Abstract
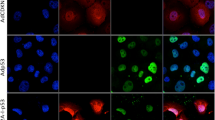
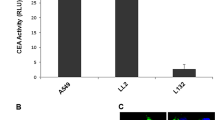
The principle of promoter-targeted gene delivery was used to direct the expression of reporter genes and inducible caspases to Cox-2-overexpressing cancer cells. The polycation poly(ethylenimine) was used in unmodified form to nonvirally deliver genes into cells, and targeting was achieved at the transcriptional level. Results demonstrated that reporter expression was reduced by an average of 89.8% in normal cells and cell lines not overexpressing Cox-2 when the strong cytomegalovirus promoter was replaced with the human Cox-2 promoter in delivered plasmids. Cocultures of normal and Cox-2-overexpressing cancer cells showed less than 0.5% reporter expression in normal fibroblast cells but over 35% reporter expression in PC3 prostate cancer cells. This targeting method was then used to direct the expression of inducible forms of caspases 3 and 9 to Cox-2-overexpressing cancer cells of the bladder and prostate. Following activation of the resulting caspase pro-forms, cells underwent apoptosis as evidenced by DNA fragmentation and cytoskeletal degradation. This result was also observed in cells resistant to apoptosis in terms of TNF-α initiation. Such directed apoptosis could eventually serve as a treatment for an entire class of Cox-2-overexpressing carcinomas.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Rubin J et al. Phase I study of immunotherapy of hepatic metastases of colorectal carcinoma by direct gene transfer of an allogeneic histocompatibility antigen, HLA-B7. Gene Therapy 1997; 4: 419–425.
Vogelzang NJ, Lestingi TM, Sudakoff G, Kradjian SA . Phase I study of immunotherapy of metastatic renal cell carcinoma by direct gene transfer into metastatic lesions. Hum Gene Ther 1994; 5: 1357–1370.
Hood JD et al. Tumor regression by targeted gene delivery to the neovasculature. Science 2002; 296: 2404–2407.
Watson AJ . Chemopreventive effects of NSAIDs against colorectal cancer: regulation of apoptosis and mitosis by COX-1 and COX-2. Histol Histopathol 1998; 13: 591–597.
Godbey WT et al. Poly(ethylenimine)-mediated transfection: a new paradigm for gene delivery. J Biomed Mater Res 2000; 51: 321–218.
Huppertz B, Frank HG, Kaufmann P . The apoptosis cascade – morphological and immunohistochemical methods for its visualization. Anat Embryol (Berlin) 1999; 200: 1–18.
Godbey WT, Wu KK, Mikos AG . Tracking the intracellular path of poly(ethylenimine)/DNA complexes for gene delivery. Proc Natl Acad Sci USA 1999; 96: 5177–5181.
Zelphati O, Szoka Jr FC . Mechanism of oligonucleotide release from cationic liposomes. Proc Natl Acad Sci USA 1996; 93: 11493–11498.
Bieber T et al. Intracellular route and transcriptional competence of polyethylenimine–DNA complexes. J Control Release 2002; 82: 441.
Davidenkova EF . Current status of the problem of the treatment and prevention of hereditary diseases. Zh Nevropatol Psikhiatr im SS Korsakova 1982; 82: 9–17.
Matthay KK, Heath TD, Papahadjopoulos D . Specific enhancement of drug delivery to AKR lymphoma by antibody-targeted small unilamellar vesicles. Cancer Res 1984; 44: 1880–1886.
Morita A et al. Development of a Langerhans cell-targeted gene therapy format using a dendritic cell-specific promoter. Gene Therapy 2001; 8: 1729–1737.
Bao R, Selvakumaran M, Hamilton TC . Targeted gene therapy of ovarian cancer using an ovarian-specific promoter. Gynecol Oncol 2002; 84: 228–234.
Maxwell IH, Glode LM, Maxwell F . Expression of the diphtheria toxin A-chain coding sequence under the control of promoters and enhancers from immunoglobulin genes as a means of directing toxicity to B-lymphoid cells. Cancer Res 1991; 51: 4299–4304.
DuBois RN et al. G1 delay in cells overexpressing prostaglandin endoperoxide synthase-2. Cancer Res 1996; 56: 733–737.
Shamma A et al. Up-regulation of cyclooxygenase-2 in squamous carcinogenesis of the esophagus. Clin Cancer Res 2000; 6: 1229–1238.
Molina MA et al. Increased cyclooxygenase-2 expression in human pancreatic carcinomas and cell lines: growth inhibition by nonsteroidal anti-inflammatory drugs. Cancer Res 1999; 59: 4356–4362.
Battu S, Rigaud M, Beneytout JL . Resistance to apoptosis and cyclooxygenase-2 expression in a human adenocarcinoma cell line HT29 CL.19A. Anticancer Res 1998; 18: 3579–3583.
Subbaramaiah K et al. Transcription of cyclooxygenase-2 is enhanced in transformed mammary epithelial cells. Cancer Res 1996; 56: 4424–4429.
Kamijo T, Sato T, Nagatomi Y, Kitamura T . Induction of apoptosis by cyclooxygenase-2 inhibitors in prostate cancer cell lines. Int J Urol 2001; 8: S35–S39.
Bostrom PJ et al. Expression of cyclooxygenase-1 and -2 in urinary bladder carcinomas in vivo and in vitro and prostaglandin E2 synthesis in cultured bladder cancer cells. Pathology 2001; 33: 469–474.
Hwang D, Scollard D, Byrne J, Levine E . Expression of cyclooxygenase-1 and cyclooxygenase-2 in human breast cancer. J Natl Cancer Inst 1998; 90: 455–460.
Yoshimura R et al. Expression of cyclooxygenase-2 in patients with bladder carcinoma. J Urol 2001; 165: 1468–1472.
Howe LR, Subbaramaiah K, Brown AM, Dannenberg AJ . Cyclooxygenase-2: a target for the prevention and treatment of breast cancer. Endocr Relat Cancer 2001; 8: 97–114.
Haq R, Zanke B . Inhibition of apoptotic signaling pathways in cancer cells as a mechanism of chemotherapy resistance. Cancer Metast Rev 1998; 17: 233–239.
Elder DJ, Halton DE, Hague A, Paraskeva C . Induction of apoptotic cell death in human colorectal carcinoma cell lines by a cyclooxygenase-2 (COX-2)-selective nonsteroidal anti-inflammatory drug: independence from COX-2 protein expression. Clin Cancer Res 1997; 3: 1679–1683.
Katsen AD, Vollmar B, Mestres-Ventura P, Menger MD . Cell surface and nuclear changes during TNF-alpha-induced apoptosis in WEHI 164 murine fibrosarcoma cells. A correlative light, scanning, and transmission electron microscopical study. Virchows Arch 1998; 433: 75–83.
Xie X et al. Adenovirus-mediated tissue-targeted expression of a caspase-9-based artificial death switch for the treatment of prostate cancer. Cancer Res 2001; 61: 6795–6804.
Shariat SF et al. Adenovirus-mediated transfer of inducible caspases: a novel ‘death switch’ gene therapeutic approach to prostate cancer. Cancer Res 2001; 61: 2562–2571.
Yamamoto M et al. Characterization of the cyclooxygenase-2 promoter in an adenoviral vector and its application for the mitigation of toxicity in suicide gene therapy of gastrointestinal cancers. Mol Ther 2001; 3: 385–394.
Tazawa R, Xu XM, Wu KK, Wang LH . Characterization of the genomic structure, chromosomal location and promoter of human prostaglandin H synthase-2 gene. Biochem Biophys Res Commun 1994; 203: 190–199.
Godbey WT, Wu KK, Hirasaki GJ, Mikos AG . Improved packing of poly(ethylenimine)/DNA complexes increases transfection efficiency. Gene Therapy 1999; 6: 1380–1388.
Acknowledgements
We thank Shay Soker, PhD for scientific discussions. Funding for this work was provided by the National Institutes of Health (R01-DK57260).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Godbey, W., Atala, A. Directed apoptosis in Cox-2-overexpressing cancer cells through expression-targeted gene delivery. Gene Ther 10, 1519–1527 (2003). https://doi.org/10.1038/sj.gt.3302012
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.gt.3302012
Keywords
This article is cited by
-
Preclinical evaluation of a gene therapy treatment for transitional cell carcinoma
Cancer Gene Therapy (2011)
-
Comparison of Caspase Genes for the Induction of Apoptosis Following Gene Delivery
Molecular Biotechnology (2009)
-
Expression-targeted gene therapy for the treatment of transitional cell carcinoma
Cancer Gene Therapy (2008)