to predict future CVD events. HbA1c was excluded from the covariates in this analysis because it was initially associated with diabetes. ΔCAVI was also excluded because it was initially associated with persistently impaired CAVI. Cox proportional hazards model analysis showed that multi-vessel CAD (hazard ratio: 2.2, 95% confidence interval: 1.02–4.89, P=0.04), and persistently impaired CAVI (hazard ratio: 3.3, 95% confidence interval: 1.47–8.59, P<0.01) were independent predictors of future CVD events (model 1, Table 7). When multivariate analysis was repeated with the addition of the absolute value of the second CAVI instead of ‘persistent impairment of arterial stiffness,’ the second CAVI value was found to be an independent predictor of future CVD events (hazard ratio: 1.8, 95% confidence interval: 1.18–2.74, P<0.01; model 2, Table 7). Patients with CVD events had higher brachial-ankle PWV values at the second test than those without CVD events (Table 6). However, brachial-ankle PWV at the second test was found to be insignificant in the multivariate analysis (Table 7).
Discussion
This study demonstrated that arterial stiffness, as estimated by CAVI, did not improve even after comprehensive treatment of atherosclerotic risk factors in approximately half of the patients with CAD. This is the first study focusing on persistently impaired arterial stiffness, which primarily reflected CAVI after treatment, as an independent risk for poor CVD outcome. Only one of the patients in whom CAVI normalized after treatment suffered a CVD event.
Arterial stiffness develops from interactional changes involving structural and cellular elements of the arterial walls.1, 2 Several previous studies demonstrated the importance of assessing arterial stiffness as a predictor of all-cause and CVD mortality for various diseases, independent of classical CVD risk factors. The results of these observations stressed the importance of arterial stiffness as an index for assessing the severity of atherosclerosis. Furthermore, increased arterial stiffness is also reportedly associated with endothelial dysfunction and inflammation, an association linked to future CVD events.17
CAVI has been validated by the stiffness parameter β in the thoracic descending aorta and the carotid artery.18 The correlations of CAVI with other atherosclerotic parameters (age, carotid IMT and CAD severity) were superior to those between CAVI and PWV. In addition, the independence of CAVI from arterial blood pressure has been reported.3, 18 On the other hand, several studies have already shown that life-style modification and medical therapies, such as smoking cessation,4 blood glucose control,5 control of hypertension6 and lipid-lowering therapies, improved CAVI.19, 20 To our knowledge, however, there are no studies regarding the prognostic value of CAVI on long-term CVD outcomes.
In this study, impaired CAVI did not improve after 6 months of comprehensive treatment of atherosclerotic risk factors in 50% of patients with CAD. This finding suggests that CAVI may reflect irreversible organ damage and functionally reversible arterial stiffness in patients with advanced atherosclerosis. CAVI values before the treatment of atherosclerotic risks could not distinguish between irreversible and reversible arterial stiffness after managing atherosclerotic risks. In fact, the value of the first CAVI at study enrollment did not correlate with future CVD events in this study. All patients enrolling in our study had impaired CAVI and concomitant CAD. Serial measurements of CAVI, particularly after treatment, seem to help identifying high-risk patients requiring more aggressive management, as well as providing the pathogenic mechanisms of arterial stiffness in patients with advanced atherosclerosis in clinical practice.
Another important finding of this study was that all clinical variables, including, medication usage and risk factor modification after comprehensive therapy, were similar between patients with persistently impaired CAVI and those with improved CAVI. In addition, the clinical variables and changes in these variables did not predict the improvement of CAVI. This may be explained as follows: first, individual risk factors, such as blood pressure, lipid profile and blood glucose, may fluctuate over time, and their values may not reflect their true impact on the arterial wall; second, the response to medications varies among individuals and multiple parameters have been reported that contribute to this variation (age, smoking status and insulin resistance).21, 22 Finally, there may be class effects of specific medications, such as antihypertensive agents causing the regression of structural changes to the arterial wall, and statins modifying both endothelial function and arterial stiffness.22, 23, 24 CAVI is an integrated parameter that reflects the severity of atherosclerosis of the arterial wall, and serves as an additional prognostic importance to stratify CAD patients at risk of developing CVD, beyond the assessment of traditional atherosclerotic risk factors.
Furthermore, as expected, carotid IMT did not change during the 6-month follow-up period of this study. Controversy still exists on the use of IMT in both the management and prediction of CAD.14, 25 A recent meta-analysis also showed no association between IMT progression and 7-year CVD outcome.26 These findings suggest the superiority of CAVI over IMT as a surrogate maker of CVD risk in response to management of atherosclerosis, particularly over short-term follow-up periods. Overcoming inherent methodological limitations of current IMT measurement via novel echocardiographic techniques, such as an automatic tracking system or three-dimensional image acquisition, may enable the combination of IMT and CAVI to be useful for more detailed risk stratification based on their representation of different aspects of atherosclerosis.
This study has limitations that need to be acknowledged. First, this study was based on a relatively small sample size. Furthermore, patients with normal CAVI values at the beginning of the study were not enrolled because this study was designed to investigate the potential of CAVI for further risk stratification of CAD by evaluating impaired arterial stiffness in relation to the treatment of atherosclerotic risk factors. Future studies with a larger number of patients are required to fully explore the factors associated with improvement of CAVI and the role of persistently impaired arterial stiffness in the pathogenesis and progression of atherosclerosis. Second, central blood pressure is noted as a factor associated with future CVD events,27 which was not accounted for by CAVI measurements. In addition, heart-femoral PWV was not measured. CAVI has been validated in prior studies against other markers of arterial stiffness (stiffness parameter β); however, these studies were based on relatively small sample sizes.28, 29 Therefore, the validity of CAVI as a maker of arterial stiffness should be confirmed either in future studies with a larger number of subjects or in comparison with pathological findings. Third, excellent reproducibility of CAVI was reported in previous studies.17 Unfortunately, this study was not designed to confirm the reproducibility of CAVI. Therefore, it was unclear whether the reproducibility of CAVI affected the results of this study. Finally, we used CCTA to enroll a more general patient population, and patients who underwent CCTA may not be representative of average patients with CAD scheduled for invasive coronary angiography. Careful attention may be necessary to extrapolate the results of this study. CCTA is an established modality that provides non-invasive diagnosis of CAD, especially for the exclusion of CAD, although CCTA may overestimate the severity of CAD. Therefore, other imaging modalities, such as invasive coronary angiography, should be used to confirm the presence of CAD in future investigations.
This study is the first to demonstrate that persistent impairment of arterial stiffness was associated with future CVD events, even after comprehensive management of traditional atherosclerotic risk factors. Serial measurements of CAVI, especially after treatment, provided important prognostic information on patients with CAD in clinical practice.
References
Lakatta EG . Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: part III: cellular and molecular clues to heart and arterial aging. Circulation 2003; 107: 490–497.
Zieman SJ, Melenovsky V, Kass DA . Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol 2005; 25: 932–943.
Shirai K, Song M, Suzuki J, Kurosu T, Oyama T, Nagayama D, Miyashita Y, Yamamura S, Takahashi M . Contradictory effects of beta1- and alpha1- aderenergic receptor blockers on cardio-ankle vascular stiffness index (CAVI)—CAVI independent of blood pressure. J Atheroscler Thromb 2011; 18: 49–55.
Noike H, Nakamura K, Sugiyama Y, Iizuka T, Shimizu K, Takahashi M, Hirano K, Suzuki M, Mikamo H, Nakagami T, Shirai K . Changes in cardio-ankle vascular index in smoking cessation. J Atheroscler Thromb 2010; 17: 517–525.
Ohira M, Endo K, Oyama T, Yamaguchi T, Ban N, Kawana H, Nagayama D, Nagumo A, Saiki A, Murano T, Watanabe H, Miyashita Y, Shirai K . Improvement of postprandial hyperglycemia and arterial stiffness upon switching from premixed human insulin 30/70 to biphasic insulin aspart 30/70. Metabolism 2010; 60: 78–85.
Sasaki H, Saiki A, Endo K, Ban N, Yamaguchi T, Kawana H, Nagayama D, Ohhira M, Oyama T, Miyashita Y, Shirai K . Protective effects of efonidipine, a t- and l-type calcium channel blocker, on renal function and arterial stiffness in type 2 diabetic patients with hypertension and nephropathy. J Atheroscler Thromb 2009; 16: 568–575.
Nakamura K, Tomaru T, Yamamura S, Miyashita Y, Shirai K, Noike H . Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J 2008; 72: 598–604.
Shirai K, Hiruta N, Song M, Kurosu T, Suzuki J, Tomaru T, Miyashita Y, Saiki A, Takahashi M, Suzuki K, Takata M . Cardio-ankle vascular index (CAVI) as a novel indicator of arterial stiffness: theory, evidence and perspectives. J Atheroscler Thromb 2011; 18: 924–938.
Namekata T, Suzuki K, Ishizuka N, Shirai K . Establishing baseline criteria of cardio-ankle vascular index as a new indicator of arteriosclerosis: a cross-sectional study. BMC Cardiovasc Disord 2011; 11: 51.
Smith SC Jr, Blair SN, Bonow RO, Brass LM, Cerqueira MD, Dracup K, Fuster V, Gotto A, Grundy SM, Miller NH, Jacobs A, Jones D, Krauss RM, Mosca L, Ockene I, Pasternak RC, Pearson T, Pfeffer MA, Starke RD, Taubert KA . AHA/ACC Guidelines for Preventing Heart Attack and Death in Patients With Atherosclerotic Cardiovascular Disease: 2001 update. A statement for healthcare professionals from the American Heart Association and the American College of Cardiology. J Am Coll Cardiol 2001; 38: 1581–1583.
Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, Ferguson TB Jr, Fihn SD, Fraker TD Jr, Gardin JM, O'Rourke RA, Pasternak RC, Williams SV . ACC/AHA 2002 guideline update for the management of patients with chronic stable angina—summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients with Chronic Stable Angina). J Am Coll Cardiol 2003; 41: 159–168.
Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB . Prediction of coronary heart disease using risk factor categories. Circulation 1998; 97: 1837–1847.
Park He, Choi SY, Kim MK, Oh BH . Cardio-ankle vascular index reflects coronary atherosclerosis in patients with abnormal glucose metabolism: assessment with 256 slice multi-detector computed tomography. J Cardiol 2012; 60: 372–376.
Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE . Common carotid intima-media thickness and risk of stroke and myocardial infarction: the rotterdam study. Circulation 1997; 96: 1432–1437.
Nakanishi K, Fukuda S, Shimada K, Ehara S, Inanami H, Matsumoto K, Taguchi H, Muro T, Yoshikawa J, Yoshiyama M . Non-obstructive low attenuation coronary plaque predicts three-year acute coronary syndrome events in patients with hypertension: multidetector computed tomographic study. J Cardiol 2012; 59: 167–175.
Otsuka K, Fukuda S, Tanaka A, Nakanishi K, Taguchi H, Yoshikawa J, Shimada K, Yoshiyama M . Napkin-ring sign on coronary CT angiography for the prediction of acute coronary syndrome. JACC Cardiovasc Imaging 2013; 6: 448–457.
van Bussel BC, Schouten F, Henry RM, Schalkwijk CG, de Boer MR, Ferreira I, Smulders YM, Twisk JW, Stehouwer CD . Endothelial dysfunction and low-grade inflammation are associated with greater arterial stiffness over a 6-year period. Hypertension 2011; 58: 588–595.
Kubozono T, Miyata M, Ueyama K, Nagaki A, Otsuji Y, Kusano K, Kubozono O, Tei C . Clinical significance and reproducibility of new arterial distensibility index. Circ J 2007; 71: 89–94.
Miyashita Y, Endo K, Saiki A, Ban N, Yamaguchi T, Kawana H, Nagayama D, Ohira M, Oyama T, Shirai K . Effects of pitavastatin, a 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitor, on cardio-ankle vascular index in type 2 diabetic patients. J Atheroscler Thromb 2009; 16: 539–545.
Satoh N, Shimatsu A, Kotani K, Himeno A, Majima T, Yamada K, Suganami T, Ogawa Y . Highly purified eicosapentaenoic acid reduces cardio-ankle vascular index in association with decreased serum amyloid a-ldl in metabolic syndrome. Hypertens Res 2009; 32: 1004–1008.
Shear CL, Franklin FA, Stinnett S, Hurley DP, Bradford RH, Chremos AN, Nash DT, Langendorfer A . Expanded clinical evaluation of lovastatin (EXCEL) study results. Effect of patient characteristics on lovastatin-induced changes in plasma concentrations of lipids and lipoproteins. Circulation 1992; 85: 1293–1303.
Kono Y, Fukuda S, Shimada K, Nakanishi K, Otsuka K, Kubo T, Jissho S, Taguchi H, Yoshikawa J, Yoshiyama M . Very rapid effect of pitavastatin on microvascular function in comparison to rosuvastatin: reactive hyperemia peripheral arterial tonometric study. Drug Des Devel Ther 2013; 7: 369–374.
Sakabe K, Fukuda N, Fukuda Y, Wakayama K, Nada T, Morishita S, Shinohara H, Tamura Y . Comparisons of short- and intermediate-term effects of pitavastatin versus atorvastatin on lipid profiles, fibrinolytic parameter, and endothelial function. Int J Cardiol 2008; 125: 136–138.
Cavalcante JL, Lima JA, Redheuil A, Al-Mallah MH . Aortic stiffness: current understanding and future directions. J Am Coll Cardiol 2011; 57: 1511–1522.
Costanzo P, Perrone-Filardi P, Vassallo E, Paolillo S, Cesarano P, Brevetti G, Chiariello M . Does carotid intima-media thickness regression predict reduction of cardiovascular events? A meta-analysis of 41 randomized trials. J Am Coll Cardiol 2010; 56: 2006–2020.
Lorenz MW, Polak JF, Kavousi M, Mathiesen EB, Volzke H, Tuomainen TP, Sander D, Plichart M, Catapano AL, Robertson CM, Kiechl S, Rundek T, Desvarieux M, Lind L, Schmid C, DasMahapatra P, Gao L, Ziegelbauer K, Bots ML, Thompson SG . Carotid intima-media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): a meta-analysis of individual participant data. Lancet 2012; 379: 2053–2062.
Pini R, Cavallini MC, Palmieri V, Marchionni N, Di Bari M, Devereux RB, Masotti G, Roman MJ . Central but not brachial blood pressure predicts cardiovascular events in an unselected geriatric population: the ICARe Dicomano Study. J Am Coll Cardiol 2008; 51: 2432–2439.
Takaki A, Ogawa H, Wakeyama T, Iwami T, Kimura M, Hadano Y, Matsuda S, Miyazaki Y, Matsuda T, Hiratsuka A, Matsuzaki M . Cardio-ankle vascular index is a new noninvasive parameter of arterial stiffness. Circ J 2007; 71: 1710–1714.
Takaki A, Ogawa H, Wakeyama T, Iwami T, Kimura M, Hadano Y, Matsuda S, Miyazaki Y, Hiratsuka A, Matsuzaki M . Cardio-ankle vascular index is superior to brachial-ankle pulse wave velocity as an index of arterial stiffness. Hypertens Res 2008; 31: 1347–1355.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Otsuka, K., Fukuda, S., Shimada, K. et al. Serial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery disease. Hypertens Res 37, 1014–1020 (2014). https://doi.org/10.1038/hr.2014.116
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.116
Keywords
This article is cited by
-
Acute effects of low-volume intermittent versus higher-volume continuous exercise on arterial stiffness in healthy young men
Scientific Reports (2022)
-
Insufficient blood pressure control is independently associated with increased arterial stiffness
Hypertension Research (2022)
-
The independent association between salivary alpha-amylase activity and arterial stiffness in Japanese men and women: the Toon Health Study
Hypertension Research (2022)
-
Psychological stress-induced increase in the cardio-ankle vascular index (CAVI) may be a predictor of cardiovascular events
Hypertension Research (2022)
-
Brachial-ankle pulse wave velocity and prognosis in patients with atherosclerotic cardiovascular disease: a systematic review and meta-analysis
Hypertension Research (2021)