Abstract
Purpose:
As genetic counseling and testing become more fully integrated into clinical care, alternative delivery models are increasingly prominent. This study examines predictors of genetic testing for hereditary breast/ovarian cancer among high-risk women in a randomized trial of in-person versus telephone-based genetic counseling.
Methods:
Methods include multivariable logistic regression and interaction analyses.
Results:
Of the 669 participants, 600 completed counseling and 523 received test results. As previously reported, participants randomized to telephone counseling were significantly less likely to be tested. In intention-to-treat analyses, completion of counseling and testing was associated with: race/ethnicity (odds ratio (OR) = 1.96, 95% confidence interval (CI): 1.20–3.20), perceived stress (OR = 0.89, 95% CI: 0.81–0.98), knowledge (OR = 1.12, 95% CI: 1.02–1.23), and randomization group (OR = 1.48, 95% CI: 1.01–2.16). Further, race/ethnicity moderated the association between randomization group and testing; minority women receiving telephone counseling were least likely to complete testing.
Conclusion:
Evidence for logistical and communication-based explanations for this interaction is presented. The overall increased access made possible with telephone genetic counseling should be considered in light of the possibility that this may also lead to lower rates of testing among high-risk minority women. Additional care should be taken to assess and address potential barriers when services are delivered by telephone.
Genet Med 17 6, 467–475.
Similar content being viewed by others
Introduction
Genetic testing of the BRCA1 and BRCA2 (BRCA1/2) genes has become standard of care for women at risk for hereditary breast and ovarian cancer (HBOC). Although comprehensive genetic counseling is recommended,1,2 this service is not always accessible given the small size and unequal distribution of the genetic counseling workforce.3 Thus, in practice, this need may be addressed by having non-geneticist physicians, such as the patient’s obstetrician/gynecologist, primary care doctor, surgeon, or oncologist order BRCA1/2 testing. The ordering of BRCA1/2 testing by non-genetics professionals may or may not be accompanied by adequate genetic counseling and result interpretation.4,5 However, an increasingly common alternative approach to service delivery is for genetics professionals to deliver pretest and/or posttest genetic counseling by telephone.6,7,8 Despite the increasing use of telephone counseling, little is known about how telephone delivery of genetic services impacts the receipt of counseling or uptake of testing.
We recently completed a randomized noninferiority trial that demonstrated that delivering genetic counseling via telephone (TC) led to outcomes that were not inferior to standard in-person genetic counseling (usual care (UC)) for HBOC. Specifically, TC was not inferior to UC regarding knowledge, satisfaction, decisional conflict, quality of life, and distress.9 In addition, TC yielded a cost savings of $114 per patient counseled compared with UC.9 Although concerns exist regarding potential limitations of or adverse outcomes related to telemedicine generally10,11 and telephone genetic counseling specifically,12,13 these data support the use of TC as a safe and cost-effective approach to increase access to genetic services for HBOC.9
Notably, however, in this trial we found that women who were randomized to TC were less likely to complete BRCA1/2 testing than women randomized to UC.9 The lower rate of genetic testing for TC participants was replicated in another recent trial comparing TC and in-person genetic counseling.14 There are several plausible explanations for this difference. Because participants who received TC did not have the option of providing DNA for testing immediately after counseling, the built-in delay with TC may have been a barrier to testing. Alternatively, the delay may have allowed increased time for deliberation among TC participants, leading some women to decide not to proceed with testing. Although these structural differences are plausible, it is also possible that unmeasured genetic counseling process differences (e.g., differences in rapport or needs assessment between TC and UC) contributed to this difference.
If telephone delivery of genetic counseling is to be part of the solution to the shortage and uneven distribution of genetics professionals, then a better understanding of how TC impacts uptake of genetic testing is needed. The increasing use of panel-based genetic testing for cancer susceptibility only underscores the need for understanding the factors contributing to counseling and test uptake with alternative delivery models, as greater demand is being placed on the professionals delivering this service. Specifically, identifying factors that contribute to the lower uptake of genetic testing after TC could facilitate improved tailoring and delivery of TC. For example, TC may not be uniformly appropriate for all patients, based on their medical, socio-demographic, or psychological characteristics.
In this report we examined socio-demographic, medical, and psychosocial predictors of genetic testing uptake and we evaluated whether there were patient-related moderators that contributed to lower genetic testing uptake after TC. Specifically, we tested the following moderator variables based on previous literature:15,16 knowledge, numeracy, race/ethnicity, education, perceived and objective mutation risk, and distress. We examined these putative moderators within our intention-to-treat (ITT) and our per-protocol (PP) samples. The ITT population reflects the comparison between UC and TC with respect to both attending genetic counseling and obtaining BRCA1/2 results, whereas the PP analyses reflect a comparison of test uptake after receipt of in-person genetic counseling versus TC.
Materials and Methods
Participants
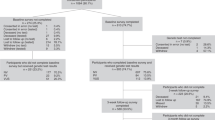
Participants were women who were enrolled in a randomized noninferiority trial comparing standard genetic counseling to telephone-based genetic counseling.9,17 From 2005 to 2012, we enrolled women who were self-referred or physician-referred to the genetic counseling programs at the Lombardi Comprehensive Cancer Center (Washington, DC), Icahn School of Medicine at Mount Sinai (New York, NY), University of Vermont Cancer Center (Burlington, VT), and the Dana Farber Cancer Institute (Boston, MA). Eligible participants were women 21 to 85 years old who sought BRCA1/2 genetic counseling, had not received previous counseling or testing, did not have newly diagnosed or metastatic breast or ovarian cancer, lived within the catchment area of one of our study sites, and agreed to be randomized to telephone versus in-person genetic counseling. As displayed in Figure 1 , of 1,057 potentially eligible women, 669 (63.3%) completed a baseline interview and agreed to be randomized to telephone counseling (n = 335) versus in-person counseling (n = 334). This report focuses on baseline (i.e., prerandomization) predictors of the completion of genetic testing within this trial.
Procedures
Eligible patients completed a precounseling telephone interview with a research assistant to collect demographic, cancer history, and psychosocial information. After the interview, we explained the study, obtained verbal consent, and randomized consenting participants via computer-generated random numbers to either UC or TC. The UC and TC interventions are explained in detail in other reports.9,17 UC participants completed both their initial session and results disclosure session in person. TC participants completed both sessions by telephone. The study was approved by the institutional review boards of the participating sites.
Measures
Socio-demographics. We assessed age, education, marital status, race/ethnicity, employment, and Jewish ancestry. For analysis, we treated age as a continuous variable but created binary variables for education (college graduate versus less than college graduate), marital status (married/partnered versus unmarried/unpartnered), race/ethnicity (non-Hispanic white versus racial/ethnic minority), employment (full-time versus less than full-time), and Jewish ancestry (Jewish versus non-Jewish).
Medical history. We assessed personal and family cancer history to calculate an a priori risk score using BRCAPRO.18 We used BRCAPRO score as a single composite of objective risk rather than using individual measures of personal cancer history and breast and ovarian cancer family history (all of which are components of and highly correlated with BRCAPRO score).
Intentions for risk-reducing surgery. We created a binary variable to reflect baseline intentions for risk-reducing mastectomy or risk-reducing oophorectomy. Participants who reported that they were not considering risk-reducing mastectomy or risk-reducing oophorectomy served as the reference group (n = 353). This group included participants who had already undergone both surgeries (n = 24); participants who had one of the surgeries but were not considering the other (n = 125); and participants who had neither surgery and were not considering either in the future (n = 204). These participants were contrasted with participants who reported that they were considering risk-reducing mastectomy, risk-reducing oophorectomy, or both (n = 316).
Perceived risk of a BRCA mutation. We measured perceived risk with the following 5-point Likert-style item: “In your opinion, how likely is it that you have an altered breast–ovarian cancer gene?” We dichotomized this variable for analysis as “very likely and above” versus “somewhat likely and below” based on response distribution.
Perceived risk of breast cancer and perceived risk of ovarian cancer. We measured perceived risk for breast and ovarian cancer with separate 5-point Likert response items. For both, we dichotomized the responses at “very likely and above” versus “somewhat likely and below” based on response distribution.
Knowledge. We measured BRCA1/2 knowledge with the 27-item Breast Cancer Genetic Counseling Knowledge scale.19 The total score was the number of correct responses. Cronbach’s α for this sample was 0.78.
Numeracy. We measured numeracy with Lipkus’ three-item scale.20 The number of items answered correctly was summed to create a total numeracy score (range 0–3). Cronbach’s α was 0.74.
Decisional conflict. We measured decisional conflict regarding BRCA1/2 testing with the 10-item version of the Decisional Conflict Scale.21 Items are scored on a weighted three-point scale (yes, 0/unsure, 2/no, 4), with higher scores indicating greater decisional conflict. We calculated a total score by multiplying the average item score by 25. Cronbach’s α was 0.82.
Distress. We measured cancer-specific distress with the total score on the 15-item Impact of Event Scale.22 Cronbach’s α was 0.88. We measured global perceived stress with the four-item version of the Perceived Stress Scale.23 Perceived Stress Scale items are rated on a 5-point Likert scale and summed for a total score. Cronbach’s α was 0.69.
Quality of life. We measured quality of life with the Short-Form 12-Item Health Survey.24 The survey has two subscales, the Mental Component Summary and the Physical Component Summary. Higher scores reflect better quality of life. Because of complex scoring procedures, we relied on published internal consistency data for the Short-Form 12-Item Health Survey (Cronbach’s α = 0.86 and 0.87).25
Statistical analyses
We conducted analyses separately for the ITT and PP populations. We used t-tests and χ2 tests to identify bivariate associations with completion of genetic testing in the entire sample (ITT population) and limited to those who completed a genetic counseling session (PP population). To identify independent main effect predictors, we used multiple logistic regression with backward elimination in which we started with all variables with P < 0.10 for bivariate associations with the outcome of interest. To identify variables that modified the association between randomization group and counseling/testing completion, we conducted exploratory analyses of the following potential moderator variables: knowledge, numeracy, race/ethnicity, education level, perceived and objective mutation risk, and distress (Impact of Event Scale and Perceived Stress Scale). For each of these putative moderators, we conducted separate multiple logistic regressions in which we added the main effect term for the moderator (if not already in the final model) and the group by moderator interaction term to the final main effects model. All analyses were conducted using SAS version 9.3 (SAS Institute, Cary, NC).
Results
Sample characteristics
The participants were predominantly non-Hispanic white (82.7%), affected with cancer (65.3% with breast or ovarian cancer), had a college education or more (79.7%), and married (62.3%). Participants had a mean age of 47.7 years (SD = 13.4) and had a mean BRCAPRO risk score of 25.0% (SD = 22.9). The TC and UC groups did not differ significantly on any socio-demographic variables (P > 0.05).
As previously reported, of the 669 participants in the trial, 600 (89.7%) completed an initial genetic counseling session and the TC and UC groups did not differ on genetic counseling participation (UC = 90.4%, TC = 89.0%; P = 0.53).9 Also, as previously reported, 523 participants received genetic testing results, representing 78.2% of all participants and 87.2% of participants who completed an initial genetic counseling session. The TC and UC groups differed significantly on genetic testing uptake within the ITT sample (UC = 81.4% vs. TC = 74.9%; Χ2 (n = 699) = 4.16, df = 1, P = 0.04) and the PP sample (UC = 90.1% vs. TC = 84.2%; Χ2 (n = 600) = 4.57, df = 1, P = 0.03).
Genetic counseling and testing completion: intention-to-treat population
As shown in Table 1 , significant bivariate predictors of completing genetic testing in the full sample were: randomization to UC (X2 = 4.16, degrees of freedom (df) = 1, P = 0.042); higher knowledge (t = 2.80, df = 667, P = 0.005); lower perceived stress (t = 2.29, df = 200.68 (Satterthwaite) P = 0.023); non-Hispanic white race/ethnicity (X2 = 6.48, df = 1, P = 0.011); and higher education (X2 = 5.76, df = 1, P = 0.016). Jewish ancestry (X2 = 3.39, df = 1, P = 0.066) and being married/partnered (X2 = 3.03, df = 1, P = 0.082) were marginally associated with completing genetic counseling and testing.
To identify independent main effect predictors of completing genetic counseling and testing, we included all variables with P < 0.10 for bivariate associations with genetic counseling/testing completion in the initial step of a backward elimination procedure for the logistic regression model. The following variables remained in the final model, indicating that they were independently associated with the completion of BRCA1/2 genetic counseling and testing: non-Hispanic white race/ethnicity (odds ratio (OR) = 1.96, 95% confidence interval (CI): 1.20–3.20), perceived stress (OR = 0.89, 95% CI: 0.81–0.98), knowledge (OR = 1.12, 95% CI: 1.02–1.23) and randomization group (OR = 1.48, 95% CI: 1.01–2.16) ( Table 2 ). Participants randomized to UC, those with higher knowledge, those with lower perceived stress, and non-Hispanic white participants were more likely to complete genetic counseling and BRCA1/2 testing.
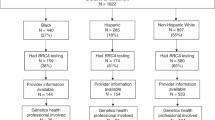
We tested the following patient variables as potential moderators of the association between randomization group and completion of genetic testing: race/ethnicity, knowledge, education, numeracy, distress, and objective and perceived risk for carrying a BRCA1/2 mutation. We tested each of the potential moderators separately by adding their main effect term (if not already in the model) and the randomization group by moderator interaction term to the final main effect model described. Only the group by race/ethnicity interaction approached statistical significance (P = 0.054). As displayed in Figure 2 , within the UC group, 76.2% of minority participants completed counseling and BRCA1/2 testing compared with 82.1% of non-Hispanic white participants (OR = 0.88, 95% CI: 0.40–1.94). Within the TC group, 53.1% of minority participants completed counseling and BRCA1/2 testing compared with 78.9% of non-Hispanic white participants (OR = 0.33, 95% CI: 0.17–0.62).
Genetic testing among those who completed a counseling session: PP population
As displayed in Table 1 , significant bivariate predictors of BRCA1/2 testing among those who completed a genetic counseling visit were: randomization to UC (X2 = 4.57, df = 1, P = 0.033); higher knowledge (t = −2.56, df = 598, P = 0.011); Jewish ancestry (X2 = 3.01, df = 1, P = 0.083); being married/partnered (X2 = 5.14, df = 1, P = 0.023); intentions for risk-reducing surgery (X2 = 4.91, df = 1, P = 0.027); higher objective risk as measured by BRCAPRO score (t = −2.69, df = 598, P = 0.007); and non-Hispanic white race/ethnicity (X2 = 3.38, df = 1, P = 0.066).
We included all variables with P < 0.10 for bivariate associations with genetic testing in the initial step of a backward elimination procedure for the logistic regression model. The following were independently associated with utilization of BRCA1/2 genetic testing: marital status (OR = 1.85, 95% CI: 1.12–3.08), BRCAPRO probability (OR = 1.22, 95% CI: 1.06–1.41), knowledge (OR = 1.13, 95% CI: 1.00–1.27), and randomization group (OR = 1.65, 95% CI: 1.00–2.72) ( Table 2 ). The odds of undergoing BRCA1/2 testing were higher for participants who were married, had higher objective risk, had greater knowledge, and were randomized to UC.
We evaluated the same potential moderator variables as described above. Only the race/ethnicity by group interaction was statistically significant (P = 0.028; data for null interactions not presented). As displayed in Figure 3 , among participants who completed an in-person genetic counseling session, race/ethnicity was not associated with undergoing BRCA1/2 testing. Specifically, 94.2% of minority participants completed BRCA1/2 testing compared with 89.4% of non-Hispanic white participants (OR = 2.75, 95% CI: 0.61–12.50). In contrast, race/ethnicity was significantly associated with testing among participants who completed a TC session with 68.4% of minority participants completing BRCA1/2 testing compared with 87.0% of non-Hispanic white participants (OR = 0.41, 95% CI: 0.18–0.92).
Discussion
The goal of this report was to better understand the lower rate of genetic testing completion among women who received telephone-based BRCA1/2 counseling compared with women who received standard in-person counseling. We examined this question within our ITT and PP samples. It is particularly important to evaluate this question in both samples because the ITT population included all randomized participants regardless of whether they completed a genetic counseling session and therefore reflects the comparison between UC and TC with respect to both attending genetic counseling and obtaining BRCA1/2. In contrast, the PP analyses were limited to participants who completed a genetic counseling session as assigned, therefore reflecting a comparison of test uptake after receipt of in-person versus telephone genetic counseling.
Within the ITT population, independent predictors of genetic testing were randomization group, race/ethnicity, perceived stress, and knowledge. Within the PP population, independent predictors were randomization group, knowledge, marital status, and objective mutation risk. The fact that knowledge was a predictor in both populations suggests that knowledge before counseling may be a facilitator of attending counseling and of choosing to be tested after counseling. Knowledge did not interact with group assignment in either analysis. Similarly, neither education nor numeracy interacted with group assignment, indicating that the impact of previous knowledge, education, and numeracy were comparable for in-person and telephone counseling.
Predictors that differed in the ITT and PP populations included objective risk, perceived stress, and marital status. Objective risk was associated with getting tested only among participants who completed a genetic counseling session. This suggests that the decision about whether to proceed with testing is appropriately influenced by knowledge of objective risk that is conveyed through genetic counseling. In contrast, perceived stress was associated with a decreased likelihood of completing genetic testing in the ITT but not PP analyses. This may suggest that perceived stress serves as a barrier to participating in counseling but became less important after counseling. Perhaps women who were experiencing moderate stress avoided the potential added stressor of genetic counseling. This is consistent with previous data highlighting the roles of stress and avoidant coping as barriers to completing the HBOC genetic testing process.26 Finally, being married/partnered was associated with getting tested only among participants who completed a genetic counseling session. This suggests that the life-cycle stability of long-term partnership may create a more conducive environment for pursuing BRCA1/2 testing and the subsequent risk-management decision-making.27,28
Neither perceived stress nor objective risk interacted with group assignment, suggesting that the effects of these variables were comparable in both TC and UC; interactions with marital status were not tested.
Given our previously reported difference in genetic testing uptake between the two groups,9 a key aim of this report was to explore moderators that could help to explain this unexpected difference. The only variable that moderated the association between group and genetic testing uptake was race/ethnicity. Compared with non-Hispanic white participants, minority participants were significantly less likely to undergo BRCA1/2 testing when randomized to the telephone counseling and when limited to participants who completed an initial genetic counseling session but were no less likely than whites to be tested when randomized to in-person counseling or when limited to those who completed an in-person counseling session. The differential impact of race between UC and TC largely accounts for the overall uptake difference between these groups. Previous studies have reported lower rates of BRCA1/2 testing for minority participants receiving standard in-person genetic counseling and testing15,29,30 and have speculated on the contribution of access and awareness to decreased uptake. However, our sample focused on women who had self-referred for genetic counseling. Thus, our data suggest that the lower rate of counseling and testing in minority women cannot be fully explained by reduced access and awareness.15,16
There are several plausible explanations for the lower rate of testing among minority women in the TC arm. For all women receiving TC, the logistics of completing testing may have served as a barrier. Whereas UC participants could provide DNA immediately after their genetic counseling session, TC participants had to travel to a doctor’s office, laboratory, or the genetic counseling clinic to provide DNA. It is possible that these practical barriers may have been more important for minority participants. For example, evidence suggests that minorities are less likely to have a regular health-care provider to go to for DNA provision.31 Second, a recent report32 indicates that nonwhite participants experience high and clinically significant levels of distress and depression related to genetic counseling and testing. For participants experiencing this distress during genetic counseling, choosing not to pursue testing may be a coping strategy. This line of evidence suggests that particular attention should be given to assessing distress during the initial genetic counseling session.
Third, it is possible that unmeasured genetic counseling process differences may have differentially impacted minority participants. Although explicit biases are rare, social patterns related to race/ethnicity from the dominant culture are evident in health-care communication across almost all services and illnesses.33,34,35,36,37,38 Thus, minority patients often receive slightly poorer and less patient-centered communication from their providers. Further, there is some evidence that TC increases specific negative communication patterns, such as less rapport-building, increased verbal dominance by the health-care provider, and fewer problems disclosed by patients.11,39 Thus, it is possible that the telephone delivery of genetic counseling compounded such existing differences in verbal and non-verbal communication to minority participants. To our knowledge, no process studies have directly investigated the effect of telephone versus in-person counseling on communication with minority and racial majority patients.
The present findings suggest that clinicians should consider the possibility that delivering counseling via telephone may lead to lower rates of BRCA1/2 genetic testing among minority women. However, this concern should be balanced with the possibility that offering telephone delivery may increase access in the first place.40 Thus, the question of whether overall rates of testing would be increased with the availability of telephone delivery remains to be answered. However, for those women who do complete telephone genetic counseling, additional care should be taken to assess and address potential barriers to completing genetic testing. With the availability of buccal sampling for DNA provision, it is possible that one of the major barriers to completing testing could be greatly minimized. Despite the undefined mechanism for the interaction between race/ethnicity and randomization group, these findings suggest that attention to communication quality and responding to signs of distress for all patients, but especially for minority patients receiving genetic counseling by telephone, may address potential aspects of the identified discrepancy in testing uptake.
Our study had several limitations. First, because the study sample comprised participants in a randomized trial, these results may not be generalizable to the larger population of women seeking genetic counseling and testing. Specifically, the overall completion rate of both counseling and testing may be higher than in the general population. It is also possible that some of the participants who did not complete genetic counseling may have chosen to receive counseling and testing outside of the study protocol. Although at least two of the enrolled women who did not complete genetic counseling as part of this protocol went on to receive clinical genetic counseling through one of our programs, it is possible that some women pursued genetic counseling elsewhere. Additionally, although this large multisite study enrolled a sample that reflects the typical genetic counseling population, the fact remains that the sample was primarily non-Hispanic white and well educated. Also, the heterogeneous minority race/ethnicity categorization did not allow sufficient power to investigate more specific associations between race/ethnicity and uptake. Finally, although studying many psychosocial and biomedical associations, this study did not seek to characterize patient-reported reasons for test uptake or lack thereof; the collection of that type of information could have further contextualized our findings.
Despite these limitations, the present study provides information about the potential barriers and facilitators to genetic testing across two modes of clinical service delivery. These results indicate an interaction between race and randomization group, such that minority women assigned to telephone counseling are the least likely to complete genetic testing, and it is this difference that makes up the majority of differential uptake between randomization groups. As other modes of delivery emerge for genetic counseling and testing, attention to factors that influence uptake and outcomes will be important.
References
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology. Genetic/Familial High-Risk Assessment: Breast and Ovarian. V.1.2014. http://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf.
US Preventive Services Task Force. Risk Assessment, Genetic Counseling, and Genetic Testing for BRCA-Related Cancer: Draft Recommendation Statement. April 2013. AHRQ Publication No. 12-05164-EF-2. http://www.uspreventiveservicestaskforce.org/uspstf12/brcatest/draftrecbrcatest.htm.
National Society of Genetic Counselors. 2012 Professional Status Survey: Executive Summary. http://nsgc.org/p/cm/ld/fid=68.
Brierley KL, Blouch E, Cogswell W, et al. Adverse events in cancer genetic testing: medical, ethical, legal, and financial implications. Cancer J 2012;18:303–309.
Vig HS, Wang C . The evolution of personalized cancer genetic counseling in the era of personalized medicine. Fam Cancer 2012;11:539–544.
Baumanis L, Evans JP, Callanan N, Susswein LR . Telephoned BRCA1/2 genetic test results: prevalence, practice, and patient satisfaction. J Genet Couns 2009;18:447–463.
Bradbury AR, Patrick-Miller L, Fetzer D, et al. Genetic counselor opinions of, and experiences with telephone communication of BRCA1/2 test results. Clin Genet 2011;79:125–131.
Wham D, Vu T, Chan-Smutko G, Kobelka C, Urbauer D, Heald B . Assessment of clinical practices among cancer genetic counselors. Fam Cancer 2010;9:459–468.
Schwartz MD, Valdimarsdottir HB, Peshkin BN, et al. Randomized noninferiority trial of telephone versus in-person genetic counseling for hereditary breast and ovarian cancer. J Clin Oncol 2014;32:618–626.
McKinstry B, Sheikh A . Unresolved questions in telephone consulting. J R Soc Med 2006;99:2–3.
McKinstry B, Hammersley V, Burton C, et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010;19:298–303.
Helmes AW, Culver JO, Bowen DJ . Results of a randomized study of telephone versus in-person breast cancer risk counseling. Patient Educ Couns 2006;64:96–103.
Mackenzie A, Patrick-Miller L, Bradbury AR . Controversies in communication of genetic risk for hereditary breast cancer. Breast J 2009;15(suppl 1):S25–S32.
Kinney AY, Butler KM, Boucher KM, et al. Telephone vs. in-person genetic counseling for hereditary breast and ovarian cancer in urban and rural women: a cluster randomized trial. J Natl Cancer Inst, in press.
Armstrong K, Micco E, Carney A, Stopfer J, Putt M . Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA 2005;293:1729–1736.
Forman AD, Hall MJ . Influence of race/ethnicity on genetic counseling and testing for hereditary breast and ovarian cancer. Breast J 2009;15(suppl 1):S56–S62.
Peshkin BN, Demarco TA, Graves KD, et al. Telephone genetic counseling for high-risk women undergoing BRCA1 and BRCA2 testing: rationale and development of a randomized controlled trial. Genet Test 2008;12:37–52.
Berry DA, Iversen ES Jr, Gudbjartsson DF, et al. BRCAPRO validation, sensitivity of genetic testing of BRCA1/BRCA2, and prevalence of other breast cancer susceptibility genes. J Clin Oncol 2002;20:2701–2712.
Erblich J, Brown K, Kim Y, Valdimarsdottir HB, Livingston BE, Bovbjerg DH . Development and validation of a Breast Cancer Genetic Counseling Knowledge Questionnaire. Patient Educ Couns 2005;56:182–191.
Lipkus IM, Klein WM, Rimer BK . Communicating breast cancer risks to women using different formats. Cancer Epidemiol Biomarkers Prev 2001;10:895–898.
O’Connor AM . Validation of a decisional conflict scale. Med Decis Making 1995;15:25–30.
Horowitz M, Wilner N, Alvarez W . Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979;41:209–218.
Cohen S, Kamarck T, Mermelstein R . A global measure of perceived stress. J Health Soc Behav 1983;24:385–396.
Ware J Jr, Kosinski M, Keller SD . A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–233.
Busija L, Pausenberger E, Haines TP, Haymes S, Buchbinder R, Osborne RH . Adult measures of general health and health-related quality of life: Medical Outcomes Study Short Form 36-Item (SF-36) and Short Form 12-Item (SF-12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Short Form 6D (SF-6D), Health Utilities Index Mark 3 (HUI3), Quality of Well-Being Scale (QWB), and Assessment of Quality of Life (AQoL). Arthritis Care Res (Hoboken) 2011;63(suppl 11):S383–S412.
Dougall AL, Smith AW, Somers TJ, Posluszny DM, Rubinstein WS, Baum A . Coping with genetic testing for breast cancer susceptibility. Psychosom Med 2009;71:98–105.
Hoskins LM, Werner-Lin A . A multi-case report of the pathways to and through genetic testing and cancer risk management for BRCA mutation-positive women aged 18-25. J Genet Couns 2013;22:27–38.
Hoskins LM, Greene MH . Anticipatory loss and early mastectomy for young female BRCA1/2 mutation carriers. Qual Health Res 2012;22:1633–1646.
Graves KD, Christopher J, Harrison TM, Peshkin BN, Isaacs C, Sheppard VB . Providers’ perceptions and practices regarding BRCA1/2 genetic counseling and testing in African American women. J Genet Couns 2011;20:674–689.
Levy DE, Byfield SD, Comstock CB, et al. Underutilization of BRCA1/2 testing to guide breast cancer treatment: black and Hispanic women particularly at risk. Genet Med 2011;13:349–355.
Beal AC, Chou SC, Palmer RH, Testa MA, Newman C, Ezhuthachan S . The changing face of race: risk factors for neonatal hyperbilirubinemia. Pediatrics 2006;117:1618–1625.
Cukier YR, Thompson HS, Sussner K, et al. Factors associated with psychological distress among women of African descent at high risk for BRCA mutations. J Genet Couns 2013;22:101–107.
Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR . Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med 2003;139:907–915.
Gordon HS, Street RL Jr, Sharf BF, Souchek J . Racial differences in doctors’ information-giving and patients’ participation. Cancer 2006;107:1313–1320.
Johnson RL, Roter D, Powe NR, Cooper LA . Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health 2004;94:2084–2090.
Smedley BD, Stith AY, Nelson AR . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press: Washington, DC, 2003.
Street RL Jr, O’Malley KJ, Cooper LA, Haidet P . Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med 2008;6:198–205.
Thornton RL, Powe NR, Roter D, Cooper LA . Patient-physician social concordance, medical visit communication and patients’ perceptions of health care quality. Patient Educ Couns 2011;85:e201–e208.
Agha Z, Roter DL, Schapira RM . An evaluation of patient-physician communication style during telemedicine consultations. J Med Internet Res 2009;11:e36.
Cohen SA, Marvin ML, Riley BD, Vig HS, Rousseau JA, Gustafson SL . Identification of genetic counseling service delivery models in practice: a report from the NSGC Service Delivery Model Task Force. J Genet Couns 2013;22:411–421.
Acknowledgements
Grant support was received from the National Cancer Institute (grants R01 CA108933 and P30 CA051008) and the Jess and Mildred Fisher Center for Familial Cancer Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Butrick, M., Kelly, S., Peshkin, B. et al. Disparities in uptake of BRCA1/2 genetic testing in a randomized trial of telephone counseling. Genet Med 17, 467–475 (2015). https://doi.org/10.1038/gim.2014.125
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2014.125
Keywords
This article is cited by
-
The role of virtual consultations in cancer genetics: challenges and opportunities introduced by the COVID-19 pandemic
BJC Reports (2023)
-
Examining the uptake of predictive BRCA testing in the UK; findings and implications
European Journal of Human Genetics (2021)
-
The Genetic Education for Men (GEM) Trial: Development of Web-Based Education for Untested Men in BRCA1/2-Positive Families
Journal of Cancer Education (2021)
-
Exome sequencing reveals a high prevalence of BRCA1 and BRCA2 founder variants in a diverse population-based biobank
Genome Medicine (2020)
-
Predictors of contralateral prophylactic mastectomy in genetically high risk newly diagnosed breast cancer patients
Breast Cancer Research and Treatment (2020)