Abstract
Multiple endocrine neoplasia type 2 is historically composed of three clinical subtypes, all of which are associated with germline mutations in the RET proto-oncogene. Multiple endocrine neoplasia type 2A, familial medullary thyroid carcinoma, and multiple endocrine neoplasia type 2B are collectively associated with a 70–100% risk of medullary thyroid carcinoma by age 70 years. Pheochromocytomas are identified in 50% of individuals with multiple endocrine neoplasia type 2A and multiple endocrine neoplasia type 2B. Furthermore, those with multiple endocrine neoplasia type 2A have a 20–30% risk for primary hyperparathyroidism. Individuals with multiple endocrine neoplasia type 2B often have distinct physical features including mucosal neuromas of the lips and tongue, medullated corneal nerve fibers, ganglioneuromatosis of the gastrointestinal tract, distinctive facies with enlarged lips, and a “Marfanoid” body habitus. Clinical recognition and accurate diagnosis of individuals and families who are at risk of harboring a germline RET mutation is critical for the prevention and management of potentially life-threatening neoplasms. This overview summarizes the clinical description of multiple endocrine neoplasia type 2, diagnosis and testing strategies, management and surveillance, and differential diagnosis for other related syndromes.
Similar content being viewed by others
Main
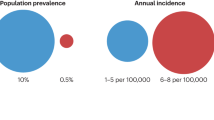
The identification and phenotypic characterization of germline high-penetrance gain-of-function mutations in the RET proto-oncogene, encoding a receptor tyrosine kinase, as causing the great majority of multiple endocrine neoplasia (MEN) type 2 (MEN 2) heralded the era of accurate, evidence-based molecular diagnosis, predictive testing, genetic counseling, gene-informed cancer risk assessment, and preventative medicine. MEN 2, occurring in 1:200,000 live births, is an autosomal dominant neuroendocrine neoplasia predisposition syndrome characterized by variable penetrance of medullary thyroid carcinoma (MTC), pheochromocytoma, and hyperparathyroidism (HPT). Age at presentation, frequency, and age-related penetrances of component neoplasias vary between each subtype of MEN 2 and most likely are genotype dependent.
CLINICAL DESCRIPTION OF MEN 2
Historically, MEN 2 has been divided into three subtypes depending on clinical features. With the identification and characterization of RET and genotype-associated phenotypes, it became obvious that all three subtypes are allelic and that MEN 2A and familial MTC (FMTC) are merely manifestations of different penetrances of RET mutations.1,2
Multiple endocrine neoplasia type 2A (OMIM# 171400)
MEN 2A makes up approximately 70–80% of cases of MEN 2. As genetic testing for RET mutations has become available, it has become apparent that 70–95% of individuals with MEN 2A develop MTC, approximately 50% develop pheochromocytoma, and approximately 15–30% develop HPT.1,3
MTC is generally the first manifestation of MEN 2A. Probands with MTC typically present with a neck mass or neck pain, usually before age 35 years. Up to 70% of such individuals already have cervical lymph node metastases.4 Diarrhea, the most frequent systemic manifestation, occurs in affected individuals with a plasma calcitonin concentration of more than 10 ng/mL and implies a poor prognosis. All individuals with an MTC-predisposing mutation who have not undergone prophylactic thyroidectomy demonstrate biochemical evidence of MTC by age 35 years.5,6
Pheochromocytomas usually present after MTC or concomitantly; however, they are the first symptom in 13–27% of individuals with pheochromocytomas and MEN 2A.7–9 Pheochromocytomas in persons with MEN 2A and MEN 2B are diagnosed at an earlier age, have subtler symptoms, and are more likely to be bilateral than sporadic tumors.10,11 Malignant transformation occurs in approximately 4% of cases.12 As pheochromocytoma can be the first manifestation of MEN 2A, the diagnosis of pheochromocytoma in an individual warrants further investigation for MEN 2A and other syndromes with this neoplasia as component such as von Hippel Lindau (VHL) disease and hereditary paraganglioma–pheochromocytoma syndrome.7,13
HPT in MEN 2A is typically mild and may range from a single adenoma to marked hyperplasia. Most individuals with HPT have no symptoms; however, hypercalciuria and renal calculi may occur.14 If HPT is longstanding and unrecognized, symptoms may become severe. HPT usually presents many years after the diagnosis of MTC; the average age of onset is 38 years.2,15
A small number of families with MEN 2A have pruritic cutaneous lichen amyloidosis (CLA), also known as CLA.16 This lichenoid skin lesion is located over the upper portion of the back and may appear before the onset of MTC.17 Individuals with MEN 2A and CLA almost always carry codon 634 mutations.18
Familial medullary thyroid carcinoma (OMIM# 155240)
The FMTC subtype comprises approximately 10–20% of cases of MEN 2. By operational definition, MTC is the only clinical manifestation of FMTC. The age of onset of MTC is later in FMTC, and the penetrance of MTC is lower than what is observed in MEN 2A and MEN 2B.1–3,19,20 To avoid neglecting the risk of pheochromocytoma, strict criteria should be met before a family is classified as having FMTC. In the past, some believed that a kindred with FMTC should have more than 10 members with a RET mutation, multiple individuals with a RET mutation over the age of 50 years, and all members should have an adequate medical history demonstrating a lack of pheochromocytoma or HPT.14 Today, FMTC is typically viewed as a variant of MEN 2A with decreased penetrance of pheochromocytoma and HPT, rather than a distinct subtype.2
Multiple endocrine neoplasia type 2B (OMIM# 162300)
The MEN 2B subtype comprises approximately 5% of cases of MEN 2. MEN 2B is characterized by the early development of an aggressive form of MTC in all affected individuals.21 Individuals with MEN 2B who do not undergo thyroidectomy at an early age (<1 year) are likely to develop metastatic MTC at an early age. Before intervention with early prophylactic thyroidectomy, the average age of death in individuals with MEN 2B was 21 years.
Pheochromocytomas occur in 50% of individuals with MEN 2B; approximately half are multiple and often bilateral.
Clinically significant parathyroid disease is absent in MEN 2B.
Individuals with MEN 2B may be identified in infancy or early childhood by the presence of mucosal neuromas on the anterior dorsal surface of the tongue, palate, or pharynx and a distinctive facial appearance. The lips become prominent (or “blubbery”) over time, and submucosal nodules may be present on the vermilion border of the lips. Neuromas of the eyelids may cause thickening and eversion of the upper eyelid margins. Prominent thickened corneal nerves may be seen by slit lamp examination.
Approximately 40% of affected individuals have diffuse ganglioneuromatosis of the gastrointestinal tract. Associated symptoms include abdominal distension, megacolon, constipation, or diarrhea. In one study of 19 individuals with MEN 2B, 84% reported gastrointestinal symptoms beginning in infancy or early childhood.22
Approximately 75% of affected individuals have a Marfanoid habitus, often with kyphoscoliosis or lordosis, joint laxity, and decreased subcutaneous fat. Proximal muscle wasting and weakness can also be seen.
DIAGNOSIS AND TESTING
MEN 2 includes the phenotypes MEN 2A, FMTC, and MEN 2B. Each can be diagnosed based on clinical features; but with the advances of RET testing, genotype-specific risks, and management, molecular genetic testing is virtually mandatory and is most often used to distinguish sporadic from hereditary MTC.
Clinical diagnosis: MEN 2A
MEN 2A is diagnosed clinically by the occurrence of two or more specific endocrine tumors (MTC, pheochromocytoma, or parathyroid adenoma/hyperplasia) in a single individual or in close relatives.
Clinical diagnosis: FMTC
FMTC is historically operationally diagnosed in families with four or more cases of MTC in the absence of pheochromocytoma or parathyroid adenoma/hyperplasia.1,3,23 Because RET accounts for all clinical subtypes of MEN 2, FMTC may be viewed as MEN 2A with reduced organ-specific penetrance.
Clinical diagnosis: MEN 2B
MEN 2B is diagnosed clinically by the presence of mucosal neuromas of the lips and tongue, as well as medullated corneal nerve fibers, distinctive facies with enlarged lips, an asthenic “Marfanoid” body habitus, and MTC.2
Histological, biochemical, and imaging studies
MTC and C-cell hyperplasia
MTC originates in neural crest-derived calcitonin-producing cells (C cells) of the thyroid gland. MTC is diagnosed histologically when nests of C cells appear to extend beyond the basement membrane and to infiltrate and destroy thyroid follicles. Immunohistochemistry for calcitonin expression may be performed as a pathologic diagnostic adjunct.
C-cell hyperplasia (CCH) is diagnosed histologically by the presence of an increased number of diffusely scattered or clustered C cells. In MEN 2, the age of transformation from CCH to MTC varies with different germline RET mutations.24
MTC and CCH are suspected in the presence of an elevated plasma calcitonin concentration, a specific and sensitive marker. However, CCH has been described occasionally in the setting of HPT, chronic lymphocytic thyroiditis, and aging. Secondary CCH rarely transforms to MTC.25
In provocative testing, plasma calcitonin concentration is measured before (basal level) and 2 and 5 minutes after intravenous administration of calcium (stimulated level). Other calcitonin secretagogues are also used, such as pentagastrin (available in Europe and limited in the United States). Reference levels for basal calcitonin vary across laboratories: <10 pg/mL for adult males and <5 pg/mL for adult females are typically considered normal. A basal or stimulated calcitonin level of ≥100 pg/mL is an indication for surgery.2,26 Caution should be used when interpreting calcitonin levels in children younger than 5 years.2
Pheochromocytoma
Pheochromocytoma is suspected when biochemical screening reveals elevated excretion of catecholamines and catecholamine metabolites (i.e., norepinephrine, epinephrine, metanephrine, and vanillylmandelic acid) in plasma or 24-hour urine collections.11,27 In MEN 2, pheochromocytomas consistently produce epinephrine or epinephrine and norepinephrine.27
Abdominal magnetic resonance imaging (MRI) and computed tomography (CT) are performed whenever a pheochromocytoma is suspected clinically and whenever plasma or urinary catecholamine values are increased. MRI is more sensitive than CT in detection of a pheochromocytoma. [18F]-fluorodopamine positron emission tomography (PET) is the best overall imaging modality in the localization of pheochromocytomas. If [18F]-fluorodopamine PET is unavailable, 123I- or 131I-metaiodobenzylguanidine scintigraphy should be used for further evaluation of individuals with biochemical or radiographic evidence of pheochromocytoma.28
Parathyroid abnormalities
The diagnosis of parathyroid abnormalities is made when biochemical screening reveals simultaneously elevated serum concentrations of calcium and elevated or high-normal parathyroid hormone. Postoperative parathyroid localizing studies with 99mTc-sestamibi scintigraphy may be helpful if HPT recurs. For preoperative adenoma localization, three-dimensional single-photon emission CT may also be used.29
Molecular genetic testing
RET is the only gene known to be associated with MEN 2. RET molecular genetic testing is indicated in all individuals with a diagnosis of MTC, a clinical diagnosis of MEN 2, or primary CCH.2,14 The algorithm for testing is summarized in the most recent American Thyroid Association MTC Practice Guidelines (Table 1).2 Features such as young age of onset, significant CCH, and/or multifocal disease suggest an inherited disorder.
All individuals with MTC, irregardless of other features or family history, and those with clinical features suspicious for MEN 2 and/or with family history suspicious of MEN 2 should be offered germline RET testing for exons 10, 11, and 13–16; ideally, testing should be completed preoperatively and with genetic counseling. Approximately 98% of families with MEN 2A have a RET mutation in exon 10 or 11.2,3 Families with FMTC have an identifiable RET mutation approximately 95% of the time.2,32 In addition to exons 10, 11, and 13–16, a small percentage of mutations occur in exons 5 and 8 in FMTC families. In the setting of a clinical diagnosis of MEN 2A, sequencing of the entire RET coding region should be completed if exon-specific testing is negative.
For individuals with features suggestive of MEN 2B, targeted mutation analysis or sequencing of exons 16 and 15 to detect the p.M918T and p.A883F mutations should be completed first. If mutation negative, testing for p.V804M in exon 14 followed by sequencing of the entire RET coding region should be performed. Although an isolated p.V804M mutation is associated with FMTC, p.V804M co-occurring with a second RET variant seems to result in MEN 2B.11 This strategy will detect more than 98% of mutations in individuals with MEN 2B.2
RET molecular genetic testing may be warranted in subsets of individuals presenting with apparently isolated adrenal pheochromocytoma, although other differential diagnoses such as VHL and succinate dehydrogenase-associated pheochromocytoma should also be considered.13 Testing algorithms for genes associated with paraganglioma and pheochromocytoma have been proposed based on age of onset, location, laterality, malignancy, and family history.30,31 It is important to note that unexpected germline RET mutations are rarely (if ever) found in head and neck paraganglioma presentations in the absence of other features of MEN 2 or in the absence of a family history of MEN 2 phenotype.33
Other clinical presentations may prompt consideration of genetic testing. Exon 10 sequencing should be considered in individuals with Hirschsprung disease (HSCR).2 CLA of the central upper back may prompt molecular genetic testing for the presence of a codon 634 mutation.2 The differential diagnosis in persons with intestinal ganglioneuromatosis should include MEN 2B, and RET testing may be considered.2
Rarely, a germline RET mutation may not be detected in a family with a clinical diagnosis of MEN 2A or 2B, or FMTC. At-risk relatives should be periodically screened for MTC with neck ultrasound examination, and basal and/or stimulated calcitonin measurements; for HPT with albumin-corrected calcium or ionized calcium; and for pheochromocytoma with measurement of plasma or 24-hour urine metanephrines and normetanephrines, as appropriate.2
Genetically related (allelic) disorders
Hirschsprung disease
HSCR is a complex genetic disorder characterized by aganglionosis of the gut, likely due to absent gut ganglia from premature apoptosis of the ganglia anlage. HSCR typically results in enlargement of the bowel and constipation or even obstipation in neonates. Because of a seemingly similar clinical presentation, the clinician should be careful differentiating the diagnosis of HSCR from the constipation/obstipation resulting from ganglioneuromatosis of MEN 2B. After MEN 2A and FMTC families were noted to segregate HSCR, a seemingly unrelated neurocristopathy and developmental disorder, linkage studies indeed showed that some HSCR families were linked to 10q as well.34,35 Up to 50% of familial cases and up to 35% of simplex cases (i.e., a single occurrence in a family) of HSCR are caused by germline loss-of-function mutations in the RET proto-oncogene.34–37 Germline mutations causing HSCR occur throughout the coding sequence of RET.38 Subsets of families and individuals harboring germline RET mutations in exon 10, especially affecting codons 618 and 620 cosegregate MEN 2A/FMTC and HSCR.2,3,39 Functional studies proved that missense mutations that were more N-terminal (5′) in the RET receptor had a tendency to be retained in the Golgi apparatus, thus resulting in a functional haploinsufficiency.40,41 This observation could explain the presence of both MEN 2A/FMTC and HSCR in the same individual or same family segregating a single RET mutation (e.g., C618 or C620). Based on these data, constitutional activation of the receptor tyrosine kinase is necessary and sufficient for neuroendocrine neoplasia, irrespective of number of receptors. However, a certain threshold number of RET receptors on the cell surface is important for proper development and maintenance of the nervous system of the gut.
Papillary thyroid carcinoma
Approximately 20–40% of papillary thyroid carcinoma (PTC) is associated with somatic gene rearrangements that cause juxtaposition of the tyrosine kinase domain of RET to various gene partners.42,43 A few families with rare RET exon 13 and exon 14 germline mutations have demonstrated concomitant medullary and papillary thyroid cancer (see “Genotype-Phenotype Correlations”),44,45 although other studies have shown that the family-specific RET mutation does not segregate with the PTC phenotype.46
GENOTYPE-PHENOTYPE CORRELATIONS
RET genotype-MEN 2 phenotype correlations were the first clear genotype-phenotype associations to be found in inherited neoplasia syndromes.3 The most striking observation was that gain-of-function mutations affected several hotspot codons, with the great majority mutating cysteine residues in exons 10 and 11. Notably, mutations of codon 634 in exon 11 were highly associated with the full-blown phenotype of MEN 2A, i.e., with a high prevalence of pheochromocytoma and hyperparathyroidism, with p.C634R being the most common, the most highly penetrant, and the most fulminant.1–3,47 Interestingly, the fulminant nature was reconfirmed recently where a report of 12 Brazilian families indicated that p.C634R is associated with a higher probability of having metastases at diagnosis of MTC than other codon 634 mutations.48 Although 25% of FMTC kindreds harbor a mutation in codon 634, most commonly p.C634Y, p.C634R mutations are virtually absent in this subtype.1,32
Codon 634 mutations are also associated with development of CLA.17 Among 25 individuals from three families with a codon 634 mutation, 36% had CLA.49
RET germline p.M918T mutations are only associated with MEN 2B; however, somatic mutations at this codon are frequently observed in MTC in individuals with no known family history of MTC and are overrepresented in individuals with sporadic MTC who have a particular germline RET variant, c.2439C>T; p.S836S.50
Although the initial genotype-phenotype studies would suggest that the exon 10 codon mutations, in particular at codons 609 and 611, would carry the lowest penetrance, a recent large multicenter study of 103 families with exon 10 mutations demonstrated an incidence of MTC in 77%, pheochromocytoma in 17%, and HPT in 3%.9 Although the original observations of low incidence of pheochromocytoma and HPT hold true, the incidence of MTC is quite high and should be noted.
Mutations involving the cysteine codons 609, 618, and 620 in exon 10 of RET are associated with MEN 2A or FMTC cosegregating with HSCR (mechanism described earlier).39,51,52 Initially, it was believed that 30% of individuals carrying p.C618R and p.C620R also cosegregated HSCR3; however, this was likely an overestimate, potentially due to referral bias. In an unselected, multinational series of exon 10 mutation carriers, only 7.5% of informatic carriers were found to also have a HSCR phenotype.9
Mutations at codons 768, 804, and 891 that were initially only associated with FMTC have subsequently been found in rare families with MEN 2A.53–57 Phenotypic expression of mutations at codon 804 has been shown to be highly variable, even within the same family.58,59 Some individuals with such mutations have MTC at age 5 years and fatal metastatic MTC at age 12 years, whereas other individuals with the same mutation have been shown to have normal thyroid histology at age 27 years, normal biochemical screening at age 40 years, and no clinical evidence of MTC at age 86 years. In a large family with a high level of consanguinity, biochemical testing indicated expression of thyroid disease in individuals homozygous but not heterozygous for p.V804M.60 CLA in the background of a p.V804M mutation has been reported in one individual.61
One study suggests that in addition to their association with MTC, mutations in codons 790 or 804 may be associated with PTC.44 In a large Italian family, 40% of family members with a p.V804M mutation who were examined in detail had concominant medullary and PTC.45
The American Thyroid Association Guidelines Task Force has classified mutations based on their risk for aggressive MTC (Table 2). The classification may be used in predicting phenotype and recommendations for age at which to perform prophylactic thyroidectomy and to begin biochemical screening for pheochromocytoma and hyperparathyroidism.2
DIFFERENTIAL DIAGNOSIS
Apparently sporadic MTC
There is only one genetic differential diagnosis for MTC and that is MEN 2. Therefore, it is important for medical management of the individual and his/her family to distinguish MTC presentations who have MEN 2 from those with truly sporadic MTC. In various studies of individuals with simplex MTC (i.e., no known family history of MTC or personal history of other endocrine disease), 6–9.5% were found to have disease-causing germline mutations in the RET gene.63–66 Because of this relatively high frequency of germline RET mutations, genetic counseling and testing should be offered to all individuals with MTC, a clinical diagnosis of MEN 2, or primary CCH.2
Pheochromoctyoma
The probability that pheochromocytoma is hereditary is estimated to be 84% for multifocal (including bilateral) tumors and 59% for tumors with onset on or before age 18 years.13 Approximately 25% of individuals with pheochromocytoma and no known family history of pheochromocytoma may have an inherited disease caused by a mutation in one of the following four genes, RET, VHL, SDHD, or SDHB.13,67 SDHC germline mutations are rare in apparently sporadic pheochromocytoma. The algorithm for prioritizing which gene to test is outlined by Erlic et al.31
In a large population-based study, approximately 5% of individuals with nonsyndromic pheochromocytoma and no family history of pheochromocytoma demonstrated a RET mutation.13 Of those individuals with hereditary pheochromocytoma treated at a single institution, 12% had MEN 2A, with 27% presenting with pheochromocytoma as the first manifestation of disease.7 A recent analysis of individuals with RET exon 10 mutations found that 25% of those with pheochromocytoma were diagnosed at least 1 year before MTC.9
Any individual presenting with a pheochromocytoma should be evaluated for VHL disease.31 In a population-based series, Neumann et al.13 identified germline VHL mutations in 11% of individuals with nonsyndromic pheochromocytoma and no family history of pheochromocytoma. VHL is characterized by pheochromocytoma, renal cell carcinoma, cerebellar and spinal hemangioblastoma, and retinal angioma. Some families with apparent autosomal dominant pheochromocytoma have VHL gene mutations in the absence of other clinical manifestations of VHL.7,13,68
Approximately 8.5% of individuals with apparently sporadic nonsyndromic pheochromocytoma have been shown to have a mutation in one of the succinate dehydrogenase subunit genes, SDHD or SDHB, that cause hereditary paraganglioma-pheochromocytoma syndrome.13 These genes are associated with familial paragangliomas, which are also known as extra-adrenal pheochromocytomas or glomus tumors.69,70 Although head and neck paragangliomas are common in individuals with SDHB, SDHC, and SDHD mutations, they are extremely rare in MEN 2 and VHL.71 When head and neck paraganglioma are associated with MEN 2 or VHL, individuals almost always have other syndromic features or a suggestive family history.
Although NF 1 is always included in the genetic differential diagnosis of pheochromocytoma, virtually all such presentations are accompanied by clinical features of NF 1.72 Similarly, pheochromocytoma and paraganglioma are considered rare components of MEN 1. Personal or family history of MEN 1 features should be evident.
Hyperparathryoidism (HPT)
HPT is almost never (some believe never) a first presentation of MEN 2, and so, a formal differential diagnosis section for this organ has been omitted. In contrast, HPT is commonly (said to be >80%) the first manifestation of MEN 1.
Intestinal ganglioneuromatosis
Germline analysis for the RET p.M918T and p.A883F mutations should be offered for infants and children presenting with intestinal ganglioneuromatosis.73 The only other genetic differential diagnoses to consider in intestinal ganglioneuromatosis are Cowden syndrome and type 1 neurofibromatosis.74–76 Individuals with Cowden syndrome are more likely to exhibit ganglioneuromatous polyps than those with MEN 2B or NF 1. It is important to distinguish the constipation/obstipation associated with MEN 2B-related ganglioneuromatosis from the same symptoms derived from the colonic aganglionosis seen in HSCR.
DISEASE MANAGEMENT
Treatment of manifestations
Standard treatment for MTC is surgical removal of the thyroid with regional lymph node dissection.2 Standard chemotherapy and radiation are not effective in the treatment of MTC.4 Resection and autotransplantation of parathyroid tissue are not typically performed at the time of thyroidectomy unless there is evidence of HPT.2 It is always important to ensure that pheochromocytomas are not coexistent before thyroid surgery (see later).
Pheochromocytomas detected by biochemical testing and radionuclide imaging are removed by adrenalectomy, which may be performed using video-assisted laparoscopy. Antihypertensive treatment before adrenalectomy involves the use of α- and β-adrenergic receptor blockade.11 Historically, some specialists recommended bilateral adrenalectomy at the time of demonstration of tumor even within a single adrenal gland because of the strong probability that the other adrenal gland would develop a tumor within 10 years. However, because of the risk of adrenal insufficiency and Addisonian crisis after bilateral adrenalectomy, most experts now recommend unilateral adrenalectomy in unilateral tumors and cortical-sparing adrenal surgery with close monitoring of the remnant tissue in persons with one remaining adrenal gland or bilateral pheochromocytoma.2
Parathyroid adenoma or hyperplasia diagnosed at the time of thyroidectomy is treated with resection of the visibly enlarged parathyroid gland(s), subtotal parathyroidectomy, or total parathyroidectomy with forearm autograft.2 However, in most individuals with MEN 2A, HPT is diagnosed many years after thyroidectomy. Individuals with biochemical evidence of primary HPT who have undergone prior thyroidectomy should have preoperative localization with excision of the localized hypertrophied parathyroid glands and forearm autotransplantation. Therapy with medications to control primary HPT should be considered in individuals with a high risk of surgical mortality, limited life expectancy, or persistent or recurrent primary HPT after one or more surgical attempts.2
Prevention of primary manifestations
Prophylactic thyroidectomy is the primary preventive measure for individuals with an identified germline RET mutation.2,4 Prophylactic thyroidectomy is safe for all age groups in the hands of those facile with this operation; however, the timing of the surgery is controversial.77 According to the consensus statement from the American Thyroid Association Guidelines Task Force, the age at which prophylactic thyroidectomy is performed can be guided by the codon position of the RET mutation (Table 2).2 However, these guidelines continue to be modified as more data are available.
Thyroidectomy for CCH, before progression to invasive MTC, may allow surgery to be limited to thyroidectomy with sparing of lymph nodes.14,78
For all individuals with a RET mutation who have not had a thyroidectomy, annual biochemical screening is recommended with immediate thyroidectomy if results are abnormal.79 Annual serum calcitonin screening should begin for children with MEN 2B at age 6 months and at age 3–5 years for those with MEN 2A or FMTC.2 However, caution should be used in interpreting calcitonin results for children younger than 3 years, especially children younger than 6 months.2
Prevention of secondary manifestations
Before any surgery, the presence of a functioning pheochromocytoma should be excluded by appropriate biochemical screening in any individual with MTC, MEN 2A, or MEN 2B. Individuals with undiagnosed pheochromocytoma may die from a cardiovascular hypertensive crisis perioperatively. In a prospective study of at-risk family members with the disease-causing mutation, 8% had pheochromocytoma detected at the same time as MTC.80 If pheochromocytoma is detected, adrenalectomy should be performed before thyroidectomy to avoid intraoperative catecholamine crisis.81
Surveillance
Medullary thyroid carcinoma
Approximately 50% of individuals diagnosed with MTC who have undergone total thyroidectomy and neck nodal dissections have recurrent disease.4 Furthermore, thyroid glands removed from individuals with a RET disease-causing mutation who had normal plasma calcitonin concentrations have been found to contain MTC.21 Therefore, continued monitoring for residual or recurrent MTC is indicated after thyroidectomy, even if thyroidectomy is performed before biochemical evidence of disease. The screening protocol for MTC after prophylactic thyroidectomy is an annual measurement of serum calcitonin.2 More frequent follow-up is recommended for those with residual disease.
Pheochromocytoma
For individuals whose initial screening results are negative for pheochromocytoma, annual biochemical screening is recommended, followed by MRI and/or CT if the biochemical results are abnormal.2,11 Women with MEN 2 should be screened for pheochromocytoma before a planned pregnancy or as early as possible during an unplanned pregnancy.2 Other screening studies, such as scintigraphy or PET, may be warranted in some individuals. Annual biochemical screening beginning at age 8 years has been recommended for individuals with MEN 2A or FMTC caused by mutations of codons 630 and 634 and at age 20 years for mutations in all other codons (Table 2).2 Individuals with MEN 2B should begin screening for pheochromocytoma at age 8 years.2
Parathyroid adenoma or hyperplasia
Annual biochemical screening with serum calcium concentrations and parathyroid hormone is recommended for at-risk individuals who have not had parathyroidectomy and parathyroid autotransplantation. In MEN 2A, screening should begin at age 8 years for individuals with mutations of codons 630 and 634 and by age 20 years for individuals with other RET mutations (Table 2).2 Periodic screening is recommended for individuals with FMTC beginning at age 20 years.2 Screening is likely unnecessary in MEN 2B as these individuals do not have an increased risk of HPT.
Hypoparathyroidism
All individuals who have undergone thyroidectomy and autotransplantation of the parathyroids need monitoring for possible hypoparathyroidism.
Agents/circumstances to avoid
Dopamine D2 receptor antagonists (e.g., metoclopramide and veralipride) and β-adrenergic receptor antagonists (β blockers) have a high potential to cause an adverse reaction in individuals with pheochromocytoma. Other medications including monoamine oxidase inhibitors, sympathomimetics (e.g., ephedrine), and certain peptide and corticosteroid hormones may also cause complications, whereas tricyclic antidepressants are inconsistent in causing adverse reactions.82
Testing of relatives at risk
RET molecular genetic testing should be offered to probands with any of the MEN 2 subtypes and to all at-risk members of kindreds in which a germline RET mutation has been identified in an affected family member.2,83 American Society of Clinical Oncologists identifies MEN 2 as a group 1 disorder, i.e., a well-defined hereditary cancer syndrome for which genetic testing is considered part of the standard management for at-risk family members.83
RET molecular genetic testing should be performed as soon as possible after birth in all children known to be at risk for MEN 2B.2,14 In families with MEN 2A or FMTC, molecular genetic testing should be offered to at-risk children by age 5 years, as MTC has been documented in childhood.2,14
Therapies under investigation
Clinical trials of tyrosine kinase inhibitors, such as vandetanib (ZD6474), are currently underway. In a Phase II trial, 73% (22/30) of individuals with hereditary metastatic MTC who were treated with vandetanib experienced a partial response or stable disease.84 Tyrosine kinase inhibitors are promising potential treatments for patients with unresectable, locally advanced, or metastatic MTC.
Other
Genetics clinics, staffed by genetics professionals, provide information for individuals and families regarding the natural history, treatment, mode of inheritance, and genetic risks to other family members and information about available consumer-oriented resources. The GeneTests Clinic Directory is a resource available to the public to assist in the identification of genetics clinics.
Genetic counseling
Genetic counseling is the process of providing individuals and families with information on the nature, inheritance, and implications of genetic disorders to help them make informed medical and personal decisions. The following section deals with genetic risk assessment and the use of family history and genetic testing to clarify genetic status for family members. This section is not meant to address all personal, cultural, or ethical issues that individuals may face or to substitute for consultation with a genetics professional.
Mode of inheritance
All the MEN 2 subtypes are inherited in an autosomal dominant manner.
Risk to family members
The proportion of individuals with MEN 2 who have an affected parent varies by subtype. Approximately 95% of individuals with MEN 2A have an affected parent, and approximately 5% of cases are due to de novo germline mutations.85 Because incomplete penetrance of the mutant allele is possible, some parents who have a RET mutation are asymptomatic. It is appropriate to evaluate the parents of an individual with MEN 2A for manifestations of the disorder and offer molecular genetic testing if the RET mutation has been identified in the proband.
By operational definition, individuals with FMTC have multiple family members who are affected by MTC. However, if, for example, a p.C634R mutation was identified in an individual from an FMTC family, then the clinician should be cautious that the individual has a high likelihood of developing pheochromocytoma and HPT.2,86
Approximately 50% of affected individuals with MEN 2B have a de novo germline mutation, and 50% have inherited the mutation from a parent.87 The majority of de novo mutations are paternal in origin, but cases of maternal origin have been reported.88
The risk to siblings depends on the genetic status of the parent, which can be clarified by pedigree analysis and/or molecular genetic testing. If a parent has the gene mutation, the risk is 50%. In situations of apparent de novo germline mutations, germline mosaicism in an apparently unaffected parent needs to be considered, even though such an occurrence has not yet been reported.
Each child of an individual with MEN 2 has a 50% chance of inheriting the RET mutation. The probability that the offspring of an individual with simplex MTC (i.e., no known family history of MTC) and no identifiable RET germline mutation would inherit a RET mutation is 0.18%.14,89 This estimate is based on a 95% mutation detection rate and on empiric data that 7% of individuals with sporadic MTC have a germline mutation.
Related genetic counseling issues
Consideration of molecular genetic testing of at-risk family members is appropriate for surveillance. Molecular genetic testing can be used for testing of at-risk relatives only if a disease-causing germline mutation has been identified in the family. When a known disease-causing mutation is not identified, linkage analysis can be considered in families with more than one affected family member from different generations. Because early detection of at-risk individuals affects medical management, testing of asymptomatic children is beneficial.83 Education and genetic counseling of at-risk children and their parents before genetic testing are appropriate.
When the parents of a proband with an autosomal dominant condition do not have the disease-causing mutation or clinical evidence of the disorder, it is likely that the proband has a de novo mutation. However, possible nonmedical explanations including alternate paternity or undisclosed adoption could also be explored.
For comprehensive descriptions of the medical, psychosocial, and ethical ramifications of identifying at-risk individuals through cancer risk assessment with or without molecular genetic testing, see:
-
Genetic Cancer Risk Assessment and Counseling: Recommendations of the National Society of Genetic Counselors.
-
Elements of Cancer Genetics Risk Assessment and Counseling (part of PDQ®, National Cancer Institute).
Family planning.
The optimal time for determination of genetic risk and availability of prenatal testing is before pregnancy. It is appropriate to offer genetic counseling (including discussion of potential risks to offspring and reproductive options) to young adults who are affected or at risk.
Prenatal testing
Prenatal diagnosis for pregnancies at increased risk is possible by analysis of DNA extracted from fetal cells obtained by amniocentesis usually performed at approximately 15–18 weeks' gestation or chorionic villus sampling at approximately 10–12 weeks' gestation. The disease-causing allele of a family member must be identified in the family before prenatal testing can be performed.
Preimplantation genetic diagnosis
Preimplantation genetic diagnosis may be available for families in which the disease-causing mutation has been identified.2
MOLECULAR GENETICS
RET proto-oncogene maps to 10q11.2 and encodes the receptor tyrosine kinase REarranged during Transfection protein.
Molecular genetic pathogenesis
RET encodes a tyrosine kinase receptor that plays an integral role in transducing signals for growth and differentiation in tissues derived from the neural crest. Gain-of-function mutations that produce a constitutively active protein or decreased specificity for its substrate cause MEN 2.90 In contrast, loss-of-function mutations are associated with a subset of HSCR.1
Normal allelic variants
The RET proto-oncogene is composed of 21 exons spanning more than 55 kb of genomic sequence.
Normal allelic variants and variants of uncertain significance have been described. A database of normal, uncertain, and pathologic RET variants is maintained by ARUP Laboratories (http://www.arup.utah.edu/database/MEN2/MEN2_welcome.php).91 The variants p.S649L and p.Y791F were recently reclassified as nonpathogenic, although whether they act as modifiers of risk is unknown.62
Pathologic allelic variants
The major disease-causing mutations are nonconservative gain-of-function substitutions located in one of six cysteine codons in the extracellular domain of the encoded protein.86,92 They include codons 609, 611, 618, and 620 in exon 10 and codons 630 and 634 in exon 11. All these variants have been identified in families with MEN 2A, and some have been identified in families with FMTC. Mutations in these sites have been detected in 98% of families with MEN 2A.3
Approximately 95% of all individuals with the MEN 2B phenotype have a single point mutation in the tyrosine kinase domain of the RET gene at codon 918 in exon 16, which substitutes a threonine for methionine.3 A second point mutation at codon 883 has been found in 2–3% of individuals with MEN 2B.93,94 Tandem RET mutations of codons 805, 806, and 904 in cis configuration with the p.V804M mutation have also been reported in individuals with MEN 2B.2,95–97
Normal gene product
RET produces a receptor tyrosine kinase with extracellular, transmembrane, and intracellular domains. The extracellular domain consists of a calcium-binding cadherin-like region and a cysteine-rich region. The encoded protein plays a role in signal transduction by interaction with the glial-derived neurotropic factor (GDNF) family of ligands: GDNF, neurturin, persephin, and artemin. Ligand interaction is by the ligand-binding GDNF family receptors to which RET protein binds the encoded protein complexes. Formation of a complex containing two RET protein molecules leads to RET autophosphorylation and intracellular signaling whereby phosphorylated tyrosines become docking sites for intracellular signaling proteins.98 The RET tyrosine kinase catalytic core, which is located in the intracellular domain, interacts with the docking protein FRS2 and causes downstream activation of the mitogen-activated protein kinase signaling cascade.99 Normal tissues contain transcripts of several lengths.100
Abnormal gene product
Mutations in codons in the cysteine-rich extracellular domain (609, 611, 618, 620, and 634) cause ligand-independent RET dimerization, leading to constitutive activation (i.e., gain of function) of tyrosine kinase.101
The disease-causing point mutation codon 918 that causes 95% of the MEN 2B phenotype lies within the substrate specificity pocket of the catalytic core of the tyrosine kinase and causes both a constitutive activation (i.e., gain of function) and perhaps loss of substrate specificity of the RET kinase in its monomeric state, independent of the normal ligand-binding and dimerization steps.101
In contrast to the activating mutations in MEN 2, mutations that cause HSCR result in a decrease in the transforming activity of RET.102 For families in which MEN 2A and HSCR cosegregate, models to explain how the same mutation can cause gain of function and loss of function have been proposed.103
REFERENCES
Zbuk KM, Eng C . Cancer phenomics: RET and PTEN as illustrative models. Nat Rev Cancer 2007; 7: 35–45.
Kloos RT, Eng C, Evans DB, et al. Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid 2009; 19: 565–612.
Eng C, Clayton D, Schuffenecker I, et al. The relationship between specific RET proto-oncogene mutations and disease phenotype in multiple endocrine neoplasia type 2. International RET mutation consortium analysis. JAMA 1996; 276: 1575–1579.
Cohen MS, Moley JF . Surgical treatment of medullary thyroid carcinoma. J Intern Med 2003; 253: 616–626.
DeLellis R, Lloyd RV, Heitz PU, Eng C . Pathology and genetics: tumours of the endocrine organs. World Health Organization classification of tumours. Oxford, UK: Oxford University Press, 2004.
Ponder BA, Ponder MA, Coffey R, et al. Risk estimation and screening in families of patients with medullary thyroid carcinoma. Lancet 1988; 1: 397–401.
Inabnet WB, Caragliano P, Pertsemlidis D . Pheochromocytoma: inherited associations, bilaterality, and cortex preservation. Surgery 2000; 128: 1007–1011; discussion 1011–1002.
Rodriguez JM, Balsalobre M, Ponce JL, et al. Pheochromocytoma in MEN 2A syndrome. Study of 54 patients. World J Surg 2008; 32: 2520–2526.
Frank-Raue K, Rybicki LA, Erlic Z, et al. Risk profiles and penetrance estimations in multiple endocrine neoplasia type 2A caused by germline RET mutations located in exon 10. Hum Mutat 2011; 32: 51–58.
Pomares FJ, Canas R, Rodriguez JM, Hernandez AM, Parrilla P, Tebar FJ . Differences between sporadic and multiple endocrine neoplasia type 2A phaeochromocytoma. Clin Endocrinol (Oxf) 1998; 48: 195–200.
Pacak K, Ilias I, Adams KT, Eisenhofer G . Biochemical diagnosis, localization and management of pheochromocytoma: focus on multiple endocrine neoplasia type 2 in relation to other hereditary syndromes and sporadic forms of the tumour. J Intern Med 2005; 257: 60–68.
Modigliani E, Vasen HM, Raue K, et al. Pheochromocytoma in multiple endocrine neoplasia type 2: European study. The Euromen Study Group. J Intern Med 1995; 238: 363–367.
Neumann HP, Bausch B, McWhinney SR, et al. Germ-line mutations in nonsyndromic pheochromocytoma. N Engl J Med 2002; 346: 1459–1466.
Brandi ML, Gagel RF, Angeli A, et al. Guidelines for diagnosis and therapy of MEN type 1 and type 2. J Clin Endocrinol Metab 2001; 86: 5658–5671.
Schuffenecker I, Virally-Monod M, Brohet R, et al. Risk and penetrance of primary hyperparathyroidism in multiple endocrine neoplasia type 2A families with mutations at codon 634 of the RET proto-oncogene. Groupe D'etude des Tumeurs a Calcitonine. J Clin Endocrinol Metab 1998; 83: 487–491.
Gagel RF, Levy ML, Donovan DT, Alford BR, Wheeler T, Tschen JA . Multiple endocrine neoplasia type 2a associated with cutaneous lichen amyloidosis. Ann Intern Med 1989; 111: 802–806.
Seri M, Celli I, Betsos N, Claudiani F, Camera G, Romeo G . A Cys634Gly substitution of the RET proto-oncogene in a family with recurrence of multiple endocrine neoplasia type 2A and cutaneous lichen amyloidosis. Clin Genet 1997; 51: 86–90.
Ceccherini I, Romei C, Barone V, et al. Identification of the Cys634–>Tyr mutation of the RET proto-oncogene in a pedigree with multiple endocrine neoplasia type 2A and localized cutaneous lichen amyloidosis. J Endocrinol Invest 1994; 17: 201–204.
Machens A, Dralle H . Multiple endocrine neoplasia type 2 and the RET protooncogene: from bedside to bench to bedside. Mol Cell Endocrinol 2006; 247: 34–40.
Machens A, Gimm O, Hinze R, Hoppner W, Boehm BO, Dralle H . Genotype-phenotype correlations in hereditary medullary thyroid carcinoma: oncological features and biochemical properties. J Clin Endocrinol Metab 2001; 86: 1104–1109.
Skinner MA, DeBenedetti MK, Moley JF, Norton JA, Wells SA Jr . Medullary thyroid carcinoma in children with multiple endocrine neoplasia types 2A and 2B. J Pediatr Surg 1996; 31: 177–181; discussion 181–172.
Wray CJ, Rich TA, Waguespack SG, Lee JE, Perrier ND, Evans DB . Failure to recognize multiple endocrine neoplasia 2B: more common than we think?. Ann Surg Oncol 2008; 15: 293–301.
Farndon JR, Leight GS, Dilley WG, et al. Familial medullary thyroid carcinoma without associated endocrinopathies: a distinct clinical entity. Br J Surg 1986; 73: 278–281.
Machens A, Niccoli-Sire P, Hoegel J, et al. Early malignant progression of hereditary medullary thyroid cancer. N Engl J Med 2003; 349: 1517–1525.
LiVolsi VA . C cell hyperplasia/neoplasia. J Clin Endocrinol Metab 1997; 82: 39–41.
Costante G, Meringolo D, Durante C, et al. Predictive value of serum calcitonin levels for preoperative diagnosis of medullary thyroid carcinoma in a cohort of 5817 consecutive patients with thyroid nodules. J Clin Endocrinol Metab 2007; 92: 450–455.
Ilias I, Pacak K . Diagnosis, localization and treatment of pheochromocytoma in MEN 2 syndrome. Endocr Regul 2009; 43: 89–93.
Ilias I, Chen CC, Carrasquillo JA, et al. Comparison of 6-18F-fluorodopamine PET with 123I-metaiodobenzylguanidine and 111in-pentetreotide scintigraphy in localization of nonmetastatic and metastatic pheochromocytoma. J Nucl Med 2008; 49: 1613–1619.
Brenner ME, Jacene HA . Recurrent or residual hyperparathyroidism and thyroid cancer effectively evaluated with scintigraphy. Otolaryngol Clin North Am 2008; 41: 1117–1133, viii-ix
Gimenez-Roqueplo AP, Lehnert H, Mannelli M, et al. Phaeochromocytoma, new genes and screening strategies. Clin Endocrinol (Oxf) 2006; 65: 699–705.
Erlic Z, Rybicki L, Peczkowska M, et al. Clinical predictors and algorithm for the genetic diagnosis of pheochromocytoma patients. Clin Cancer Res 2009; 15: 6378–6385.
Hansford JR, Mulligan LM . Multiple endocrine neoplasia type 2 and RET: from neoplasia to neurogenesis. J Med Genet 2000; 37: 817–827.
Boedeker CC, Erlic Z, Richard S, et al. Head and neck paragangliomas in von Hippel-Lindau disease and multiple endocrine neoplasia type 2. J Clin Endocrinol Metab 2009; 94: 1938–1944.
Angrist M, Kauffman E, Slaugenhaupt SA, et al. A gene for Hirschsprung disease (megacolon) in the pericentromeric region of human chromosome 10. Nat Genet 1993; 4: 351–356.
Lyonnet S, Bolino A, Pelet A, et al. A gene for Hirschsprung disease maps to the proximal long arm of chromosome 10. Nat Genet 1993; 4: 346–350.
Edery P, Lyonnet S, Mulligan LM, et al. Mutations of the RET proto-oncogene in Hirschsprung's disease. Nature 1994; 367: 378–380.
Romeo G, Ronchetto P, Luo Y, et al. Point mutations affecting the tyrosine kinase domain of the RET proto-oncogene in Hirschsprung's disease. Nature 1994; 367: 377–378.
Attie T, Pelet A, Edery P, et al. Diversity of RET proto-oncogene mutations in familial and sporadic Hirschsprung disease. Hum Mol Genet 1995; 4: 1381–1386.
Mulligan LM, Eng C, Attie T, et al. Diverse phenotypes associated with exon 10 mutations of the RET proto-oncogene. Hum Mol Genet 1994; 3: 2163–2167.
Pelet A, Geneste O, Edery P, et al. Various mechanisms cause RET-mediated signaling defects in Hirschsprung's disease. J Clin Invest 1998; 101: 1415–1423.
Bordeaux MC, Forcet C, Granger L, et al. The RET proto-oncogene induces apoptosis: a novel mechanism for Hirschsprung disease. EMBO J 2000; 19: 4056–4063.
Tallini G, Santoro M, Helie M, et al. RET/PTC oncogene activation defines a subset of papillary thyroid carcinomas lacking evidence of progression to poorly differentiated or undifferentiated tumor phenotypes. Clin Cancer Res 1998; 4: 287–294.
Santoro M, Papotti M, Chiappetta G, et al. RET activation and clinicopathologic features in poorly differentiated thyroid tumors. J Clin Endocrinol Metab 2002; 87: 370–379.
Brauckhoff M, Gimm O, Hinze R, Ukkat J, Brauckhoff K, Dralle H . Papillary thyroid carcinoma in patients with RET proto-oncogene germline mutation. Thyroid 2002; 12: 557–561.
Shifrin AL, Xenachis C, Fay A, Matulewicz TJ, Kuo YH, Vernick JJ . One hundred and seven family members with the rearranged during transfection V804M proto-oncogene mutation presenting with simultaneous medullary and papillary thyroid carcinomas, rare primary hyperparathyroidism, and no pheochromocytomas: is this a new syndrome–MEN 2C?. Surgery 2009; 146: 998–1005.
Fugazzola L, Cerutti N, Mannavola D, et al. Multigenerational familial medullary thyroid cancer (FMTC): evidence for FMTC phenocopies and association with papillary thyroid cancer. Clin Endocrinol (Oxf) 2002; 56: 53–63.
Yip L, Cote GJ, Shapiro SE, et al. Multiple endocrine neoplasia type 2: evaluation of the genotype-phenotype relationship. Arch Surg 2003; 138: 409–416; discussion 416.
Punales MK, Graf H, Gross JL, Maia AL . RET codon 634 mutations in multiple endocrine neoplasia type 2: variable clinical features and clinical outcome. J Clin Endocrinol Metab 2003; 88: 2644–2649.
Verga U, Fugazzola L, Cambiaghi S, et al. Frequent association between MEN 2A and cutaneous lichen amyloidosis. Clin Endocrinol (Oxf) 2003; 59: 156–161.
Gimm O, Neuberg DS, Marsh DJ, et al. Over-representation of a germline RET sequence variant in patients with sporadic medullary thyroid carcinoma and somatic RET codon 918 mutation. Oncogene 1999; 18: 1369–1373.
Decker RA, Peacock ML, Watson P . Hirschsprung disease in MEN 2A: increased spectrum of RET exon 10 genotypes and strong genotype-phenotype correlation. Hum Mol Genet 1998; 7: 129–134.
Romeo G, Ceccherini I, Celli J, et al. Association of multiple endocrine neoplasia type 2 and Hirschsprung disease. J Intern Med 1998; 243: 515–520.
Aiello A, Cioni K, Gobbo M, et al. The familial medullary thyroid carcinoma-associated RET E768D mutation in a multiple endocrine neoplasia type 2A case. Surgery 2005; 137: 574–576.
Jimenez C, Habra MA, Huang SC, et al. Pheochromocytoma and medullary thyroid carcinoma: a new genotype-phenotype correlation of the RET protooncogene 891 germline mutation. J Clin Endocrinol Metab 2004; 89: 4142–4145.
Gibelin H, Bezieau S, Misso C, Bouin-Pineau MH, Marechaud R, Kraimps JL . Germline RET V804M mutation associated with multiple endocrine neoplasia type 2A. Br J Surg 2004; 91: 1458–1459.
Hoie J, Heimdal K, Nesland JM, Bormer O . [Prophylactic thyroidectomy in carriers of RET oncogene mutation carriers]. Tidsskr Nor Laegeforen 2000; 120: 3249–3252.
Nilsson O, Tisell LE, Jansson S, Ahlman H, Gimm O, Eng C . Adrenal and extra-adrenal pheochromocytomas in a family with germline RET V804L mutation. JAMA 1999; 281: 1587–1588.
Feldman GL, Edmonds MW, Ainsworth PJ, et al. Variable expressivity of familial medullary thyroid carcinoma (FMTC) due to a RET V804M (GTG–>ATG) mutation. Surgery 2000; 128: 93–98.
Frohnauer MK, Decker RA . Update on the MEN 2A c804 RET mutation: is prophylactic thyroidectomy indicated? Surgery 2000; 128: 1052–1057; discussion 1057–1058.
Lecube A, Hernandez C, Oriola J, et al. V804M RET mutation and familial medullary thyroid carcinoma: report of a large family with expression of the disease only in the homozygous gene carriers. Surgery 2002; 131: 509–514.
Rothberg AE, Raymond VM, Gruber SB, Sisson J . Familial medullary thyroid carcinoma associated with cutaneous lichen amyloidosis. Thyroid 2009; 19: 651–655.
Erlic Z, Hoffmann MM, Sullivan M, et al. Pathogenicity of DNA variants and double mutations in multiple endocrine neoplasia type 2 and von Hippel-Lindau syndrome. J Clin Endocrinol Metab 2010; 95: 308–313.
Romei C, Cosci B, Renzini G, et al. RET genetic screening of sporadic medullary thyroid cancer (MTC) allows the pre-clinical diagnosis of unsuspected gene carriers and the identification of a relevant percentage of hidden Familial MTC (FMTC). Clin Endocrinol (Oxf) 2011; 74: 241–247.
Wohllk N, Cote GJ, Bugalho MM, et al. Relevance of RET proto-oncogene mutations in sporadic medullary thyroid carcinoma. J Clin Endocrinol Metab 1996; 81: 3740–3745.
Elisei R, Romei C, Cosci B, et al. RET genetic screening in patients with medullary thyroid cancer and their relatives: experience with 807 individuals at one center. J Clin Endocrinol Metab 2007; 92: 4725–4729.
Wiench M, Wygoda Z, Gubala E, et al. Estimation of risk of inherited medullary thyroid carcinoma in apparent sporadic patients. J Clin Oncol 2001; 19: 1374–1380.
Bryant J, Farmer J, Kessler LJ, Townsend RR, Nathanson KL . Pheochromocytoma: the expanding genetic differential diagnosis. J Natl Cancer Inst 2003; 95: 1196–1204.
Richards FM, Webster AR, McMahon R, Woodward ER, Rose S, Maher ER . Molecular genetic analysis of von Hippel-Lindau disease. J Intern Med 1998; 243: 527–533.
Baysal BE, Ferrell RE, Willett-Brozick JE, et al. Mutations in SDHD, a mitochondrial complex II gene, in hereditary paraganglioma. Science 2000; 287: 848–851.
Astuti D, Latif F, Dallol A, et al. Gene mutations in the succinate dehydrogenase subunit SDHB cause susceptibility to familial pheochromocytoma and to familial paraganglioma. Am J Hum Genet 2001; 69: 49–54.
Boedeker CC, Neumann HP, Offergeld C, et al. Clinical features of paraganglioma syndromes. Skull Base 2009; 19: 17–25.
Bausch B, Borozdin W, Neumann HP . Clinical and genetic characteristics of patients with neurofibromatosis type 1 and pheochromocytoma. N Engl J Med 2006; 354: 2729–2731.
Eng C, Marsh DJ, Robinson BG, et al. Germline RET codon 918 mutation in apparently isolated intestinal ganglioneuromatosis. J Clin Endocrinol Metab 1998; 83: 4191–4194.
Heald B, Mester J, Rybicki L, Orloff MS, Burke CA, Eng C . Frequent gastrointestinal polyps and colorectal adenocarcinomas in a prospective series of PTEN mutation carriers. Gastroenterology 2010; 139: 1927–1933.
Hobert JA, Eng C . PTEN hamartoma tumor syndrome: an overview. Genet Med 2009; 11: 687–694.
Thway K, Fisher C . Diffuse ganglioneuromatosis in small intestine associated with neurofibromatosis type 1. Ann Diagn Pathol 2009; 13: 50–54.
Moley JF, Debenedetti MK, Dilley WG, Tisell LE, Wells SA . Surgical management of patients with persistent or recurrent medullary thyroid cancer. J Intern Med 1998; 243: 521–526.
Kahraman T, de Groot JW, Rouwe C, et al. Acceptable age for prophylactic surgery in children with multiple endocrine neoplasia type 2a. Eur J Surg Oncol 2003; 29: 331–335.
Szinnai G, Meier C, Komminoth P, Zumsteg UW . Review of multiple endocrine neoplasia type 2A in children: therapeutic results of early thyroidectomy and prognostic value of codon analysis. Pediatrics 2003; 111: E132–E139.
Nguyen L, Niccoli-Sire P, Caron P, et al. Pheochromocytoma in multiple endocrine neoplasia type 2: a prospective study. Eur J Endocrinol 2001; 144: 37–44.
Lee NC, Norton JA . Multiple endocrine neoplasia type 2B—genetic basis and clinical expression. Surg Oncol 2000; 9: 111–118.
Eisenhofer G, Rivers G, Rosas AL, Quezado Z, Manger WM, Pacak K . Adverse drug reactions in patients with phaeochromocytoma: incidence, prevention and management. Drug Saf 2007; 30: 1031–1062.
American Society of Clinical Oncology. American Society of Clinical Oncology policy statement update: genetic testing for cancer susceptibility. J Clin Oncol 2003; 21: 2397–2406.
Wells SA Jr, Gosnell JE, Gagel RF, et al. Vandetanib for the treatment of patients with locally advanced or metastatic hereditary medullary thyroid cancer. J Clin Oncol 2010; 28: 767–772.
Schuffenecker I, Ginet N, Goldgar D, et al. Prevalence and parental origin of de novo RET mutations in multiple endocrine neoplasia type 2A and familial medullary thyroid carcinoma. Le Groupe d'Etude des Tumeurs a Calcitonine. Am J Hum Genet 1997; 60: 233–237.
Mulligan LM, Eng C, Healey CS, et al. Specific mutations of the RET proto-oncogene are related to disease phenotype in MEN 2A and FMTC. Nat Genet 1994; 6: 70–74.
Carlson KM, Bracamontes J, Jackson CE, et al. Parent-of-origin effects in multiple endocrine neoplasia type 2B. Am J Hum Genet 1994; 55: 1076–1082.
Kitamura Y, Goodfellow PJ, Shimizu K, et al. Novel germline RET proto-oncogene mutations associated with medullary thyroid carcinoma (MTC): mutation analysis in Japanese patients with MTC. Oncogene 1997; 14: 3103–3106.
Massoll N, Mazzaferri EL . Diagnosis and management of medullary thyroid carcinoma. Clin Lab Med 2004; 24: 49–83.
Santoro M, Carlomagno F, Romano A, et al. Activation of RET as a dominant transforming gene by germline mutations of MEN2A and MEN2B. Science 1995; 267: 381–383.
Margraf RL, Crockett DK, Krautscheid PM, et al. Multiple endocrine neoplasia type 2 RET protooncogene database: repository of MEN2-associated RET sequence variation and reference for genotype/phenotype correlations. Hum Mutat 2009; 30: 548–556.
Mulligan LM, Kwok JB, Healey CS, et al. Germ-line mutations of the RET proto-oncogene in multiple endocrine neoplasia type 2A. Nature 1993; 363: 458–460.
Gimm O, Marsh DJ, Andrew SD, et al. Germline dinucleotide mutation in codon 883 of the RET proto-oncogene in multiple endocrine neoplasia type 2B without codon 918 mutation. J Clin Endocrinol Metab 1997; 82: 3902–3904.
Smith DP, Houghton C, Ponder BA . Germline mutation of RET codon 883 in two cases of de novo MEN 2B. Oncogene 1997; 15: 1213–1217.
Miyauchi A, Futami H, Hai N, et al. Two germline missense mutations at codons 804 and 806 of the RET proto-oncogene in the same allele in a patient with multiple endocrine neoplasia type 2B without codon 918 mutation. Jpn J Cancer Res 1999; 90: 1–5.
Cranston AN, Carniti C, Oakhill K, et al. RET is constitutively activated by novel tandem mutations that alter the active site resulting in multiple endocrine neoplasia type 2B. Cancer Res 2006; 66: 10179–10187.
Menko FH, van der Luijt RB, de Valk IA, et al. Atypical MEN type 2B associated with two germline RET mutations on the same allele not involving codon 918. J Clin Endocrinol Metab 2002; 87: 393–397.
Santoro M, Melillo RM, Carlomagno F, Vecchio G, Fusco A . Minireview: RET: normal and abnormal functions. Endocrinology 2004; 145: 5448–5451.
Manie S, Santoro M, Fusco A, Billaud M . The RET receptor: function in development and dysfunction in congenital malformation. Trends Genet 2001; 17: 580–589.
Takaya K, Yoshimasa T, Arai H, et al. Expression of the RET proto-oncogene in normal human tissues, pheochromocytomas, and other tumors of neural crest origin. J Mol Med 1996; 74: 617–621.
Takahashi M, Asai N, Iwashita T, Murakami H, Ito S . Molecular mechanisms of development of multiple endocrine neoplasia 2 by RET mutations. J Intern Med 1998; 243: 509–513.
Iwashita T, Murakami H, Asai N, Takahashi M . Mechanism of ret dysfunction by Hirschsprung mutations affecting its extracellular domain. Hum Mol Genet 1996; 5: 1577–1580.
Takahashi M, Iwashita T, Santoro M, Lyonnet S, Lenoir GM, Billaud M . Co-segregation of MEN2 and Hirschsprung's disease: the same mutation of RET with both gain and loss-of-function?. Hum Mutat 1999; 13: 331–336.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Moline, J., Eng, C. Multiple endocrine neoplasia type 2: An overview. Genet Med 13, 755–764 (2011). https://doi.org/10.1097/GIM.0b013e318216cc6d
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e318216cc6d
Keywords
This article is cited by
-
Patients’ perception on the quality of care for multiple endocrine neoplasia disorders in Europe: an online survey from a patient support group
Endocrine (2021)
-
Pediatric applications of Dotatate: early diagnostic and therapeutic experience
Pediatric Radiology (2020)
-
Occurrence of paratesticular ganglioneuroma 18 years after concurrent adrenal ganglioneuroma and papillary thyroid carcinoma – a case report
BMC Cancer (2019)