Abstract
The IFNL4 gene is negatively associated with spontaneous and treatment-induced clearance of hepatitis C virus infection. The activity of IFNλ4 has an important causal role in the pathogenesis, but the molecular details are not fully understood. One possible reason for the detrimental effect of IFNλ4 could be a tissue-specific regulation of an unknown subset of genes. To address both tissue and subtype specificity in the interferon response, we treated primary human hepatocytes and airway epithelial cells with IFNα, IFNλ3 or IFNλ4 and assessed interferon mediated gene regulation using transcriptome sequencing. Our data show a surprisingly similar response to all three subtypes of interferon. We also addressed the tissue specificity of the response, and identified a subset of tissue-specific genes. However, the interferon response is robust in both tissues with the majority of the identified genes being regulated in hepatocytes as well as airway epithelial cells. Thus we provide an in-depth analysis of the liver interferon response seen over an array of interferon subtypes and compare it to the response in the lung epithelium.
Similar content being viewed by others
Introduction
Tissue-specific responses to the different interferon (IFN) subtypes are poorly understood, and the vast majority of studies are performed using cell lines. Cell lines provide a highly homogeneous cell population allowing for the generation of data with little noise. However, cancer-derived cell lines do not necessarily provide the best picture of the in vivo IFN response. Primary cells, on the other hand, resemble the in vivo situation much better. The lung epithelium is exposed to the environment and thus to frequent viral infections, although most respiratory infections are transient in nature. In contrast, viruses need to overcome several barriers to reach and infect the hepatocytes in the liver. Nevertheless, once a viral infection is established in the liver it can cause significant pathogenicity. Viral hepatitis is frequently caused by the two RNA viruses, hepatitis A virus (family Picornaviridae) and hepatitis C virus (HCV; family Flaviviridae), as well as by the DNA virus hepatitis B virus (family Hepadnaviridae).
Humans possess three types of IFNs: type I, II, and III. Type II IFN (IFNγ) is called an interferon for historical reasons; it signals via the formation of STAT1 homodimers and only has limited direct antiviral activity but has potent proinflammatory activities. For simplicity, it will not be further addressed here. Type I and type III IFNs (the latter are also known as IFNλs) signal through distinct receptor complexes. The type I IFN receptor is composed of the IFNAR1 and IFNAR2 receptor chains.1, 2 These receptor chains are universally expressed on all nucleated cells and therefore type I IFNs possess a systemic effect when produced in adequate amounts. Type III IFNs signal through a receptor complex consisting of the IFNλR1 (IL28RA)-specific chain and the shared IL10R2 (IL10Rβ) chain.3, 4 Expression of IFNλR1 is rather restricted, with epithelial tissues and the liver showing the most prominent expression in humans.5, 6 This restricted expression of IFNλR1 implies that IFNλ can target tissues of high risk for viral infection without the detrimental effect caused by a systemic type I IFN response. Despite using different receptor complexes, both type I and type III IFN can induce activation of the transcription factor IFN-stimulated gene factor 3 (ISGF3) and therefore regulate a highly overlapping set of genes.7, 8, 9 However, the kinetics of the response can be rather different.10, 11
Genome-wide association studies have identified several single nucleotide polymorphisms (SNPs) within the IFNλ loci as powerful predictors of HCV treatment outcome as well as of spontaneous clearance of HCV infections.12, 13, 14, 15, 16 Recently, IFNλ4, a novel member of the IFNλ family, was identified.17 The IFNL4 gene encodes a protein with only 29% sequence identity to IFNλ3. Nevertheless, the IFNλ4 protein is fully active and can signal through the canonical IFNλ receptor complex.18 Paradoxically, a frameshift mutation disrupting translation of the IFNL4 mRNA (rs368234815TT) is strongly correlated with improved HCV clearance, both treatment induced and spontaneous.17, 19 Furthermore, a direct correlation between the activity of the IFNλ4 protein and poor HCV clearance was recently demonstrated.20 Thus, despite being highly antiviral in vitro, having a functional IFNL4 gene is disadvantageous during HCV infection. The malicious effect of IFNλ4 might extend to other chronic viral infections, as recent data suggest for cytomegalovirus infection.21, 22 The paradoxical situation that an apparent antiviral cytokine is disadvantageous during viral infection, and the current inability to explain why this effect is specific to IFNλ4, has spurred speculation toward alternative signaling pathways of IFNλ4.23
In order to determine whether IFNλ4 can induce an alternative set of genes, that are not induced in the classical IFN response, we have compared the transcriptional response after IFNα, IFNλ3 and IFNλ4 stimulation in both primary human hepatocytes (PHH) and primary human airway epithelial (HAE) cells using transcriptome sequencing (RNA-seq). We chose epithelial cells because they represent a first line of defense, where type III IFNs have a major role and hepatocytes because the detrimental effect of IFNλ4 has been described for pathogenesis of HCV infection. The gene induction pattern of the three IFN subtypes was found to be remarkably similar, with a core set of 68 genes induced by all three IFNs in both cell types. Moreover, we identified putative tissue-specific genes that are differentially regulated in the HAE compared to the PHH cells upon IFN treatment.
Results
IFN responses in primary human cells
We established cultures of PHH24 and primary HAE cells.25 The two systems were chosen as the respective primary cells originate from tissues that are of biological relevance for type III IFN. Both tissues respond well to both type I and type III IFNs, thus allowing us to compare the tissue- and IFN-type specific responses. PHH and HAE were cultured and stimulated with IFN for 6 h.
A major obstacle in using primary cells is the inherent donor-to-donor variation. We sought to overcome this by using cells from several donors and by applying relatively strict statistical selection criteria. In brief, these are a minimum of 2-fold induction or 1.5-fold repression and a maximal P-value of 0.05 (see Materials and methods for details). Table 1 lists the number of significantly regulated genes in both tissues. Globally, in PHH and HAE cells, more genes meet the inclusion criteria for IFNα than for IFNλ. This is not surprising as several prior studies have shown a stronger response to IFNα than to IFNλ, but both types of IFN fundamentally target the same set of genes through activation of the transcription factor ISGF3.7, 8, 9, 10, 11 Finally, the number of significantly induced genes is higher in HAE cells than in PHH. This is largely owing to the fact that the donor-to-donor variation is substantially lower in the HAE cultures, compared with the PHH cultures, resulting in fewer genes being rejected due to poor P-values. Of note, the lung-derived cells are cultured for several weeks between the surgery and the IFN treatment, whereas the PHH are typically treated 24 h after liver resection. This longer culture period of the HAE cells, which is necessary to obtain a pseudostratified epithelium, might render them more homogenous and blur donor-to-donor differences, explaining the better P-values.
We then chose to focus on a set of robustly regulated genes, requiring a gene to meet the selection criteria for at least three of the six experiments (three IFNs tested in two distinct primary cell culture systems), resulting in 122 genes (Supplementary Table 1). Of those, 68 genes are induced by all three IFNs and in both tissues. Overall we observe little qualitative difference between the different subtypes of IFN used, but type I IFN (IFNα) shows a stronger response with more genes meeting the threshold for significance.
IFNλ4 induces a classical IFN signature
Figure 1 shows scatter plots of gene expression change caused by IFNλ4 versus IFNα (Figure 1) or versus IFNλ3 treatment (Figure 1). Black dots represent genes that are significantly induced by both treatments. Orange dots represent genes that meet the selection criteria for IFNλ4 but not for the IFN used for comparison (IFNα or IFNλ3), and thus represent potential IFNλ4-specific genes. Blue dots are genes meeting the selection criteria for either IFNα (Figure 1) or IFNλ3 (Figure 1), but not for IFNλ4. Identification of genes that are specifically regulated by IFNλ4 is of particular interest to reconcile the apparent paradox between the antiviral activity of IFNλ4 against HCV18 and unfavorable in vivo effects on HCV infection and treatment outcome.17
IFNλ4 induces a classical IFN response in primary liver and lung cells. The IFNλ4 gene regulation profile is compared with IFNα (top row) or to IFNλ3 (bottom row) in both PHH (left column) and HAE cells (right column). Each point in the scatter plots corresponds to a unique gene. The expression of each gene was deduced from the number of its mRNA reads; fold change (FC) values are relative to the mock-treated control and were plotted in log2 scale. Genes that are significantly regulated in both conditions are depicted in black whereas genes that are only significantly regulated by one of the two IFNs are shown in blue (y axis) or orange (x axis). Nonsignificant genes are depicted in gray. The vertical and horizontal dotted lines indicate a 2-fold positive and a 1.5-fold negative change in expression, respectively.
The scatter plots in Figure 1 show a strikingly similar response to IFNα and IFNλ4 (Figure 1), with the majority of regulated genes appearing on the diagonal. Furthermore, the responses to IFNλ3 and IFNλ4 are highly similar (Figure 1). Although several genes appear as IFNλ4-specific in the scatter plots (orange dots), they are on average induced to similar levels by both types of IFNs (dots on or close to the diagonal). Lack of significance for IFNα and/or IFNλ3 is owing to high donor-to-donor variability. Most of the concerned genes are known IFN-stimulated genes (ISGs) and we do not detect any genes that are reliably induced by IFNλ4 only. Thus, IFNλ4 shows a classical IFN signature virtually identical to that of IFNλ3 in both PHH and HAE cells.
There is an abundance of IFNα-specific genes (Figure 1, Table 1). However, this is likely owing to the statistical bias of our stringent significance thresholds. Indeed, the overall broader amplitude of the IFNα-mediated ISG stimulation results in more genes meeting the selection criteria. This stronger IFNα response has been observed by others and might be caused by the choice of an early analysis time point (6 h treatment), which underestimates the slower IFNλ response.10, 11 Furthermore, both HAE and PHH show a substantial higher mRNA expression for the type I IFN receptor complex compared with the type III receptor (see below). Consistent with this, most IFNα-specific genes are close to the diagonal. The few genes that showed no apparent regulation by IFNλ4 in PHH (along the y axis in Figure 1) have very low expression values (data not shown). Altogether, there is a nearly complete overlap between the IFNα, λ3 and λ4 IFN-regulated genes (We use the term IFN-regulated genes (IRGs) to cover all genes, both positively and negatively regulated, whereas term ISGs in its traditional sense refers to the genes induced by IFNs).
Tissue-specific IFN responses
We then compared the IFN response of PHH and HAE cells (Figure 2). In general, there was a robust IFN induction in both tissues, with the majority of IRGs being induced in a similar manner (black dots, Figure 2). However, a number of genes were only significantly induced in one of the two cell types (blue and orange dots, Figure 2). An even higher correlation between PHH and HAE responses was reached when comparing the mean expression values in PHH and HAE cells, in the basal or IFN-induced conditions (Figure 3).
Comparison of the IFN responses in primary liver and lung cells. Scatter plots comparing the response of PHH and HAE cells to IFNα (left), λ3 (middle) or λ4 (right). Shown are mean logFC gene expression values. Genes significantly altered upon IFN stimulation in both tissues are depicted in black, genes significantly regulated only in HAE cells in blue, and genes significantly regulated only in PHH are shown in orange. Remaining genes are plotted in gray.
Comparison of the absolute gene expression in primary liver and lung cells. IRGs are highlighted. These scatter plots compare the absolute gene expression (RPKM) in PHH vs HAE cells, in mock-treated cells (top-left) or 6 h after IFNα (top-right), λ3 (bottom-left) or λ4 (bottom-right) induction. Genes in black are significantly regulated in both tissues; genes in blue and orange are significantly regulated only in HAE or PHH cells, respectively.
To analyze possible tissue-specific effects of IFNs more in-depth, we manually inspected the raw expression data for all of the 122 genes previously found to be robustly induced by IFN (Supplementary Table 1). Among these, we observed a subset of genes that displayed various degrees of tissue specificity. We categorized genes as tissue specific by taking both the level of induction as well as absolute expression levels into account. In addition, we focused on genes that had an acceptable level of donor-to-donor variation. These genes are listed in Table 2. Only two IRGs were expressed in a liver-specific manner: ANGPTL1 and APOL3. Both of these genes showed higher induction levels as well as higher absolute expression levels in the liver. ACO1 was slightly repressed in liver cells, but strongly repressed in HAE cells. LY6E, WARS, AIM2 and IDO1 were all induced to a higher level and had a higher absolute expression in HAE cells. Interestingly, both WARS and IDO1 modify the tryptophan biogenesis pathway. The next group, TNFSF13B, ZBP1, IFITM1 and IFI27, showed significant induction in both tissues but strongest induction and higher absolute expression in HAE cells. HRASLS2, HSH2D and IFI16 showed a more mixed phenotype. All had a higher absolute expression in the lung cells, but were also induced in the liver cells by IFNα, whereas their induction by IFNλ varied. IRF9, LAMP3 and MX2 displayed higher fold induction in the liver cells but higher absolute expression levels in lung cells.
To verify our manual selection of tissue-specific genes, we performed an additional automated differential gene expression analysis, this time looking for differences in expression between the two tissues for the same IFN treatment (and not comparing control versus IFN as in the first analysis). Importantly, all our manually selected genes were detected as being significantly differently expressed between the two tissues for each of the three IFNs in this second analysis (data not shown).
As analyzed with the Interferome database human chromosome location and transcription factor analysis tools,26 no obvious features such as clustering of the genes on the human genome or common promoter motif could explain this tissue specificity.
Expression of IFN receptors
Naturally, the response to a given IFN depends upon the receptor expression and therefore we mined the data for expression values of both the receptors for type I and type III IFNs. We focused our analysis on the two high-affinity receptor chains. Both of these have a complex splice pattern with the potential to express multiple isoforms of the receptor chain. However, one of the strengths of the transcriptome sequencing approach is that it allows for precise determination of the splice pattern and provides a quantitative measurement of the different splice variants detected. Figure 4 shows the possible protein isoforms originating from the canonical mRNAs and their observed expression levels. The observed splice variants corresponded to the canonical splice forms found in the literature (Figure 4a).3, 4, 27 We also tested the signaling ability of all three isoforms of the IFNλR1 receptor chain (Figure 4b). IFNλR1-1 encodes the full-length protein and is signaling competent. IFNλR1-2, which lacks the juxtamembrane region, but retains the transmembrane domain and most of the intracellular part, is incapable of signaling in our assay. IFNλR1-3, encodes a protein which is truncated upstream of the transmembrane domain and has a changed amino-acid composition at the C-terminus. This isoform is assumed to be secreted in a soluble form and in vitro data suggest that it can act as a negative regulator of type III IFN signaling.28 We noted an overall low expression of the IFNλR1 receptor chain in both tissues, with splice variant 1 and 3 being expressed at approximately the same level and splice variant 2 at a slightly lower level in HAE (Figure 4c). The IFNλR1 chain was reported to be induced by IFN in liver cells.29 We see a trend toward an increased expression of splice variant 1 in PHH but not HAE following IFN treatment, but this did not reach statistical significance at the α=0.05 level (data not shown). It is possible that the chosen time point was not optimal to observe a significant induction of the IFNLR1 mRNA.
IFN receptor expression in primary liver and lung cells. (a) Protein isoforms originating from the different protein coding sequences of the detected IFNLR1 and IFNAR2 mRNAs. Numbers refer to the numbering of the exons in the longest protein isoforms. (b) Signaling capacity of IFNλR1 isoforms measured in HEK293 cells transiently transfected with the pEF2 vector containing IFNλR1 splice variants, as well as Renilla and firefly luciferase reporters 24 h before IFN treatment. The firefly construct is IFN inducible, whereas the Renilla construct is constitutively expressed and is used for normalization. Experiments were performed in triplicates. Mean and s.d. are shown. (c) Expression levels of IFNLR1 splice variants, (d) IFNAR2 splice variants and (e) IL10R2 in PHH and HAE cells; fragments per kilobase of exon per million fragments mapped (FPKM). Identified mRNAs for IFNAR2 corresponded to: NM_207584, NM_000874, and NM_207585.
Interestingly, three similar protein isoforms have also been described for the IFNAR2 chain, as a result of differential splicing (Figure 4a).30 The full-length isoform 1 (also called IFNAR2c or IFNAR2-2) is required for signaling.30 This isoform is expressed in both tissues at levels ~10-fold higher than seen for full-length IFNλR1, which could explain the stronger and more robust response to IFNα (Figure 4d). Isoform 2 (also called IFNAR2b or IFNAR2-1) has been reported to act as a dominant negative regulator,31, 32 and its mRNA is expressed at two times higher level than the full-length receptor. Finally, the soluble isoform 3 (also called IFNAR2a or IFNAR2-3) that has previously been shown to possess either agonistic or antagonistic properties in mice depending on the experimental setup tested,33 was not detected in both PHH and HAE cells.
The expression level of IL10R2 was ~12 times higher in HAE cells compared with hepatocytes (Figure 4e). This increased expression could be caused by the fact that the IL10R2 chain is shared with other cytokines, which could have an important role during viral infections of the respiratory system. For example, IL-22, which utilizes IL10R2 for signaling, is the key cytokine responsible for the regeneration of tracheal epithelial cells during influenza virus infection.34
Discussion and conclusion
RNA-seq offers a unique opportunity to survey whole transcriptomes in a high-throughput and quantitative manner.35 We used this powerful technique to analyze the IFN response in primary cell cultures derived from liver and lung of different donors. We induced HAE and PHH cultures with three different IFNs, IFNα2b, IFNλ3 and IFNλ4, allowing us to perform two fundamentally different comparisons. We compared responses with different types of IFN within a given tissue, as well as responses to the same type of IFN but in different tissues. Overall, this analysis revealed IFN responses as very robust with little tissue specificity. Nevertheless, small but significant differences were observed between PHH and HAE in their response to IFN. Furthermore, we observed a remarkably similar response to the three different subtypes of IFN tested.
Compared with a recently published microarray analysis of type I and type III IFN responses in PHH, which used similar statistical thresholds but substantially higher IFNλ concentrations than our study (1000 ng ml−1),11 our RNA-seq data provide a more complete estimate of the IFN response (87 versus 50 genes significantly regulated by IFNλ3). In the HAE cultures, we identified 345 genes significantly induced by IFNα2b, 110 by IFNλ3 and 124 by IFNλ4. The larger number of significantly activated IRGs in the HAE cultures is largely an effect of the lower donor-to-donor variability in this system, which results in more genes reaching statistical significance. We compared our results with those of other published transcriptome analyses of PHH and in general the RNA-seq methods found more genes than microarray-based methods.10, 11
To our knowledge this study is the first to fully analyze the transcriptome of HAE cultures in response to IFN. The epithelium is one of the primary target tissues for type III IFNs. In mice, control of several epithelial infections is impaired in IFNλR1 deficient animals. This is the case for both respiratory infections such as SARS coronavirus and influenza A virus, as well as for the intestinal rotavirus infection.36, 37 As expected, our analyses revealed a powerful IFN response in HAE. IFNα responses were stronger than IFNλ responses at the doses we used, but we could not detect any fundamental difference in the induced gene sets. Previous studies in cell lines using chromosome immunoprecipitation experiments showed that signaling of both type I and type III IFN converges at the transcription factor ISGF3.9 This model is supported by the very similar gene induction profile that both we and others find in PHH and HAE for the different types of IFN tested.
The IFNL4 gene has an important role during HCV infection, and by means which are not fully understood yet, only the functional variant of the gene impairs clearance of HCV, both spontaneous and treatment induced.17, 19, 38 Despite the negative influence on HCV clearance, the gene product of IFNL4, IFNλ4, is highly antiviral and induces a typical IFN response.18 However, whereas the initial analyses of the IFNλ4 protein showed that it could signal through the IFNλR1:IL10R2 receptor complex, the experiments did not rule out any additional signaling abilities. We therefore compared genes induced by IFNλ3 and IFNλ4 in both HAE and PHH. This analysis did not reveal any genes that were both specifically and significantly regulated by IFNλ4. It is thus unlikely that IFNλ4 prevents HCV clearance by an alternative, non-IFN signaling pathway.
Owing to its immense absorptive area and high ventilation rate, the respiratory tract is the most common route of viral entry. We analyzed tissue-based differences in the IFN responses by manually inspecting all the 122 genes that we had classified as significantly regulated by IFN. Here we looked for differences in both the relative expression after IFN treatment (fold change) and absolute expression levels. There was surprisingly little difference in the IFN responses between the two tissue types. Nevertheless, a small subset of genes exhibits a tissue dependent response to type I and type III IFNs (Table 2). However, this analysis establishes detailed signatures of IFN-induced changes in gene regulation of primary human lung and liver cells. This information should be useful for guiding future research to explore IFN-regulated effector mechanisms relevant for controlling viral infections in these tissues.
Materials and methods
IFN sources and concentrations
IFNα2b was obtained from SP Europe/Essex Pharma (IntronA) or from Sigma-Aldrich (Steinheim, Germany; I4401). His-tagged IFNλ3 and λ4 were produced and purified as previously described.18, 39 IFNα was used at 100 U ml−1 and IFNλs at 10 ng ml−1.
IFN treatment of primary human hepatocytes
PHHs were obtained from Primacyt (Schwerin, Germany) or from the Primary Human Hepatocyte Core Facility at the Hannover Medical School (Hannover, Germany). We did not observe any systematic variation between the two sources of PHH. We used a low-speed centrifugation (50 g) to purify the hepatocytes and the resulting purity of hepatocyte preparations is higher than 95%. Cells were seeded in 6-well dishes on collagen directly after surgery.24 Twenty-four hours post seeding, the PHHs were induced for 6 h with IFNs or PBS (mock control) diluted in hepatocyte culture medium (HCM, Lonza, Walkersville, MD, USA). The cells were then lysed in 1 ml Trizol reagent (Invitrogen, Karlsruhe, Germany) per well. Total RNA extraction was performed according to the manufacturer’s instructions (Trizol reagent) with the addition of 10 μg glycogen per sample to facilitate the RNA precipitation.
IFN treatment of primary HAE cells
Primary human tracheobronchial cells were isolated from three different donors as described elsewhere.25 Isolated HAE cells obtained from these donors were seeded in 24-well permeable supports (Corning, CLS3396, pore size 0.4 μm) and maintained for 4 weeks until cultures were well differentiated as described.25 The HAE cell cultures were induced from the basolateral side for 6 or 24 h with exogenous recombinant human IFNs or PBS (mock) diluted in air-liquid interface medium. Total RNA from induced HAE cultures was isolated using Qiagen’s RNeasy Kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocols.
Transcriptome analysis using RNA-Seq
Quality and integrity of the total RNA was controlled on an Agilent Technologies 2100 Bioanalyzer (Agilent Technologies; Waldbronn, Germany). The RNA sequencing library was generated from 100 ng total RNA using TruSeq RNA Sample Prep Kits v2 (Illumina, San Diego, CA, USA) for mRNA purification followed by ScriptSeq v2 RNA-Seq Library Preparation Kit (Epicentre, Illumina) according to manufacturer’s protocols. The libraries were sequenced on Illumina HiSeq2500 (Illumina), using TruSeq SBS Kit v3-HS (Illumina) (50 cycles, single ended run) with an average of 3 × 107 reads per RNA sample. Reads were aligned to the reference genome using open source short read aligner Tophat40 followed by Cufflinks41 that assembles transcripts, estimates their abundances, and tests for differential expression and regulation.
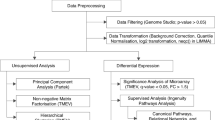
Differential expression analysis of RNA-seq data on the gene level
HTSeq-count with parameters m=intersection-strict, s=no, and t=exon was used to produce raw read counts of expression for each gene.42 We used the following three state-of-the-art R packages for differential expression analysis on the gene level: DESeq,43 edgeR44 and limma. For DESeq and edgeR we used the raw read counts as input, whereas for limma we transformed them via its internal voom function prior to the differential expression analysis.45 In each analysis we used the following criteria for hit calling: a fold change of at least 2 for induction or 1.5 for repression in gene expression, and an FDR-adjusted P-value of 0.05 or better. With the aim of reducing false-positive hits, we required a gene to be selected by at least two of the three programs.
Sample size and power estimation
To assess the sensitivity of the applied methods to identify differentially expressed genes in the context of the observed donor-to-donor variability, we estimated necessary sample sizes for given power and fold change as well as the power for given fold change and sample size using the R package RNASeqPower.46 The following parameter values were estimated based on all genes with a read count per million reads mapped of at least one in the control samples for both HAE and PHH: (i) the average coverage of a gene (depth parameter was 2007 (HAE) and 1830 (PHH); (ii) the average coefficient of variation of read counts (cv parameter) was 0.16 (HAE) and 0.41 (PHH); and (iii) the false discovery rate α was set to 0.05. Estimated sample sizes for different fold-change values and a power of 0.8 and 0.9 are shown in Supplementary Table 2. Moreover, to detect a fold change of two with a sample size of three (the number of biological replicates in our study) the estimated power is 0.78, 1.0 and 0.54 for comparisons of HAE vs PHH, HAE vs HAE and PHH vs PHH, respectively.
Activity assay in HEK293 cells
HEK293 cells were seeded at a density of 1.5 × 105 cells per well in a 24-well plate and left to rest for 24 h. After 24 h, the cells were transfected with the pEF2 plasmid encoding one of the IFNλR1 splice variants, firefly luciferase under the control of the Mx1 promoter47 and Renilla luciferase under the control of the β-actin promoter. Twenty-four hours post-transfection, cells were induced in triplicates with 10 ng ml−1 of IFNλ3 or left untreated. Twenty-four hours after induction, the cells were washed with PBS and lysed with Passive Lysis Buffer (Promega, Madison, WI, USA). The lysates were spun down at 10 000 g for 2 min at 4 °C, and the cleared lysates were used for the measurement of luciferase activity (Dual-Luciferase Reporter Assay System, Promega).
References
Mogensen KE, Lewerenz M, Reboul J, Lutfalla G, Uze G . The type I interferon receptor: structure, function, and evolution of a family business. J Interferon Cytokine Res 1999; 19: 1069–1098.
Stark GR, Kerr IM, Williams BR, Silverman RH, Schreiber RD . How cells respond to interferons. Annu Rev Biochem 1998; 67: 227–264.
Kotenko SV, Gallagher G, Baurin VV, Lewis-Antes A, Shen M, Shah NK et al. IFN-lambdas mediate antiviral protection through a distinct class II cytokine receptor complex. Nat Immunol 2003; 4: 69–77.
Sheppard P, Kindsvogel W, Xu W, Henderson K, Schlutsmeyer S, Whitmore TE et al. IL-28, IL-29 and their class II cytokine receptor IL-28R. Nat Immunol 2003; 4: 63–68.
Hermant P, Demarez C, Mahlakoiv T, Staeheli P, Meuleman P, Michiels T . Human but not mouse hepatocytes respond to interferon-lambda in vivo. PLoS One 2014; 9: e87906.
Sommereyns C, Paul S, Staeheli P, Michiels T . IFN-lambda (IFN-lambda) is expressed in a tissue-dependent fashion and primarily acts on epithelial cells in vivo. PLoS Pathog 2008; 4: e1000017.
Doyle SE, Schreckhise H, Khuu-Duong K, Henderson K, Rosler R, Storey H et al. Interleukin-29 uses a type 1 interferon-like program to promote antiviral responses in human hepatocytes. Hepatology (Baltimore, Md) 2006; 44: 896–906.
Marcello T, Grakoui A, Barba-Spaeth G, Machlin ES, Kotenko SV, Macdonald MR et al. Interferons alpha and lambda inhibit hepatitis C virus replication with distinct signal transduction and gene regulation kinetics. Gastroenterology 2006; 131: 1887–1898.
Zhou Z, Hamming OJ, Ank N, Paludan SR, Nielsen AL, Hartmann R . Type III interferon (IFN) induces a type I IFN-like response in a restricted subset of cells through signaling pathways involving both the Jak-STAT pathway and the mitogen-activated protein kinases. J Virol 2007; 81: 7749–7758.
Bolen CR, Ding S, Robek MD, Kleinstein SH . Dynamic expression profiling of type I and type III interferon-stimulated hepatocytes reveals a stable hierarchy of gene expression. Hepatology (Baltimore, Md) 2014; 59: 1262–1272.
Jilg N, Lin W, Hong J, Schaefer EA, Wolski D, Meixong J et al. Kinetic differences in the induction of interferon stimulated genes by interferon-alpha and interleukin 28B are altered by infection with hepatitis C virus. Hepatology (Baltimore, Md) 2014; 59: 1250–1261.
Ge D, Fellay J, Thompson AJ, Simon JS, Shianna KV, Urban TJ et al. Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance. Nature 2009; 461: 399–401.
Rauch A, Kutalik Z, Descombes P, Cai T, Di Iulio J, Mueller T et al. Genetic variation in IL28B is associated with chronic hepatitis C and treatment failure: a genome-wide association study. Gastroenterology 2010; 138: 1338–1345 1345 e1–e7.
Suppiah V, Moldovan M, Ahlenstiel G, Berg T, Weltman M, Abate ML et al. IL28B is associated with response to chronic hepatitis C interferon-alpha and ribavirin therapy. Nat Genet 2009; 41: 1100–1104.
Tanaka Y, Nishida N, Sugiyama M, Kurosaki M, Matsuura K, Sakamoto N et al. Genome-wide association of IL28B with response to pegylated interferon-alpha and ribavirin therapy for chronic hepatitis C. Nat Genet 2009; 41: 1105–1109.
Thomas DL, Thio CL, Martin MP, Qi Y, Ge D, O'Huigin C et al. Genetic variation in IL28B and spontaneous clearance of hepatitis C virus. Nature 2009; 461: 798–801.
Prokunina-Olsson L, Muchmore B, Tang W, Pfeiffer RM, Park H, Dickensheets H et al. A variant upstream of IFNL3 (IL28B) creating a new interferon gene IFNL4 is associated with impaired clearance of hepatitis C virus. Nat Genet 2013; 45: 164–171.
Hamming OJ, Terczynska-Dyla E, Vieyres G, Dijkman R, Jorgensen SE, Akhtar H et al. Interferon lambda 4 signals via the IFNlambda receptor to regulate antiviral activity against HCV and coronaviruses. EMBO J 2013; 32: 3055–3065.
Bibert S, Roger T, Calandra T, Bochud M, Cerny A, Semmo N et al. IL28B expression depends on a novel TT/-G polymorphism which improves HCV clearance prediction. J Exp Med 2013; 210: 1109–1116.
Terczynska-Dyla E, Bibert S, Duong FH, Krol I, Jorgensen S, Collinet E et al. Reduced IFNlambda4 activity is associated with improved HCV clearance and reduced expression of interferon-stimulated genes. Nat Commun 2014; 5: 5699.
Bibert S, Wojtowicz A, Taffe P, Manuel O, Bernasconi E, Furrer H et al. The IFNL3/4 DeltaG variant increases susceptibility to cytomegalovirus retinitis among HIV-infected patients. AIDS 2014; 28: 1885–1889.
Manuel O, Wojtowicz A, Bibert S, Mueller NJ, van Delden C, Hirsch HH et al. Influence of IFNL3/4 Polymorphisms on the Incidence of Cytomegalovirus Infection After Solid-Organ Transplantation. J Infect Dis 2014; 211: 906–914.
Booth D, George J . Loss of function of the new interferon IFN-lambda4 may confer protection from hepatitis C. Nat Genet 2013; 45: 119–120.
Kleine M, Riemer M, Krech T, DeTemple D, Jager MD, Lehner F et al. Explanted diseased livers - a possible source of metabolic competent primary human hepatocytes. PLoS One 2014; 9: e101386.
Dijkman R, Jebbink MF, Koekkoek SM, Deijs M, Jonsdottir HR, Molenkamp R et al. Isolation and characterization of current human coronavirus strains in primary human epithelial cell cultures reveal differences in target cell tropism. J Virol 2013; 87: 6081–6090.
Rusinova I, Forster S, Yu S, Kannan A, Masse M, Cumming H et al. Interferome v2.0: an updated database of annotated interferon-regulated genes. Nucleic Acids Res 2013; 41 (Database issue): D1040–D1046.
Dumoutier L, Lejeune D, Hor S, Fickenscher H, Renauld JC . Cloning of a new type II cytokine receptor activating signal transducer and activator of transcription (STAT)1, STAT2 and STAT3. Biochem J 2003; 370 (Pt 2): 391–396.
Witte K, Gruetz G, Volk HD, Looman AC, Asadullah K, Sterry W et al. Despite IFN-lambda receptor expression, blood immune cells, but not keratinocytes or melanocytes, have an impaired response to type III interferons: implications for therapeutic applications of these cytokines. Genes Immun 2009; 10: 702–714.
Duong FH, Trincucci G, Boldanova T, Calabrese D, Campana B, Krol I et al. IFN-lambda receptor 1 expression is induced in chronic hepatitis C and correlates with the IFN-lambda3 genotype and with nonresponsiveness to IFN-alpha therapies. J Exp Med 2014; 211: 857–868.
Lutfalla G, Holland SJ, Cinato E, Monneron D, Reboul J, Rogers NC et al. Mutant U5A cells are complemented by an interferon-alpha beta receptor subunit generated by alternative processing of a new member of a cytokine receptor gene cluster. EMBO J 1995; 14: 5100–5108.
Pfeffer LM, Basu L, Pfeffer SR, Yang CH, Murti A, Russell-Harde D et al. The short form of the interferon alpha/beta receptor chain 2 acts as a dominant negative for type I interferon action. J Biol Chem 1997; 272: 11002–11005.
Gazziola C, Cordani N, Carta S, De Lorenzo E, Colombatti A, Perris R . The relative endogenous expression levels of the IFNAR2 isoforms influence the cytostatic and pro-apoptotic effect of IFNalpha on pleomorphic sarcoma cells. Int J Oncol 2005; 26: 129–140.
Hardy MP, Owczarek CM, Trajanovska S, Liu X, Kola I, Hertzog PJ . The soluble murine type I interferon receptor Ifnar-2 is present in serum, is independently regulated, and has both agonistic and antagonistic properties. Blood 2001; 97: 473–482.
Kumar P, Thakar MS, Ouyang W, Malarkannan S . IL-22 from conventional NK cells is epithelial regenerative and inflammation protective during influenza infection. Mucosal Immunol 2013; 6: 69–82.
Wang Z, Gerstein M, Snyder M . RNA-Seq: a revolutionary tool for transcriptomics. Nature reviews. Genetics 2009; 10: 57–63.
Mordstein M, Neugebauer E, Ditt V, Jessen B, Rieger T, Falcone V et al. Lambda interferon renders epithelial cells of the respiratory and gastrointestinal tracts resistant to viral infections. J Virol 2010; 84: 5670–5677.
Pott J, Mahlakoiv T, Mordstein M, Duerr CU, Michiels T, Stockinger S et al. IFN-lambda determines the intestinal epithelial antiviral host defense. Proc Natl Acad Sci USA 2011; 108: 7944–7949.
Aka PV, Kuniholm MH, Pfeiffer RM, Wang AS, Tang W, Chen S et al. Association of the IFNL4-DeltaG Allele With Impaired Spontaneous Clearance of Hepatitis C Virus. The Journal of infectious diseases 2014; 209: 350–354.
Dellgren C, Gad HH, Hamming OJ, Melchjorsen J, Hartmann R . Human interferon-lambda3 is a potent member of the type III interferon family. Genes Immun 2009; 10: 125–131.
Kim D, Pertea G, Trapnell C, Pimentel H, Kelley R, Salzberg SL . TopHat2: accurate alignment of transcriptomes in the presence of insertions, deletions and gene fusions. Genome Biol 2013; 14: R36.
Trapnell C, Williams BA, Pertea G, Mortazavi A, Kwan G, van Baren MJ et al. Transcript assembly and quantification by RNA-Seq reveals unannotated transcripts and isoform switching during cell differentiation. Nat Biotechnol 2010; 28: 511–515.
Anders S, Pyl PT, Huber W . HTSeq — A Python framework to work with high-throughput sequencing data. Bioinformatics 2014; 31: 166–169.
Anders S, Huber W . Differential expression analysis for sequence count data. Genome Biol 2010; 11: R106.
Robinson MD, McCarthy DJ, Smyth GK . edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics 2010; 26: 139–140.
Law CW, Chen Y, Shi W, Smyth GK . voom: precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol 2014; 15: R29.
Hart SN, Therneau TM, Zhang Y, Poland GA, Kocher JP . Calculating sample size estimates for RNA sequencing data. J Comput Biol 2013; 20: 970–978.
Jorns C, Holzinger D, Thimme R, Spangenberg HC, Weidmann M, Rasenack J et al. Rapid and simple detection of IFN-neutralizing antibodies in chronic hepatitis C non-responsive to IFN-alpha. J Med Virol 2006; 78: 74–82.
Acknowledgements
We are grateful to Sergei Kotenko for the gift of the pEF2-IFNλR1 plasmid. RH is supported by the Danish Cancer Society (grant R20-A927) and the Danish Council for Independent Research, Medical Research (grant 11-107588). TP is supported by Deutsche Forschungsgemeinschaft (DFG) Sonderforschungsbereiche (SFB) 900, (project A6), Deutsches Zentrum für Infektionsforschung and grant from the Initiative and Networking Fund of the Helmholtz Association (SO-024). FWRV is supported by Deutsches Zentrum für Infektionsforschung. V.T. and R.D. are supported by Swiss National Science Foundation, (project nr. 149784).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Genes and Immunity website
Supplementary information
Rights and permissions
About this article
Cite this article
Lauber, C., Vieyres, G., Terczyńska-Dyla, E. et al. Transcriptome analysis reveals a classical interferon signature induced by IFNλ4 in human primary cells. Genes Immun 16, 414–421 (2015). https://doi.org/10.1038/gene.2015.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gene.2015.23
This article is cited by
-
Establishment of well-differentiated camelid airway cultures to study Middle East respiratory syndrome coronavirus
Scientific Reports (2022)
-
Distinct molecular phenotypes involving several human diseases are induced by IFN-λ3 and IFN-λ4 in monocyte-derived macrophages
Genes & Immunity (2022)
-
The role of IFNL4 in liver inflammation and progression of fibrosis
Genes & Immunity (2022)
-
IFN-λ4 potently blocks IFN-α signalling by ISG15 and USP18 in hepatitis C virus infection
Scientific Reports (2017)
-
IFN-λ3, not IFN-λ4, likely mediates IFNL3–IFNL4 haplotype–dependent hepatic inflammation and fibrosis
Nature Genetics (2017)