Abstract
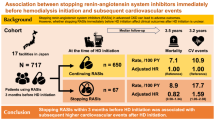
Suppression of the renin–angiotensin system is known to slow progression of chronic kidney disease (CKD). However, few trials have been performed with Japanese patients. This study investigated whether the angiotensin receptor blocker (ARB) valsartan would delay the progression of kidney disease more effectively than conventional treatment in Japanese hypertensive patients with advanced, predialysis CKD. In a multicenter, randomized, open-label trial, 303 patients with hypertension and CKD with serum creatinine levels ⩾2.0 mg dl−1 were assigned to receive either conventional therapy plus valsartan (valsartan add-on group) or conventional therapy without ARB (control group). The primary outcome was a change in serum creatinine levels. Changes in urinary protein levels and time to onset of renal events were analyzed as secondary end points. There were no between-group differences in blood pressure during the study. Changes in serum creatinine and urinary protein levels did not differ between the groups. However, the rate of renal events, including doubling of serum creatinine levels or end-stage renal disease, was significantly lower in the valsartan add-on group than in the control group. The addition of valsartan decreased the risk by 42.6% after adjustment for baseline variables. The addition of valsartan to conventional therapy significantly slowed the rate of renal function decline and delayed the need for renal replacement therapy in Japanese hypertensive patients with advanced CKD.
Similar content being viewed by others
Introduction
The number of patients developing end-stage renal disease (ESRD) has increased continuously over the past 10 years in Japan.1 Most of these patients have a progressive decline of renal function over many years before renal replacement therapy (RRT) is required. In numerous Western studies,2, 3 blockade of the renin–angiotensin system (RAS) with either angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin II type 1 receptor blockers (ARBs) has been shown to delay the progression of disease in patients with chronic kidney disease (CKD). Based on these studies, many guidelines, including those from Japan, strongly recommend the use of ACEIs or ARBs in hypertensive patients with CKD. However, few trials have examined the effects of a RAS inhibitor on the progression of kidney disease in Japanese patients with hypertension and advanced, predialysis CKD. Given that Japanese and Western patients may have different responses to therapeutic agents, clinical data from other countries are not necessarily applicable to Japanese patients. Understanding the measures to prevent disease progression is an important goal for Japanese CKD patients. Among RAS inhibitors, ARBs are preferred in Japan because ACEIs cause a dry cough in a high proportion of the Asian population.4 Therefore, the aim of the present study was to examine the add-on effects of one of the ARBs, valsartan, on the course of renal disease progression in Japanese patients with hypertension and advanced CKD.
Methods
Study design
The Kanagawa Valsartan Trial (KVT) was a multicenter, prospective, randomized, open-label study of Japanese hypertensive patients with advanced CKD whose serum creatinine levels were ⩾2.0 mg dl−1. It was designed to evaluate the effect of add-on valsartan on the rate of CKD progression and the incidence of cardiovascular disease. A total of 13 affiliated clinical sites in Kanagawa prefecture, Japan, contributed to this study. All attending physicians were qualified nephrologists.
The enrollment visit was followed by a 4-week run-in screening period during which all ARBs were discontinued and, if necessary, patients were switched to other antihypertensive drugs to control their hypertension. Blood pressure (BP) was measured twice, and urine and blood specimens were obtained for measurements of serum creatinine and urinary protein. Eligible patients were examined for up to 36 months after the start of the trial.
There are no epidemiological data concerning the prognosis of CKD patients with a serum creatinine level ⩾2.0 mg dl−1. However, our preliminary data suggested that the 3-year incidence of ESRD or a doubling of the serum creatinine level would be more than 50% in such patients. A 30% reduction in renal outcomes was assumed among those assigned to valsartan add-on treatment. On this basis, it was estimated that with a study sample of at least 339 patients (170 in each group), the study would have 80% power to detect a clinically important difference in renal outcome between the two groups over a 3-year follow-up period, with a two-sided, type 1 error rate of 5%. Accordingly, the target for enrollment was 400 patients.
The trial was overseen by independent executive, steering, and safety and event committees. The executive committee oversaw the study, including the design, and had full access to all of the data at the end of the study as well as the final responsibility for the decision to submit the manuscript for publication. The steering committee oversaw the conduct of the trial and was responsible for data management and statistical analysis, with confirmation by biostatisticians. The safety and event committee regularly monitored adverse events and relevant clinical events. All outcomes were also reviewed and adjudicated by the safety and event committee, whose members were unaware of the treatment assignments. The authors had complete control over the analysis and interpretation of the results, the writing of the manuscript and the decision to submit it for publication, and they vouched for the accuracy and completeness of the reported data, as well as the fidelity of the reported study to the protocol (KVT study organization and investigators have been posted on Hypertension Research’s website as Supplementary Information).
The study protocol was registered in Clinical Trials.gov (NCT00190580). Good clinical practice guidelines in accordance with the Declaration of Helsinki were followed. The study was approved by the institutional review board at each site, and all patients provided written, informed consent.
Study participants
The trial involved male and female Japanese hypertensive patients aged ⩾20 years. Hypertension was defined as a BP >130/85 mm Hg on two consecutive measurements at the office during the screening period. Patients were eligible for enrollment if their serum creatinine concentration was ⩾2.0 mg dl−1 during the screening period.
The exclusion criteria were ESRD with RRT, polycystic kidney disease, collagen disease and malignant or accelerated hypertension.
Randomization and treatment assignments
During the 4-week screening phase, each patient’s eligibility for the study was established. In patients who had used ARBs before the start of the study, ARBs were suspended during the 4-week screening phase. Eligible patients were randomly assigned to either conventional therapy with valsartan (the valsartan add-on group) or conventional therapy without ARBs (the control group). Conventional treatment consisted of lifestyle modification, diet therapy including salt and protein restriction, blood glucose control in patients with diabetes, lipid control in patients with dyslipidemia, control of anemia and serum potassium, calcium and phosphate levels and blood pressure control as indicated below. Nonpharmacologic and pharmacologic approaches to treatment of hypertension and CKD were recommended according to the guidelines.5, 6
A concealed randomization scheme was generated by computer at the clinical trials center. Patients were divided into three groups according to their baseline serum creatinine level and urinary protein excretion, determined by the protein/creatinine ratio of a spot urine sample. The three groups of serum creatinine levels were classified as follows: group I, ⩾2.0 to <3.0 mg dl−1; group II, ⩾3.0 to <4.0 mg dl−1; and group III ⩾4.0 mg dl−1. The three groups were classified by urinary protein levels as follows: group I, <1.0 g gCr−1; group II, ⩾1.0 to <3.5 g gCr−1; and group III, ⩾3.5 g gCr−1. The randomization was stratified by centers, genders, serum creatinine groups and urinary protein groups to maintain balance between the two groups.
The initial target BP in both groups was <130/85 mm Hg according to the guidelines of the Japanese Hypertension Society 2000.5 This was changed to <130/80 mm Hg based on the revised guidelines of the Japanese Hypertension Society 2004 after 1 January 2004.6 To achieve the target BP, patients in the valsartan add-on group were initially given 40 mg of valsartan orally, once daily in the morning, and titrated up by 40 mg at 4- to 8-week intervals according to changes in the blood pressure, proteinuria, renal function and serum potassium level. A maximum of 160 mg per day of valsartan was permitted. If BP control was not achieved at this dosage, additional antihypertensive agents were added. In the control group, BP control was achieved by either an increase in the dose of their existing treatment or additional treatment other than an ARB, as needed. Antihypertensive agents including ACEIs were allowed in both groups to help patients achieve and maintain their target BP, although no ARB other than valsartan in the valsartan add-on group was permitted, and no ARB in the control group was permitted.
At enrollment, the patients’ baseline characteristics, including sex, age, height, weight, symptoms and signs, risk factors for cardiovascular disease (smoking, dyslipidemia, diabetes mellitus and previous cardiovascular events) and diagnosis of primary disease of CKD with or without kidney biopsy were recorded. Patients were seen every 2–4 weeks, or at least every 3 months, for up to 3 years. At every visit, an attending physician took standard BP measurements with the patient at rest in a sitting position using a validated mercury sphygmomanometer. The timing of BP measurements was free in relation to the intake of medication. Blood and urine samples were obtained at a minimum of 3-month intervals during the trial. Clinical laboratory tests included urinalysis (protein, creatinine) and blood chemistry (creatinine, sodium, potassium, total cholesterol, triglycerides, low-density lipoprotein cholesterol and high-density lipoprotein cholesterol). The glomerular filtration rate was estimated using the equation of the Japanese Society of Nephrology7 and categorized using the KDOQI (Kidney Disease Outcomes Quality Initiative) stages.8
End points
The primary end point was the course of renal function, that is, the change in serum creatinine levels during the study. The estimated glomerular filtration rate (eGFR) was also used to estimate the course of renal function. Participants who reached the two prespecified clinical end points, that is, ESRD with dialysis and renal transplantation needed or death, were treated as censored. Therefore, the course of renal function was also evaluated by the mean annual serum creatinine slope and the mean annual rate of decline in eGFR from baseline to the end of observation or the two specified end points.
Prespecified secondary end points included change in urinary protein levels; renal events, such as the doubling of serum creatinine levels, initiation of maintenance dialysis therapy or renal transplantation; cardiovascular events, such as the composite of cardiovascular complications including admission because of stroke, ischemic heart disease, heart failure and other vascular disease; and death from any cause. Any single doubling of the serum creatinine level required confirmation by one additional positive result from a separate serial test.
Statistical analysis
All analyses were performed according to the intention-to-treat principle. For the comparison of the control and valsartan add-on groups, the unpaired Student’s t-test, Mann–Whitney U-test and the χ2-test were used to compare findings, as appropriate. In the analysis of the differences among treatment groups in the overall changes of systolic and diastolic BP, serum creatinine, eGFR and proteinuria, a generalized linear mixed model was used. The cumulative event curves until the first occurring prespecified events were estimated with the Kaplan–Meier procedure and the log-rank test. Multivariate Cox regression analysis was used to estimate the hazard ratios and 95% confidence intervals for the addition of valsartan compared with conventional treatment with adjustment for baseline covariates. All statistical analyses were performed using SPSS software for Windows, version 16 (SPSS Institute, Chicago, IL, USA). The values are expressed as the means±s.d. for normally distributed data and the medians (interquartile range) for nonnormally distributed data unless otherwise indicated. Differences with P<0.05 were considered significant in all analyses.
Results
Patient population
A total of 312 patients were enrolled between May 2003 and April 2007. During the 4-week run-in screening period, 9 patients were excluded for failure to follow-up (patients did not visit the clinic because they moved or for unknown reasons) or protocol violation, including 2 patients with polycystic kidney disease; thus, 303 patients underwent randomization. After randomization, 10 patients, 6 in the control group and 4 in the valsartan add-on group, could not be followed-up: 3 withdrew consent, 5 failed to follow-up and 2 patients moved. Therefore, 293 patients were included in the analysis. The last evaluation of patients without ESRD or death was performed during the 3 months before April 2008. Data were censored on 31 May 2008. The median follow-up period was 23.8 months (range: 0.9–36.0 months).
The baseline characteristics for each treatment group are shown in Table 1. The mean age of the patients was 64.1±12.2 years, with 72% men. The mean serum creatinine level was 3.20±1.14 mg dl−1, and the mean eGFR was 17.3±6.0 ml min−1 per 1.73 m2. CKD was stage 3 in 2 patients, stage 4 in 174 patients and stage 5 in 117 patients. The mean BP was 142.9±16.9/79.0±10.9 mm Hg. The median urinary protein level was 1.65 (0.70–3.33) g gCr−1, and 11.3% of patients had a urinary protein level <0.3 g gCr−1. There were no significant differences in the baseline clinical characteristics between groups.
The main primary diseases were diabetic nephropathy (33.1%); hypertensive nephrosclerosis (18.8%); IgA nephropathy (9.2%); other glomerulonephritis including primary, secondary and hereditary glomerulonephritis (15.4%); interstitial nephritis (1.7%); others (1.7%); and unknown origin (20.1%). The occurrence of primary diseases did not differ significantly between groups. Of the 293 patients, 38 (13.0%) had been diagnosed by renal biopsy.
The types of medications taken by the participants are shown in Table 2. During the screening period, no patients took ARBs, 120 (41.0%) took ACEIs, 239 (79.9%) took calcium channel blockers and 52 (17.7%) had been prescribed statins.
Antihypertensive agents and BP control
At the end of observation, 88.7% of the valsartan add-on group and 12.0% of the control group took an ARB (Table 2). In the valsartan add-on group, the average dose of valsartan was 75.6±44.2 mg day−1 (median 80.0 mg day−1, range 20–160 mg day−1). In the control group, the proportion of patients taking ACEIs, α-blockers, β-blockers and loop diuretics increased at the end of observation. In the valsartan add-on group, the proportion of patients taking loop diuretics increased, but that of patients taking ACEIs decreased at the end of observation.
The BP measurements for each group are shown in Figure 1a. BP values in both groups decreased after starting the trial. Changes in BP from the screening period to the follow-up period were from 142.1±18.1/77.9±11.0 mm Hg to 134.5±16.6/74.4±10.2 mm Hg in the control group and from 143.6±15.7/80.1±10.7 mm Hg to 133.2±17.1/74.8±10.5 mm Hg in the valsartan add-on group. Over the course of the study, there was no significant difference in either systolic or diastolic BP values between groups.
Course of renal function
There were gradual increases in serum creatinine levels and gradual decreases in eGFR during the follow-up period in both groups (Figures 1b and c). There were no significant between-group differences in the course of serum creatinine and eGFR changes. However, the mean annual serum creatinine slope from baseline to the end of observation or the two clinical end points was significantly lower in the valsartan add-on group (1.62±1.97 mg dl−1 per year) than in the control group (2.60±4.16 mg dl−1 per year; P=0.008). The mean annual rate of decline in eGFR tended to be lower in the valsartan add-on group (3.66±4.48 ml min−1 per 1.73 m2 per year) than in the control group (5.20±10.27 ml min−1 per 1.73 m2 per year), but the difference was not significant.
Changes in urinary protein
The amounts of urinary protein declined gradually during the follow-up period in both groups (Figure 1d). Levels of proteinuria were log-transformed before analysis to reduce skewness, and there were no significant between-group differences in the changes in urinary protein levels.
Renal and cardiovascular events
The pre-specified events for patients in both groups are summarized in Table 3. The number of patients who developed ESRD was 106 (36.2%). Mean serum creatinine levels at the time of initiation of maintenance RRT were 9.05±2.7 mg dl−1 in the control group and 9.06±3.14 mg dl−1 in the valsartan add-on group, with no significant differences between groups. The proportion of patients who reached the cardiovascular end points was very low: 9 (6.3%) in the control group and 9 (6.0%) in the valsartan add-on group. The rate of death from any cause was also very low, with only three deaths occurring (1.0%), two from heart failure and one from ischemic colitis.
Because there were small numbers of cardiovascular events, the intention was to explore the effect of valsartan on renal events. The proportions of patients in each group who reached the renal end point, defined as a doubling of the serum creatinine level or ESRD, are shown in Figure 2. There was a significant decrease in the renal event rate in the valsartan add-on group compared with that in the control group (P=0.007). Renal events were reached in 70 (48.6%) patients in the control group and 53 (35.6%) patients in the valsartan add-on group. Patients in the valsartan add-on group had a 38.3% unadjusted relative risk reduction of reaching the renal end point (95% confidence interval: 11.9–56.9%; P=0.008). After adjustment for baseline variables, including sex, age, body mass index, coexistence of diabetes mellitus, ischemic heart disease, dyslipidemia, systolic BP (⩾140 mm Hg), serum creatinine group and urinary protein group, the decrease in risk with the addition of valsartan remained unchanged (42.6, 95% confidence interval: 16.4–60.6%; P=0.004; Table 4). Other significant baseline factors that correlated with renal events were serum creatinine, urinary protein and systolic BP level.
Adverse events
In addition to the three deaths, a small number of adverse events were observed (Table 3). The number of patients in whom adverse events occurred during the study period was almost the same in both groups. There were no serious adverse events that required stopping the study.
Discussion
Whether the addition of valsartan, at a flexible dose according to BP, prevents the progression of CKD better than conventional treatment without an ARB was examined in Japanese patients with hypertension and advanced CKD. Although there was no difference in the course of renal function between the two study groups, the rate of renal events was significantly decreased in the valsartan add-on group.
In this study, ∼36% of participants had progressed to ESRD during the study. Because patients with higher serum creatinine levels had withdrawn earlier from the study, it is likely that the changes in serum creatinine or eGFR do not accurately reflect the course of renal function. Therefore, the mean annual serum creatinine slope from the baseline to the last measurement was also examined in each patient. The results showed that the mean annual slope of serum creatinine was significantly lower in the valsartan add-on group than in the control group. The mean annual rate of decline in eGFR was also lower in the valsartan add-on group. Thus, the lack of difference in the course of renal function is possibly due to survival bias. Furthermore, no difference in the course of serum creatinine between groups might reflect the favorable effects of the addition of valsartan on the course of renal function because larger numbers of patients in the control group with high serum creatinine reached ESRD earlier and were excluded from subsequent analyses.
The validity of the above assumption is verified by the finding that there was a 43% decrease in the adjusted hazard ratio of the rate of renal events, defined as a doubling of serum creatinine or development of ESRD, in the valsartan add-on group compared with the conventional treatment group without ARB. Numerous randomized clinical trials in Western countries have demonstrated the benefit of ACEIs or ARBs in slowing CKD progression in patients with diabetes and non-diabetes.9, 10, 11, 12 The reduction of renal events in the present study was comparable with these previous studies. Therefore, the present study indicates that the addition of an ARB, valsartan, also slows renal disease progression to ESRD in Japanese patients with advanced CKD.
In addition to the add-on valsartan, levels of BP, serum creatinine and proteinuria were also significant factors influencing the progression of CKD in the present study. There is growing evidence that the major risk factors for renal disease progression are levels of BP, proteinuria and GFR.13, 14, 15, 16, 17, 18 In addition, it is well known that small changes in BP during the course of a study can significantly affect the rate of CKD progression.15 BP levels were well controlled and remained similar in both groups throughout this trial.
With respect to proteinuria, previous studies demonstrated that RAS inhibitors provide superior renoprotection in subjects with high urinary protein excretion.2, 14, 18 In the present study, the proportion of patients with urinary protein <0.3 g day−1 was only 11.3%. Therefore, it is likely that the significant reduction of renal events observed in the present study was because of the high proportion of participants with overt proteinuria. However, there were no between-group differences in urinary protein levels during the trial. Previous studies have demonstrated that the degree of reduction in proteinuria parallels the reduction of renal events.9, 17, 18 Many studies have confirmed the association between the severity of proteinuria and the progression of CKD.9, 18 Therefore, in the present study, a larger number of patients with a high level of proteinuria in the control group might have reached ESRD earlier and been excluded from subsequent analyses of proteinuria. As a result, proteinuria reduction with ARBs may be masked. Further analyses are needed to determine the renal protective effect of valsartan and the relationship between the reduction of urinary protein and the progression of kidney disease.
CKD patients are at greater risk for adverse cardiovascular events than developing ESRD.19 The rates of cardiovascular events in the present study were lower (∼4% or 2.9 cases per 1000 person-years) than previous studies involving patients with advanced CKD, such as the RENAAL study and IDNT. In these studies, the rates were higher by a factor of ∼20 or 60 cases per 1000 person-years.11, 12 The reason for this discrepancy is likely a result of the Japanese population generally exhibiting a lower incidence of cardiovascular disease compared with Western countries.20 Because event rates for cardiovascular disease and death were generally low in the present study, conclusions about the effect of ARB add-on therapy on these outcomes cannot be definitive.
Notably, approximately half of the participants in the conventional group and approximately a quarter of those in the valsartan add-on group were taking ACEIs in the present study. The recent results regarding combination ACEI and ARB therapy in the ONTARGET report are opposite those of the present study.21 However, the backgrounds of participants differ between the two studies, as the ONTARGET study involved patients with almost normal GFR and without massive proteinuria. In addition, the manner of dose escalation was different. In the ONTARGET study, the dose was increased on a regular basis with a predetermined fixed amount. On the other hand, in the present study, valsartan was started from half of the usual dose and increased gradually, adjusted in an appropriate manner according to the patient’s condition, considering changes in BP, proteinuria, renal function and serum potassium levels by well-trained nephrologists. It seems mandatory in the management of CKD to decide the dose and dose escalation of antihypertensive drugs, including ARBs, according to the condition and course of each individual patient, with close monitoring of serum creatinine, serum potassium, BP and urinary protein. Although there were higher incidences of hypotension and hyperkalemia in the valsartan add-on group, the overall incidence of adverse events was very small. Therefore, an ARB can be safely used in hypertensive patients with advanced CKD under careful observation of the condition and clinical course of the patients.
Recently, several studies reported differences in renal effects between subtypes of calcium channel blockers.22, 23, 24 In particular, N/L-type and T/L-type calcium channel blockers with or without RAS inhibitors have favorable effects on the kidney in patients with CKD, including reduction of proteinuria. In this study, 80% of participants took various calcium channel blockers. Therefore, further study is necessary to elucidate the differences of effects between subtypes of calcium channel blockers and the renoprotective effects of valsartan in patients with advanced predialysis CKD.
This study had several limitations. First, as this study was not a double-blind study, the results may be affected by unexpected confounders. Second, although all reported events were checked by the safety and clinical event committee, all events were reported by the attending physician, and hence minor side effects were likely missed. However, the finding of no difference in mean serum creatinine levels at the time of the initiation of RRT between the two groups supports the notion that the initiation of RRT was performed objectively. Third, the present study was not designed to define the optimal target BP with antihypertensive treatment in patients with advanced CKD. Further studies are needed to determine the optimal BP goal for advanced CKD. Finally, this study was performed at institutions with well-trained nephrologists and highly regarded programs for patients with CKD. Therefore, generalization of the results of the present study to patients managed by general physicians is difficult. Consultation with nephrologists is strongly recommended for the management of patients with advanced predialysis CKD.
This study demonstrated that the addition of an ARB, valsartan, to conventional treatment slowed the rate of renal function decline and delayed the need for RRT. ARBs might exert superior renoprotection compared with conventional treatment alone in Japanese hypertensive patients with advanced CKD.
References
Nakai S, Iseki K, Itami N, Ogata S, Kazama JJ, Kimata N, Shigematsu T, Shinoda T, Shoji T, Suzuki K, Taniguchi M, Tsuchida K, Nakamoto H, Nishi H, Hashimoto S, Hasegawa T, Hanafusa N, Hamano T, Fujii N, Masakane I, Marubayashi S, Morita O, Yamagata K, Wakai K, Wada A, Watanabe Y, Tsubakihara Y . Overview of regular dialysis treatment in Japan (as of 31 December 2009). Ther Apher Dial 2012; 16: 11–53.
Jafar TH, Schmid CH, Landa M, Giatras I, Toto R, Remuzzi G, Maschio G, Brenner BM, Kamper A, Zucchelli P, Becker G, Himmelmann A, Bannister K, Landais P, Shahinfar S, de Jong PE, de Zeeuw D, Lau J, Levey AS . Angiotensin-converting enzyme inhibitors and progression of nondiabetic renal disease. A meta-analysis of patient-level data. Ann Intern Med 2001; 135: 73–87.
Strippoli GF, Bonifati C, Craig M, Navaneethan SD, Craig JC . Angiotensin converting enzyme inhibitors and angiotensin II receptor antagonists for preventing the progression of diabetic kidney disease. Cochrane Database Syst Rev 2006; 4 : CD006257.
Woo KS, Nicholls MG . High prevalence of persistent cough with angiotensin converting enzyme inhibitors in Chinese. Br J Clin Pharmacol 1995; 40: 141–144.
Japanese Society of Hypertension Guidelines Subcommittee for the Management of Hypertension. Guidelines for the management of hypertension for general practitioners. Hypertens Res 2001; 24: 613–634.
Japanese Society of Hypertension. Japanese Society of Hypertension guidelines for the management of hypertension (JSH 2004). Hypertens Res 2006; 29 (Suppl): S1–S105.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A . Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39: S1–S266.
Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. The GISEN group (Gruppo Italiano di Studi Epidemiologici in Nefrologia). Lancet 1997; 349: 1857–1863.
Ruggenenti P, Perna A, Gherardi G, Garini G, Zoccali C, Salvadori M, Scolari F, Schena FP, Remuzzi G . Renoprotective properties of ACE-inhibition in non-diabetic nephropathies with non-nephrotic proteinuria. Lancet 1999; 354: 359–364.
Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S, RENAAL Study Investigators. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345: 861–869.
Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I, Collaborative Study Group. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001; 345: 851–860.
Shulman NB, Ford CE, Hall WD, Blaufox MD, Simon D, Langford HG, Schneider KA . Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the hypertension detection and follow-up program. The Hypertension Detection and Follow-Up Program Cooperative Group. Hypertension 1989; 13: I80–93.
Peterson JC, Adler S, Burkart JM, Greene T, Hebert LA, Hunsicker LG, King AJ, Klahr S, Massry SG, Seifter JL . Blood pressure control, proteinuria, and the progression of renal disease. The Modification of Diet in Renal Disease Study. Ann Intern Med 1995; 123: 754–762.
Bakris GL, Weir MR, Shanifar S, Zhang Z, Douglas J, van Dijk DJ, Brenner BM, RENAAL Study Group. Effects of blood pressure level on progression of diabetic nephropathy: results from the RENAAL study. Arch Intern Med 2003; 163: 1555–1565.
Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, de Zeeuw D, Shahinfar S, Toto R, Levey AS, AIPRD Study Group. Progression of chronic kidney disease: the role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: a patient-level meta-analysis. Ann Intern Med 2003; 139: 244–252.
de Zeeuw D, Remuzzi G, Parving HH, Keane WF, Zhang Z, Shahinfar S, Snapinn S, Cooper ME, Mitch WE, Brenner BM . Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: lessons from RENAAL. Kidney Int 2004; 65: 2309–2320.
Atkins RC, Briganti EM, Lewis JB, Hunsicker LG, Braden G, Champion de Crespigny PJ, DeFerrari G, Drury P, Locatelli F, Wiegmann TB, Lewis EJ . Proteinuria reduction and progression to renal failure in patients with type 2 diabetes mellitus and overt nephropathy. Am J Kidney Dis 2005; 45: 281–287.
Keith DS, Nichols GA, Gullion CM, Brown JB, Smith DH . Longitudinal follow-up and outcomes among a population with chronic kidney disease in a large managed care organization. Arch Intern Med 2004; 164: 659–663.
Ueshima H . Explanation for the Japanese paradox: prevention of increase in coronary heart disease and reduction in stroke. J Atheroscler Thromb 2007; 14: 278–286.
ONTARGET Investigators Yusuf S, Teo KK, Pogue J, Dyal L, Copland I, Schumacher H, Dagenais G, Sleight P, Anderson C . Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med 2008; 358: 1547–1559.
Fujita T, Ando K, Nishimura H, Ideura T, Yasuda G, Isshiki M, Takahashi K . Antiproteinuric effect of the calcium channel blocker cilnidipine added to renin-angiotensin inhibition in hypertensive patients with chronic renal disease. Kidney Int 2007; 72: 1543–1549.
Abe M, Okada K, Maruyama T, Maruyama N, Matsumoto K . Comparison of the antiproteinuric effects of the calcium channel blockers benidipine and amlodipine administered in combination with angiotensin receptor blockers to hypertensive patients with stage 3-5 chronic kidney disease. Hypertens Res 2009; 32: 270–275.
Konoshita T, Makino Y, Kimura T, Fujii M, Wakahara S, Arakawa K, Inoki I, Nakamura H, Miyamori I . A new-generation N/L-type calcium channel blocker leads to less activation of the renin-angiotensin system compared with conventional L type calcium channel blocker. J Hypertens 2010; 28: 2156–2160.
Acknowledgements
We thank Kazuko Ueshima for her excellent support as an executive assistant.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Yasuda, T., Endoh, M., Suzuki, D. et al. Effects of valsartan on progression of kidney disease in Japanese hypertensive patients with advanced, predialysis, chronic kidney disease: Kanagawa Valsartan Trial (KVT). Hypertens Res 36, 240–246 (2013). https://doi.org/10.1038/hr.2012.183
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.183
Keywords
This article is cited by
-
Treatments for Chronic Kidney Disease: A Systematic Literature Review of Randomized Controlled Trials
Advances in Therapy (2022)
-
The Different Therapeutic Choices with ARBs. Which One to Give? When? Why?
American Journal of Cardiovascular Drugs (2016)
-
Management of hypertension in chronic kidney disease
Nature Reviews Nephrology (2015)