Abstract
Purpose:
The Kathleen Cuningham Foundation Consortium for Research into Familial Aspects of Breast Cancer (kConFab) is a large-scale research study that notifies participants when new, personally relevant, information is discovered. In 2009, the (kConFab) instituted an intensive notification process to ensure at-risk individuals were effectively notified. This study (i) evaluated the impact of intensive notification on genetic testing uptake; (ii) identified those most likely to undergo testing postnotification; and (iii) identified those most likely to acknowledge that they had been notified.
Methods:
Clinical/demographic data were retrieved from the (kConFab) database. Logistic regression analyses were conducted to identify potential predictors of testing uptake and notification acknowledgment using IBM SPSS.
Results:
A total of 155 of 1,812 individuals underwent testing after standard notification (8.6%). In comparison, 23/291 individuals (7.9%) notified using the “intensive” approach underwent testing (χ2 = 0.14; P = 0.71). After controlling for notification process, females and participants with a previous cancer were most likely to have undergone testing (P < 0.006). Older individuals (50+ years) were most likely to acknowledge they had been notified (P = 0.038).
Conclusion:
Increasing the intensity of participant follow-up did not increase genetic testing uptake. The challenge to effectively notify participants, and increase the proportion whose risk is managed clinically, remains, particularly for males and individuals unaffected by cancer.
Genet Med 2013:15(3):187–194
Similar content being viewed by others
Introduction
In the years immediately following the identification of mutations associated with increased risk of breast and/or ovarian cancer, clear evidence of survival benefits resulting from genetic testing was lacking.1 Making the decision to undergo mutation analysis was then not clear-cut, and the appropriate clinical approach was to allow at-risk patients to weigh up the potential benefits and risks of genetic testing in their situation and to encourage them to make their own testing decisions.1 However, research demonstrating the potential positive impact of genetic testing for breast and/or ovarian cancer-related mutations is mounting.2,3
Testing for the presence of BRCA1 and BRCA2 mutations can be beneficial for individuals diagnosed with cancer, as well as those currently unaffected by cancer. For newly diagnosed breast cancer patients, for example, identification of a BRCA1 and/or BRCA2 mutation may improve prognosis by allowing tailoring of their surgical, radiotherapy, and chemotherapeutic treatment to their mutation status.2 Genetic testing also allows more accurate prognostic information to be provided to both breast4 and ovarian5 cancer patients identified as BRCA1 and/or BRCA2 mutation carriers, as well as those found to be noncarriers.6
For unaffected female mutation carriers, the striking effect of risk reducing salpingo-oophorectomy on all-cause, breast cancer–specific, and ovarian cancer–specific mortality can no longer be ignored.7 In addition, the evidence of the benefit of breast cancer screening with magnetic resonance imaging is now also clearer.6,8 There is growing evidence of the significant reduction of breast cancer incidence from risk-reducing mastectomy9,10 as well as evidence for medical prevention.11 Although there has been some debate regarding cancer risk in unaffected noncarriers of a BRCA1 and/or BRCA2 mutation,12 recent studies suggest that individuals identified as noncarriers can be reassured that their breast/ovarian cancer risk is similar to that of the general population.13
Given this, the clinical mandate in genetics is changing to one of more proactive encouragement of the uptake of genetic testing in at-risk individuals.2,5 In fact, although tools to assist individuals in choosing whether or not to undergo genetic testing were previously much needed,14 tools to assist individuals in making decisions regarding how to manage their risk after genetic testing are now becoming more widely adopted.15 However, despite the building data supporting its benefits, uptake of genetic testing by at-risk individuals in the general community remains erratic at best.16,17 Despite concerted efforts in the research and clinical communities to understand and address barriers to the uptake of genetic counseling and testing by individuals identified to be at increased risk,18,19 efforts to increase uptake have generally resulted in little change. This is particularly problematic in the context of large-scale research projects in which genetic information about research participants can become available over time.
One such project is the Kathleen Cuningham Foundation Consortium for Research into Familial Aspects of Breast Cancer (kConFab), which is a research study that recruits individuals with a strong family history of breast and/or ovarian cancer. The broad aim of the consortium is to make data and biospecimens available to researchers for use in peer-reviewed, ethically approved, funded research projects on familial aspects of breast cancer. kConFab began enrolling families with a strong history of breast and/or ovarian cancer in 1997 and as of February 2012, it stores genetic, epidemiological, medical, and psychosocial data collected from 1,482 multigenerational multicase kindreds in a central relational database. Biospecimens collected from family members are used to characterize germ-line mutations in predisposing genes such as BRCA1, BRCA2, ATM, and CHEK2, and to assist in the identification of new breast cancer genes in “BRCAX” families (patients where a known causative gene mutation has not yet been identified).
When consented to the project, kConFab participants are given the option on their consent form to be notified about genetic information that may be of clinical significance to themselves and their family. Every 6 months, the kConFab administration generates a list of families on whom there is new, clinically relevant, research mutation test results, and sends a letter to each individual notifying them that (i) a gene fault of clinical significance (i.e., a mutation) has been found in their family; (ii) this mutation causes an increased risk of cancer; and (iii) that the recipient of the letter may or may not have this gene mutation. No individual test results are provided in the letter. Instead, the letter encourages the recipient to contact a family cancer clinic to discuss this information and provides a list of contact details for all genetic clinics in Australia and New Zealand. The head clinician at each recruiting family cancer clinic has the opportunity to direct kConFab not to send letters to individuals who have already received their result in a clinic setting or to those who the clinic is aware is not at risk of the family mutation (e.g., when the parent of the participant has recently tested negative for carrying the mutation).
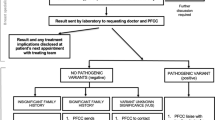
In January 2009, kConFab instituted a more intensive mutation notification process to ensure kConFab was fulfilling its obligation to notify at-risk individuals to the best of its ability. The new process involved asking letter recipients to acknowledge their receipt of the letter by returning an “acknowledgment slip” in an enclosed reply-paid envelope. After 8–10 weeks, if kConFab did not receive the acknowledgment slip, a research nurse telephoned participants to ensure they received the letter, re-sent the letter if necessary, and encouraged the individual to return his or her acknowledgment slip. This process is summarized in Figure 1 .
This change in protocol was undertaken to increase the number of kConFab participants who are adequately informed when new genetic information becomes available through the research studies. This study had five aims: (i) to measure the proportion of individuals participating in kConFab who had already attended a family cancer clinic for genetic testing before they were informed about the genetic information identified by the research study (these individuals would have been offered testing on the basis of clinical, rather than research, information); (ii) to evaluate the impact of introducing a more intensive mutation notification process on the uptake of genetic testing in at-risk individuals (that is, to compare the “letter only” group with the “letter plus acknowledgment slip plus telephone contact” group); (iii) to identify those individuals who are most (and least) likely to attend a family cancer clinic service and undergo genetic testing after they have been informed about newly available genetic information through their participation in a research study; (iv) to identify those individuals who are most (and least) likely to respond to a request to return an acknowledgment slip to acknowledge that they have been informed about the newly available genetic information; and (v) to report the follow-up status of those who do not respond to this request.
Materials and Methods
kConFab recruits multicase breast and/or ovarian cancer families in Australia (more details regarding eligibility criteria and family characteristics can be found in Mann et al.20 and at http://www.kconfab.org). The average number of family members who have a strong family history of breast and/or ovarian cancer per family in kConFab is 46 people per pedigree (median = 38). Including the individuals without a strong family history, the average number of family members per family is 63 (median = 48). Ethical approval for the study was obtained from all recruiting family cancer clinic sites in Australia and New Zealand and all kConFab participants provided individual informed consent. Study participants included all those individuals who (i) consented to participate in the kConFab research program, (ii) consented to be notified when new genetic information of potential clinical significance was identified (the majority of kConFab participants consent to be notified, with the most recent figures indicating that 12,718 of 13,732 (92.6%) participants have consented), and (iii) were sent a mutation notification letter by kConFab.
Data analysis
All responses and follow-up for mail-outs to participants were stored in a Microsoft SQL Server database (used to store and retrieve information from multiple databases) and were linked to the main kConFab study database to obtain patient characteristics such as mutation status, ethnicity, education, previous cancer history, and family relationships (specifically, whether or not the participant had a daughter). Data sets were extracted using Microsoft Access to query and link to the main dataset. Microsoft Excel was used to calculate descriptive statistics. To identify potential predictors of genetic testing uptake and response to kConFab’s request to return the acknowledgment slip, a series of logistic regression analyses were run using IBM SPSS Statistics, version 19. The variable “age” was converted into three categories to improve clinical relevance and ease of interpretation (Group 0 = 0–29 years, Group 1 = 30–49 years, and Group 2 = 50+ years). Predictor variables with P ≤ 0.10, when analyzed bivariately, were included in multivariate analyses, and a progressive, backward elimination modeling strategy was employed until a final model was obtained containing only variables with P < 0.05. Interaction terms were entered into the final models separately, with their corresponding main effects.
Results
Sample characteristics
No statistically significant differences in age, gender, or education levels were observed when comparing the characteristics of the study participants (i.e., those who received a mutation notification letter) relative to the entire kConFab cohort. Table 1 summarizes the characteristics of the sample for this study, whose mean age was 49 years (range: 18–98 years). Fifty-three percent were female (n = 1,311), 37.9% of participants held postschool qualifications, and the majority (95.8%) identified their ethnic background as “White” or “Caucasian.”
Proportion of individuals who underwent clinical mutation testing before research
Of the 3,840 individuals for whom new genetic information became available during the study period, 1,389/3,840 (36.2%) had already attended a family cancer clinic for genetic testing (as confirmed by a clinical mutation test report submitted to kConFab) before receiving their letter from kConFab, leaving a sample of 2,451 individuals (see Table 1 for their characteristics). A further 348 individuals were not sent a mutation notification letter on the basis of clinical advice from their family cancer clinic (either because they had very recently been to clinic and receipt of the mutation notification letter would be confusing, or because, in the clinical opinion of staff, they were unlikely to cope with the information contained in the letter at the current time (e.g., there had been a recent bereavement in the family or there were significant distress or mental health concerns)). Of these, 16/378 (4.6%) underwent genetic testing through their clinic during the study period.
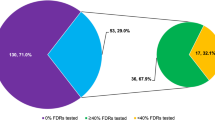
This left a sample of 2,103 individuals who were mailed a mutation notification letter because the research group had no way of knowing whether they had attended a clinic previously. Of the 2,103 individuals, 1,289 (61.3%) had at-risk daughters.
Impact of the intensive mutation notification process
Of the 2,103 notified participants, 1,812 were notified by “letter only,” whereas 291 were notified using the more intensive process (letter plus acknowledgment slip plus telephone call). Of note, 155/1,812 (8.6%) individuals underwent mutation testing after notification using the “letter only” approach. In comparison, 23/291 individuals (7.9%) notified using the “intensive” approach underwent mutation testing. This difference was not statistically significant (χ2 = 0.14; P = 0.71). A series of logistic regression analyses was performed to determine the relative contribution of the following factors to the participants’ decisions to undergo genetic testing: age, gender, education, previous cancer history (“no”/“yes, diagnosed prior to participation in kConFab” and “yes, diagnosed after their participation in kConFab”), and presence of daughters (“yes”/“no”).
After controlling for group (i.e., participants’ notification process), gender and cancer history predicted whether participants underwent genetic testing. Females were 1.67 times more likely to have undergone genetic testing than males (P = 0.005). Individuals who had previously been diagnosed with cancer either before or after their recruitment into kConFab were more likely to undergo genetic testing (in comparison with participants with no previous cancer history, participants diagnosed with cancer before they were recruited into kConFab were 2.9 times more likely to have been tested (P < 0.001), whereas participants diagnosed with cancer after they were recruited into kConFab were 3.2 times more likely to be tested (P = 0.002)).
Predictors of response to request to acknowledge receipt of the letter
In total, 112/291 participants (38.5%) in the “intensive notification group” returned their acknowledgment slip within 10 weeks of receiving it. Table 2 presents a summary of the characteristics of those who did, and did not, return the acknowledgment slip. A series of logistic regression analyses were performed to determine the relative contribution of these factors to participants’ responses to kConFab’s request to return the acknowledgment slip: age, gender, education, previous cancer history (“no”/“yes, diagnosed prior to participation in kConFab” and “yes, diagnosed with cancer after their participation in kConFab”) and presence of daughters (“yes”/“no”).
Age and gender appeared to predict participants’ response to kConFab’s request to return the acknowledgment slip. Specifically, individuals in the older age category (i.e., those over 50) were 2.3 times more likely to return the acknowledgment slip than individuals in the youngest group (0–29 year olds) (P = 0.038). With regard to gender, females appeared to be more likely to return their acknowledgment slip than males. This effect was not significant (females were 1.6 times more likely to respond than males, having allowed for age (P = 0.067)).
Follow-up status of nonresponders to request to return acknowledgment slip
The kConFab research nurse was able to contact the large majority of nonresponders by telephone, with only 14/179 nonresponders (7.8%) being unable to be contacted by kConFab and lost to their immediate family members. The research nurse left a telephone message (but did not speak to) a further 7 nonresponders (3.9%). Of the 158 nonresponders (88.3%) who the research nurse was able to speak with, 65/158 (41.1%) had received the letter but did not return the acknowledgment slip, 42/158 (26.6%) reported that they had not received the letter (despite it being sent to the correct address), and 51/158 (32.3%) requested that the research nurse re-send a new copy of the letter. Of the 51 requests for the letter to be re-sent, the majority of acknowledgment slips were not then returned (44/51, 86.3%).
Discussion
The challenge to effectively notify individuals about new genetic information discovered in research studies, and to increase the proportion whose risk is managed clinically, remains. This study demonstrated that an intensive follow-up process (involving requesting acknowledgment of receipt of the letter and follow-up phone calls), was unable to increase the uptake of genetic testing as compared with the distribution of a single notification letter. Our data do not support the intensive follow-up strategy. However, confirmatory studies are needed before recommending against it.
The proportion of individuals who participated in this research study and concurrently sought clinical genetic testing (~36%) was in line with mutation spreading (i.e., the extension of mutation testing across family members) achieved in the clinical setting (typically between 20 and 40%).16,17 Although some may argue that the responsibility for promoting mutation spreading in families lies in the clinic, improving notification of at-risk individuals is an important goal in both the research and clinical environment. Further investigation of the potential barriers to communication among genetics research groups, family cancer clinicians, at-risk individuals, and their family members is urgently needed.
Our results regarding predictors of genetic testing uptake reflect international research21 by showing that females and those with a previous cancer diagnosis were most likely to undergo genetic testing. These individuals are likely to have been managed appropriately in the clinic setting. It is concerning that those in the highest risk age category (ages 30–49) did not appear to be more likely to be tested than their younger, or older, counterparts. Also, our new, intensive, notification strategy was unable to encourage more participants to attend clinic (the standard notification rate was 8%, whereas intensive notification resulted <8% clinic attendance). Of all the predictors tested, our analyses revealed that only age was a clear predictor of whether participants were likely to acknowledge that they had received kConFab’s notification (with older participants more likely to return their acknowledgment slip).
The actual number of at-risk individuals is large. In this study, 764 research participants known by kConFab to be mutation carriers (many of whom also have at-risk offspring) did not attend a clinic for advice regarding risk management and/or preventive strategies. A proportion of these individuals may have made an informed decision to not attend clinic, however, others may be unaware of their risk and/or the services available at family cancer clinics. This is unsatisfactory given the mounting evidence that their risk could be reduced by preventative surgical7,9,10 and screening8 regimens. There is clearly more in-depth research needed to investigate the proportion of at-risk individuals making informed, vs. less informed, choices regarding their risk management options. There were also a large number of individuals who could have been reassured that they, and their offspring, were not carriers, and therefore not at increased risk.6 These individuals are likely to be aware of their family history (given their participation in kConFab) and may be concerned about their risk status. These individuals may be more distressed than those who are informed that they do, or do not, carry their family mutation,22 although recent research suggests that this is not necessarily the case.23 These individuals may also be paying higher than necessary life insurance premiums if these have been calculated on the basis of their family history alone.24
This study was unable to elucidate the reasons why the majority of at-risk individuals do not undergo genetic testing when notified about their risk. Clearly, barriers to mutation spreading are substantial. Some barriers are probably similar across research studies and clinics, whereas others are unique. Similar barriers in the two settings may include lack of effective communication between researchers/clinicians and the at-risk individual (possibly amplified by lack of genetic literacy) and lack of communication within families, among others. Barriers unique to the research environment may include the potentially increased distance between the proband and the proband’s relatives when recruited via a research study and the delay between agreeing to participate in a research study and genetic information becoming available.
Researcher/clinician–patient communication is vital. It is possible that mutation notification letter recipients do not comprehend the importance of their letter, or do not understand the relevance to their situation. We reported this as a contributing factor in a recent qualitative study including a small number of kConFab participants.25 These findings are also echoed in international research.26 Poor health literacy, and poor genetic literacy specifically, is an important problem.27 In one recent study, 30% of Australians with a university degree had poor health literacy, and the results for Australians without tertiary education were, not surprisingly, worse.28 Individuals with poor health literacy have more difficulties understanding and remembering health information,27 and find the complex information surrounding cancer29 and genetics30 particularly daunting. Genetic literacy is likely to improve over time as genetics education receives greater prominence school curriculums worldwide.31 However, low genetic literacy is likely to remain a barrier in older populations. Strategies to target low genetic literacy may involve screening to identify individuals with low genetic literacy early,30 as well as provision of low-literacy educational materials to those in need.32,33
Family communication barriers are also likely to limit mutation spreading within families in the clinic34 and research environment.35 If these barriers were identified and addressed early, family members could serve as advocates for each other’s health and improve genetic testing uptake in disinclined family members. Improving family communication is challenging, but work in this area is promising.36 It may be possible to identify, and address, unmet family communication needs to better support intra-family communication.37 Cancer risk communication tools and decision support tools may also play an important role in this process.37
In terms of barriers unique to the genetics research environment, the average number of members of each family recruited to research studies is high. The greater the distance between the proband and other family members, the less likely mutation spreading within the family will occur.38 Most probands are likely to communicate their family’s genetic information to first- and possibly second-degree relatives but are unlikely to communicate with more distant relatives.38 Also unique to the research environment is the potential time lag between joining a research study and the discovery of new, personally relevant genetic information (which can be several years). During that interval, it is likely that individuals are faced with other competing priorities, such as family and work commitments, lessening the perceived importance of the new genetic information when it becomes available. This hypothesis is supported by evidence that women with small children are less likely to undergo genetic testing than women with older children.21
Limitations
We were unable to assess actual clinic attendance, so we used mutation testing results reported to kConFab as a proxy. This means some people who attended a clinic but chose not to be tested may have been missed. However, this number is likely low given that the vast majority of Australian clinic attendees undergo testing (>95%).39 The final participant lists used in this study were also cross-checked by a research nurse in each participating family cancer clinic to minimize missing data. There may be a significant time lag between when individuals become aware of their risk and when they attend clinic, with at-risk individuals commonly not attending clinic until there is a trigger (e.g., new family diagnoses/deaths and other significant events such as starting a family).40 These triggers may, however, present too late to prevent adverse outcomes for some. It was also not possible to ascertain what proportion of nonresponsive at-risk individuals are well-informed (and making an active decision not to undergo testing) as compared with the proportion who may be making an ill-informed decision about their risk and its management.
The generalizability of the study to the clinical setting is limited by the degree of separation of individuals from the proband attending clinic and the fact that a significant proportion of kConFab participants do not attend a clinic and therefore have not had genetic counseling. However, the fact that genetic testing uptake rates of participants diagnosed with cancer before participating in kConFab was similar to the uptake rates of participants diagnosed with cancer after joining the study makes selection bias less likely.
In conclusion, further qualitative and quantitative work investigating reasons for nonattendance at family cancer clinics, and nonresponse when individuals have been notified about new, relevant genetic information is urgently needed. Innovative strategies to target individuals who are difficult to reach (including males, older individuals, and those who have never received a cancer diagnosis) need to be developed and assessed, and their impact reported widely. The ethical implications of this study are also important, and they highlight issues for further discussion in the genetics community. A key ethical question remains unanswered: “If research studies are obliged to notify participants when new genetic information becomes available, to what lengths should they go to meet these obligations?” This question also raises important financial and logistical considerations regarding how many resources research studies should (and can) use to notify their at-risk research participants.
Disclosure
The authors declare no conflict of interest.
References
Esserman L, Kaklamani V . Lessons learned from genetic testing. JAMA 2010;304:1011–1012.
Narod SA . Should all women with breast cancer be tested for BRCA mutations at the time of diagnosis? J Clin Oncol 2012;30:2–3.
Domchek SM, Friebel TM, Rebbeck TR . Association of risk-reducing surgery with cancer risks and mortality in BRCA mutation carriers—reply. JAMA 2010;304:2695–2696.
Goodwin PJ, Phillips KA, West DW, et al. Breast cancer prognosis in BRCA1 and BRCA2 mutation carriers: an International Prospective Breast Cancer Family Registry population-based cohort study. J Clin Oncol 2012;30:19–26.
Bolton KL, Chenevix-Trench G, Goh C, et al.; EMBRACE; kConFab Investigators; Cancer Genome Atlas Research Network. Association between BRCA1 and BRCA2 mutations and survival in women with invasive epithelial ovarian cancer. JAMA 2012;307:382–390.
Kurian AW, Gong GD, John EM, et al. Breast cancer risk for noncarriers of family-specific BRCA1 and BRCA2 mutations: findings from the Breast Cancer Family Registry. J Clin Oncol 2011;29:4505–4509.
Domchek SM, Friebel TM, Garber JE, et al. Occult ovarian cancers identified at risk-reducing salpingo-oophorectomy in a prospective cohort of BRCA1/2 mutation carriers. Breast Cancer Res Treat 2010;124:195–203.
Warner E, Hill K, Causer P, et al. Prospective study of breast cancer incidence in women with a BRCA1 or BRCA2 mutation under surveillance with and without magnetic resonance imaging. J Clin Oncol 2011;29:1664–1669.
Domchek SM, Friebel TM, Singer CF, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA 2010;304:967–975.
Evans DG, Baildam AD, Anderson E, et al. Risk reducing mastectomy: outcomes in 10 European centres. J Med Genet 2009;46:254–258.
Phillips K, Milne R, Rookus M, et al. Tamoxifen and risk of contralateral breast cancer for BRCA1 and BRCA2 mutation carriers: A combined analysis from the Kathleen Cuningham Foundation Consortium for Research into Familial Breast Cancer (kConFab), the International BRCA1 and BRCA2 Carrier Cohort Study (IBCCS), and the Breast Cancer Family Registry (BCFR). J Clin Oncol 2011;29(suppl), abstr:1500.
Smith A, Moran A, Boyd MC, et al. Phenocopies in BRCA1 and BRCA2 families: evidence for modifier genes and implications for screening. J Med Genet 2007;44:10–15.
Kurian AW, Sigal BM, Plevritis SK . Survival analysis of cancer risk reduction strategies for BRCA1/2 mutation carriers. J Clin Oncol 2010;28:222–231.
Wakefield CE, Meiser B, Homewood J, et al.; AGenDA Collaborative Group. A randomized controlled trial of a decision aid for women considering genetic testing for breast and ovarian cancer risk. Breast Cancer Res Treat 2008;107:289–301.
Kurian AW, Munoz DF, Rust P, et al. Online tool to guide decisions for BRCA1/2 mutation carriers. J Clin Oncol 2012;30:497–506.
Suthers GK, Armstrong J, McCormack J, Trott D . Letting the family know: balancing ethics and effectiveness when notifying relatives about genetic testing for a familial disorder. J Med Genet 2006;43:665–670.
O’Neill SM, Peters JA, Vogel VG, Feingold E, Rubinstein WS . Referral to cancer genetic counseling: are there stages of readiness? Am J Med Genet C Semin Med Genet 2006;142C:221–231.
Caruso A, Vigna C, Bigazzi V, et al. Factors associated with an individuals’ decision to withdraw from genetic counseling for BRCA1 and BRCA2 genes mutations: are personality traits involved? Fam Cancer 2011;10:581–589.
Chivers Seymour K, Addington-Hall J, Lucassen AM, Foster CL . What facilitates or impedes family communication following genetic testing for cancer risk? A systematic review and meta-synthesis of primary qualitative research. J Genet Couns 2010;19:330–342.
Mann GJ, Thorne H, Balleine RL, et al.; Kathleen Cuningham Consortium for Research in Familial Breast Cancer. Analysis of cancer risk and BRCA1 and BRCA2 mutation prevalence in the kConFab familial breast cancer resource. Breast Cancer Res 2006;8:R12.
Meiser B . Psychological impact of genetic testing for cancer susceptibility: an update of the literature. Psychooncology 2005;14:1060–1074.
Lerman C, Hughes C, Lemon SJ, et al. What you don’t know can hurt you: adverse psychologic effects in members of BRCA1-linked and BRCA2-linked families who decline genetic testing. J Clin Oncol 1998;16:1650–1654.
Foster C, Evans DG, Eeles R, et al. Non-uptake of predictive genetic testing for BRCA1/2 among relatives of known carriers: attributes, cancer worry, and barriers to testing in a multicenter clinical cohort. Genet Test 2004;8:23–29.
Subramanian K, Lemaire J, Hershey JC, Pauly MV, Armstrong K, Asch DA . Estimating adverse selection costs from genetic testing for breast and ovarian cancer: the case of life insurance. J Risk Insur 1999;66:531–550.
Wakefield CE, Ratnayake P, Meiser B, et al.; Kathleen Cuningham National Consortium for Research into Familial Breast Cancer (kConFab). “For all my family’s sake, I should go and find out”: an Australian report on genetic counseling and testing uptake in individuals at high risk of breast and/or ovarian cancer. Genet Test Mol Biomarkers 2011;15:379–385.
Vadaparampil ST, Quinn GP, Miree CA, Brzosowicz J, Carter B, Laronga C . Recall of and reactions to a surgeon referral letter for BRCA genetic counseling among high-risk breast cancer patients. Ann Surg Oncol 2009;16:1973–1981.
Koay K, Schofield P, Jefford M . Importance of health literacy in oncology. Asia Pac J Clin Oncol 2012;8:14–23.
Australian Bureau of Statistics. Health literacy, Australia, Cat. No. 4833.0. Canberra, Australia, 2006.
Davis TC, Williams MV, Marin E, Parker RM, Glass J . Health literacy and cancer communication. CA Cancer J Clin 2002;52:134–149.
Erby LH, Roter D, Larson S, Cho J . The rapid estimate of adult literacy in genetics (REAL-G): a means to assess literacy deficits in the context of genetics. Am J Med Genet A 2008;146A:174–181.
Drew JC, Jordan JC, Triplett EW . Building a Genetics Curriculum: Needs Assessment Survey of Middle and High School Students. University of Florida: Florida, Gainsville, 2009.
Holmes-Rovner M, Stableford S, Fagerlin A, et al. Evidence-based patient choice: a prostate cancer decision aid in plain language. BMC Med Inform Decis Mak 2005;5:16.
Smith SK, Trevena L, Simpson JM, Barratt A, Nutbeam D, McCaffery KJ . A decision aid to support informed choices about bowel cancer screening among adults with low education: randomised controlled trial. BMJ 2010;341:c5370.
Sermijn E, Goelen G, Teugels E, et al. The impact of proband mediated information dissemination in families with a BRCA1/2 gene mutation. J Med Genet 2004;41:e23.
Ratnayake P, Wakefield CE, Meiser B, et al.; Kathleen Cuningham National Consortium for Research into Familial Breast Cancer. An exploration of the communication preferences regarding genetic testing in individuals from families with identified breast/ovarian cancer mutations. Fam Cancer 2011;10:97–105.
Forrest LE, Burke J, Bacic S, Amor DJ . Increased genetic counseling support improves communication of genetic information in families. Genet Med 2008;10:167–172.
Sharff ME, DeMarco TA, Mays D, et al. Parenting through genetic uncertainty: themes in the disclosure of breast cancer risk information to children. Genet Test Mol Biomarkers 2012;16:376–382.
McGivern B, Everett J, Yager GG, Baumiller RC, Hafertepen A, Saal HM . Family communication about positive BRCA1 and BRCA2 genetic test results. Genet Med 2004;6:503–509.
Clarke N, Shanley S, Smith M, Leary J, Kirk J . An audit of uptake of BRCA gene predictive testing at a familial cancer service. Paper presented at: kConFab Familial breast cancer conference 2010; Couran Cove, Australia 2010.
Wakefield CE, Ratnayake P, Meiser B, et al.; Kathleen Cuningham National Consortium for Research into Familial Breast Cancer (kConFab). “For all my family’s sake, I should go and find out”: an Australian report on genetic counseling and testing uptake in individuals at high risk of breast and/or ovarian cancer. Genet Test Mol Biomarkers 2011;15:379–385.
Acknowledgements
We thank all the kConFab research nurses and staff, the heads and staff of the Family Cancer Clinics, and the Clinical Follow-Up Study (funded 2001-2009 by NHMRC and currently by the National Breast Cancer Foundation and Cancer Australia no. 628333) for their contributions to this resource, and the many families who contribute to kConFab. kConFab is supported by grants from the National Breast Cancer Foundation and the National Health and Medical Research Council and by the Queensland Cancer Fund, the Cancer Councils of New South Wales, Victoria, Tasmania and South Australia, and the Cancer Foundation of Western Australia. C.E.W. is supported by an Early Career Development Fellowship Grant from the Cancer Institute of NSW (11/ECF/3-43).
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Wakefield, C., Thorne, H., Kirk, J. et al. Improving mutation notification when new genetic information is identified in research: a trial of two strategies in familial breast cancer. Genet Med 15, 187–194 (2013). https://doi.org/10.1038/gim.2012.115
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2012.115
Keywords
This article is cited by
-
Development and Pilot Testing of a Decision Aid for Genomic Research Participants Notified of Clinically Actionable Research Findings for Cancer Risk
Journal of Genetic Counseling (2018)
-
Timing and context: important considerations in the return of genetic results to research participants
Journal of Community Genetics (2016)
-
Connecting patients, researchers and clinical genetics services: the experiences of participants in the Australian Ovarian Cancer Study (AOCS)
European Journal of Human Genetics (2015)
-
Misperceptions of ovarian cancer risk in women at increased risk for hereditary ovarian cancer
Familial Cancer (2014)