Abstract
Purpose
To evaluate effects of intravitreal ranibizumab and bevacizumab administration on ambulatory blood pressure monitoring (ABPM) recordings in normotensive patients with age-related macular degeneration (AMD).
Patients and methods
A total of 72 patients (mean age: 61.8(6.2) years, 52.8% were females) diagnosed with AMD were included in this study as divided into ranibizumab (n=34) and bevacizumab (n=38) treatment groups. Twenty-four hour, nighttime, and daytime ABMP values for systolic and diastolic BP were recorded in study groups before and after the third intravitreal injection of ranibizumab or bevacizumab.
Results
Ranibizumab injection had no impact on ABPM recordings and dipping status. In the bevacizumab group, increased daytime (129.0(6.6) vs 127.7(6.6) mm Hg, P=0.002) and nighttime systolic (116.9(7.5) vs 112.6(7.1) mmHg, p<0.001) BP and decreased daytime diastolic (80.1(6.5) vs 82.4(6.1)mm Hg, P=0.001) BP were noted in the post-injection period. Also, percentage of non-dippers was significantly increased from 5.3% at pre-injection to 28.9% (P=0.004) at the post-injection period.
Conclusion
In conclusion, given that it has no significant impact on ABPM recordings and dipping status, in our study, intravitreal ranibizumab injection may be the better choice in the management of AMD.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the leading cause of severe irreversible vision loss related to choroidal neovascularization (CNV) in the elderly.1, 2, 3
Intravitreal administration of anti-vascular endothelial growth factor (VEGF) agents, including ranibizumab (Lucentis; Genentech, San Francisco, CA, USA) and bevacizumab (Avastin; Genentech) have become widely used in the management of CNV in patients with AMD.4, 5
Ranibizumab was initially approved in the US for the treatment of neovascular (wet) AMD in 2006 followed by approvals for retinal vein occlusion in June 2010, and for diabetic macular edema in August 2012. However, bevacizumab is not US Food and Drug Administration-approved for intraocular use, but is widely used off-label for the treatment of neovascular and exudative ocular diseases since May 2005.5, 6, 7
Ranibizumab has been reported to improve vision in at least 41% of the 0.5-mg-treated group and 34% of the 0.3-mg-treated group, and to improve visual acuity within a range of 7.2–11.3 letters for the entire spectrum of CNV8, 9 and well tolerated in patients with AMD.10
In contrast to high-dose systemic intravenous bevacizumab application that was associated with hypertension and an increase in thromboembolic risk,11 intravitreal bevacizumab injection has been reported to be a safer procedure in terms of blood pressure (BP) for both hypertensive and normotensive patients.12, 13, 14, 15 However, several cases of acute elevation of systemic BP, cerebrovascular accidents, myocardial infarction, and transient ischemic attack were also reported.4, 16, 17, 18, 19
Although the mechanism of hypertension due to anti-angiogenic therapy is not yet elucidated, nitric oxide (NO)-related mechanisms has been considered in the pathogenesis on the basis of VEGF-mediated increased endothelial NO synthase expression by activation of protein kinase C pathway, leading to an increase in arterial pressure.20
High nocturnal BP in older patients has been associated with increased risk of cardiovascular complications,21 while blunted nocturnal decline in BP has been linked to the accelerated hypertensive target organ damage, as well as increased vascular morbidity and mortality.22, 23, 24, 25, 26 Ambulatory blood pressure monitoring (ABPM) has been considered to be more advantageous than office measurement of BP in terms of identification of nocturnal decline in BP levels as well as higher consistency reported with target organ damage.27 Given that majority of patients with AMD are seniors with other comorbidities, increased BP values in particular,15 studying the impact of intravitreal anti-VEGF agents on the dipper and non-dipper categorizations of BP profiles among AMD patients may help physicians to be well-informed about the potential risks of these agents and thus to base their use on firm scientific rationale and sound medical evidence.15, 28, 29
In the light of the above-mentioned points, this study was designed to evaluate short-term effects of intravitreal ranibizumab and bevacizumab administration on 24-h ABPM recordings in normotensive patients with AMD.
Materials and methods
Study population
A total of 72 patients (mean age: 61.8 (SD:6.2, ranged 53–81) years, 52.8% were females) diagnosed with increased central retinal thickness due to wet AMD on optical coherence tomography were included in this study, as divided into two groups according to type of intravitreal anti-VEGF injections applied, including ranibizumab (n=34) and bevacizumab (n=38) treatment groups.
Patients with AMD-related increased central retinal thickness, characterized by subretinal fluid and/or cystic changes within the retina, and findings of choroidal neovascular membrane on fluorescein fundus angiography were included in the present study. Patients with co-morbid hypertension or concomitant antihypertensive treatment were excluded from the study, while patients with systolic/diastolic BP levels of >140/90 mm Hg (Grade 1 hypertension according to European Society of Hypertension (ESH)/European Society of Cardiology (ESC) guidelines)30 at baseline were referred to the internal medicine department for further investigation and excluded from the study, if they were prescribed with an antihypertensive medication.
Written informed consent was obtained from each subject following a detailed explanation of the objectives and protocol of the study, which was conducted in accordance with the ethical principles stated in the ‘Declaration of Helsinki’ and approved by the institutional ethics committee.
Study parameters
The data on patient demographics and ophthalmic examination findings were recorded in each patient. Twenty-four hour, nighttime and daytime ABMP values for systolic and diastolic BP levels were recorded in ranibizumab and bevacizumab treatment groups before (pre-injection) and after (post-injection) the third intravitreal injection of ranibizumab or bevacizumab.
Ophthalmic procedures
This prospective, randomised study was carried out between December 2013 and December 2015. Both intravitreal injection types were explained to patients in detail. At enrollment, patients were randomized sequentially by a blinded study coordinator to the ranibizumab and bevacizumab group after informed consent was obtained.
At each visit, patients were routinely evaluated for visual acuity using Snellen chart as well as ophthalmic examination, including slitlamp and biomicroscopic fundus examination. Ocular imaging consisted of fluorescein angiography and/or optical coherence tomography at the time of ranibizumab injection and at each visit.
Only one eye of each patient was injected with ranibizumab or bevacizumab. Antibiotic eye drops were not used prior to administration. All eyes received a single dose of ranibizumab or bevacizumab. First, the eye was topically anesthetized with 0.5% propacaine and povidoneiodine (10%) scrub was performed on the eyelids and lashes. Then, a sterile speculum was placed between the lids and povidone-iodine (5%) drops were applied over the ocular surface three times. Additional topical anesthesia was achieved by applying a sterile cotton swab soaked in sterile 4% lidocaine to the area designated for injection in the inferotemporal quadrant. Ranibizumab (Lucentis, Genentech) or bevacizumab (Avastin, Genentech) were injected through the pars plana into the vitreous cavity inserted into the sclera 3–4 mm posterior to the limbus using a 30-gauge needle attached to a tuberculin syringe. Following the procedure, light perception was evaluated and the intraocular pressure was monitored until it was below 21 mm Hg. Then, the patients were instructed to apply topical antibiotics to the injected eye four times a day for 1 week. All patients received a phone call within 24 h to check their health status and were reminded to use their antibiotic drops as prescribed.
ABPM recordings
BP levels were recorded before and after the third intravitreal injection of ranibizumab or bevacizumab, based on single-measurement via manual auscultatory technique in the non-dominant arm prior to injection and 24-h ABPM using a portable noninvasive recording device (Model 90207, Spacelabs, Inc. Redmond, Washington, DC, USA) 24-h before and after the injection. All patients were graded according to pre-and post-injection values for overall, nighttime and daytime systolic and diastolic BP levels. Manual auscultatory BP measurements were done in cardiology service by the same physician in the same conditions and blood pressure determination was blinded from treating physician.
Twenty-four hour ABPM was obtained with BP readings set at 20 min intervals (06:00 AM – 24:00 PM) and at 30 min intervals (24:00 PM – 06:00 AM) ABPM. Patients were asked to continue with their normal daily routine and to record when they went to sleep and when they woke up. The data were transferred to a computer and loaded into ABPM report management system software for the final analysis using ABPM-FIT program (University of Heidelberg, Germany, version 2.2). For each 24-h measurement, mean systolic and diastolic BP levels were evaluated separately for daytime and nighttime periods. Arterial daytime and nocturnal hypertension were diagnosed according to the criteria of the according to ESH/ESC guidelines30 (systolic BP ≥140 mm Hg and/or diastolic BP ≥90 mm Hg, systolic BP >120 mm Hg and diastolic BP >70 mm Hg). The non-dominant arm was the site of cuff placement for ABPM. The ambulatory monitor had to agree with a mercury column sphygmomanometer to within 7 mm Hg, while patients with failure of ≥25% of BP recordings on a daily basis were not subjected to final analysis.
Definition of dippers and non-dippers
Time in bed was defined based on the patient-kept diary that documented the exact time of getting into and arising from bed. The average BP for this time in bed was calculated from the ambulatory monitoring data (termed nighttime BP). Daytime BP was defined as the BP during the remainder of the 24-h period. The percentage decline in nighttime BP was calculated as follows: 100 × (1- nighttime mean SBP/ daytime mean SBP). Patients with a decline in nighttime BP of <10% were considered to be non-dippers.25
Statistical analysis
Statistical analysis was made using MedCalc Statistical Software version 12.7.7 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2013). χ2 test and McNemar test were used for the comparison of the categorical data, while the numerical data were analyzed using paired sample t-test. The data were expressed as ‘mean (SD)’ and percent (%), where appropriate. P<0.05 was considered statistically significant.
Results
Pre-and post-injection values for ABPM in treatment groups
Overall, pre-injection and post-injection ABPM values for 24-h, nighttime and daytime systolic and diastolic BP were similar in the ranibizumab group (Table 1).
In the bevacizumab group, post-injection values for 24-h systolic (124.8(6.5) vs 122.5(6.7)mm Hg, P=0.001), daytime systolic (129.0(6.6) vs 127.7(6.6) mm Hg, P=0.002) and nighttime systolic (116.9(7.5) vs 112.6(7.1) mm Hg, P<0.001) BP were significantly higher as compared with pre-injection values. Post-injection values for 24-h diastolic (77.3(6.2) vs 79.1(6.1) mm Hg, P=0.003) and daytime diastolic (80.1(6.5) vs 82.4(6.1) mmHg, p=0.001) BP were significantly lower as compared with pre-injection values, whereas no significant difference was observed in pre-injection vs post-injection values in terms of nighttime diastolic BP (Table 1).
Dipping status in the pre-injection and post-injection periods with respect to treatment groups
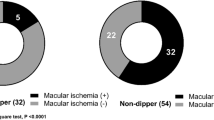
Ranibizumab injection had no significant impact on dipping status with similar percentage of dippers (94.1 and 88.2%) and non-dippers (5.9 and 11.8%) in the pre-injection and post-injection periods, respectively (Table 2).
Bevacizumab injection had significant impact on dipping status with significant increase in the percentage of non-dippers from 5.3% at pre-injection to 28.9% (P=0.004) at the post-injection period (Table 2).
Ranibizumab and bevacizumab groups were similar in terms of percentage of non-dippers patients in the pre-injection (5.9 vs 5.3%, respectively, P=0.6867) and post-injection (11.8 vs 28.9%, respectively, P=0.1354) periods (Table 2).
Safety of intravitreal anti-VEGF administration
Both in ranibizumab and bevacizumab groups, one patient experienced sub-conjunctival hemorrhage 2 days after third injection of bevacizumab, which was resolved in three weeks without medication.
Discussion
Our findings in a cohort of normotensive AMD patients who received the third intravitreal anti-VEGF injections of ranibizumab or bevacizumab revealed no significant impact of intravitreal ranibizumab administration on ABPM recordings and dipping status. Intravitreal bevacizumab injection on the other hand was associated with increased levels of 24-h, daytime and nighttime systolic BP and decreased levels of 24-h and daytime diastolic BP as well as increased percentage of non-dippers.
Earlier diastolic BP response to an intravitreal bevacizumab injection was reported in normotensive than in hypertensive patients with AMD. The fact that blood vessels in the normotensive population have preserved their physiological function in terms of vasodilatation and vasoconstriction has suggested them to respond more promptly to an intravitreal bevacizumab injection.15
Accordingly, bevacizumab was associated with increased systolic BP at both daytime and nighttime recordings, while decreased diastolic BP only in daytime recordings in our cohort. An international intravitreal bevacizumab safety survey reported that 0.21% of the patients (n=15) experienced a mild increase in BP following bevacizumab administration.4 Likewise, mild elevation of systolic BP after systemic bevacizumab administration for neovascular AMD was reported by Michels et al.31 Also, Rich et al32 monitored the BP for 3 months after intravitreal bevacizumab administration for the treatment of neovascular AMD and reported that the mean systolic BP increased from 131 mm Hg at baseline to 148 mm Hg at month 1, while the mean diastolic BP (80 mm Hg) remained unchanged along with no apparent change in systolic and diastolic BP levels at month 2.
Evaluation of the effects of intravitreal injection of bevacizumab on systemic BP changes in hypertensive or normotensive group of patients with exudative form of AMD by Risimic et al15 revealed no significant changes in systolic BP in either the hypertensive or the normotensive group of participants over the entire 6 weeks follow-up period. Also, significant decline in diastolic BP levels was reported 7 days after the intravitreal bevacizumab injection in the hypertensive group, while only 1 h after bevacizumab injection in the normotensive group, and both resolved 6 weeks after drug administration and not observed in later checkups.15
Failure to identify any significant alteration in BP levels as well as in the short-term BP regulation under antiangiogenic therapy in some studies has been associated with the fact that frequency of BP elevation is a function of treatment duration.33, 34
We have recently described the increased BP levels via intravitreal bevacizumab similarly in hypertensive and normotensive patients 3 weeks after the intravitreal bevacizumab injection. Also, we have reported the normalization of BP levels at week-6 in normotensive patients, while persistence of high BP levels in some of the hypertensive patients that may be associated with the clearance of the drug from the systemic circulation.35
Significant dose-dependent increase in risk of hypertension in patients who received bevacizumab was also reported along with findings on a uniform decrease in hypertension by the cessation of therapy.20 In studies on the relation of systemic bevacizumab treatment to BP in oncology patients, the median interval to incident hypertension was estimated at 4.5–6 months from initiation of bevacizumab therapy.36, 37 Considering intravitreal application of the agent, bevacizumab injection has been considered to be safe in terms of BP changes over 6 weeks post administration and thus regular follow-up for 6 weeks has been recommended for the prompt recognition and early treatment of individuals with altered BP values.15
Accordingly, our findings in bevacizumab group support the mild elevation of BP after bevacizumab demonstrated in previous studies,4, 31, 32 while given that changes in ABPM recordings were based on measurements taken after the third intravitreal injection in the present cohort, our finding seem not to support the normalization of BP changes at least after 6 weeks,15, 35 8 weeks,32 or 12 weeks4, 31 of injection reported in other cohorts.
Nevertheless, it should be noted that in relation to lack of a standard and systematic method of measuring parameters such as BP and other adverse events following the intravitreal administration of bevacizumab, observer bias has been assumed to be considerably high.15, 38
On the basis of a positive correlation between more severe hypertension and higher VEGF in hypertensive patients,39 which seems a paradoxical finding since lower serum VEGF levels might predispose to a hypertensive state, hypertension has been considered likely to be a disease of inappropriate response to angiogenic growth factors (AGF).40 This seems consistent with the hypothesis that higher levels of VEGF are produced in response to endothelial trauma and that improved BP control would lead to reduced VEGF levels.39
The mechanism of action of bevacizumab as a VEGF inhibitor has been considered to include the diminished synthesis of NO, a vasodilator, which leads to increase in peripheral resistance and, ultimately, increase in BP.20, 41, 42 Using bolus injections of VEGF to stimulate angiogenesis was reported to be associated with potentially lethal levels of hypotension, which was ameliorated by the use of lower doses of VEGF intravenously by Yang et al.43, 44
Given the consistently reported dose-dependency of VEGF-induced NO release,43, 44 we preferred to evaluate the effects of intravitreal anti-VEGF agents on BP among patients after the third injection. Consistent with the postulation of NO-mediated pathways in the pathogenesis of hypertension due to anti-angiogenic therapy20 and the likelihood of a central role of endothelial dysfunction in the development of VEGF-induced hypertension, we observed a higher frequency of an abnormal BP profile at night after systemic bevacizumab administration.
Reduction in blood-VEGF levels in the first day post-intravitreal bevacizumab injection was reported to be associated with detection of bevacizumab in the systemic blood circulation and thus the potential systemic effects.45 Hence, insufficient decline in nighttime BP in bevacizumab rather than ranibizumab in the present study may be associated with the longer systemic half-life of bevacizumab as compared with ranibizumab.46 This finding seems notable, given the consistently reported association between a non-dipper BP profile and an increased risk of target organ damage at the cardiac, renal, vascular, and cerebrovascular levels in several studies involving subjects with uncomplicated essential hypertension.22, 23, 24, 25, 26 Increased nighttime systolic BP under bevacizumab treatment in our cohort is also worth noting, given the consideration of high nocturnal BP in older patients with systolic hypertension to be a potent predictor of subsequent cardiovascular complications.21
Since majority of patients with AMD are seniors with other comorbidities, increased BP values in particular, paying special attention to this specific population has been suggested when considering bevacizumab treatment, given the likelihood of an eventual additional increase in BP.15
While the two treatment groups did not differ significantly with respect to their effect on the dipping status, this seems likely to be associated with small sample size of the study. Accordingly, on the basis of no influence on normal nighttime decline in BP levels, ranibizumab seems to be a safer therapeutic option in patients with family history of hypertension and require multiple consecutive intravitreal anti-VEGF injections.
In conclusion, our findings in a cohort of normotensive patients with subfoveal choroidal neovascularization due to AMD revealed intravitreal bevacizumab injection to be associated with increased daytime and nighttime systolic BP, decreased daytime diastolic BP and increased percentage of non-dippers. In this regard, given that it has no significant impact on 24-h, daytime and nighttime ABPM recordings as well as on dipping status, intravitreal ranibizumab injection seems to offer a safer therapeutic option in the management of AMD, particularly for patients with family history of hypertension and require multiple intravitreal anti-VEGF injections. Additionally, our findings emphasize the beneficial role of 24-h ABMP monitoring in comprehensive evaluation of BP status, and thereby prompt identification and early intervention of complications in patients undergoing intravitreal anti-VEGF administration, particularly for patients with hypertension and high risk of cardiovascular side effects. The effects of anti-VEGF agents on BP should be investigated in longer-term studies to be able to appropriately address the dose dependency and maintenance of BP alterations.

References
Bressler NM, Bressler SB, Fine SL . Age-related macular degeneration. Surv Ophthalmol 1988; 32: 375–413.
Bressler NM, Bressler SB, Congdon NG, Ferris FL 3rd, Friedman DS, Klein R et al. Potential public health impact of Age-Related Eye Disease Study results: AREDS report no. 11. Arch Ophthalmol 2003; 121: 1621–1624.
Ferris FL 3rd, Fine SL, Hyman L . Age-related macular degeneration and blindness due to neovascular maculopathy. Arch Ophthalmol 1984; 102: 1640–1642.
Fung AE, Rosenfeld PJ, Reichel E . The ınternational ıntravitreal bevacizumab safety survey: using the Internet to assess drug safety worldwide. Br J Ophthalmol 2006; 90: 1344–1349.
Kiss S, Liu Y, Brown J, Holekamp NM, Almony A, Campbell J et al. Clinical utilization of anti-vascular endothelial growth-factor agents and patient monitoring in retinal vein occlusion and diabetic macular edema. Clin Ophthalmol 2014; 8: 1611–1621.
Rosenfeld PJ, Fung AE, Puliafito CA . Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for macular edema from central retinal vein occlusion. Ophthalmic Surg Lasers Imaging 2005; 36: 336–339.
Rosenfeld PJ, Moshfeghi AA, Puliafito CA . Optical coherence tomography findings after an intravitreal injection of bevacizumab (avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Lasers Imaging 2005; 36: 331–335.
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK et alMARINA study group. Ranibizumab for neovascular age-related macular degeneartion. N Engl J Med 2006; 355: 1419–1431.
Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS et alANCHOR Study group. Ranibizumab versus vertoporfin for neovascular age-related macular degeneration. N Engl J Med 2006; 355: 1432–1444.
Lalwani GA, Rosenfeld PJ, Fung AE, Dubovy SR, Michels S, Feuer W et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol 2009; 148: 43–58.
Barron H. MedWatch Genentech. ımportant drug warning [letter]. US Food and Drug Administration. Available at: http://www.fda.gov/medwatch/SAFETY/2005/Avastin_dearhcp.pdf.
Lee K, Yang H, Lim H, Lew HM . A prospective study of blood pressure and intraocular pressure changes in hypertensive and nonhypertensive patients after intravitreal bevacizumab injection. Retina 2009; 29: 1409–1417.
Kernt M, Neubauer AS, Kampik A . Intravitreal bevacizumab (Avastin) treatment is safe in terms of intraocular and blood pressure. Acta Ophthalmol Scand 2007; 85: 119–120.
Ziemssen F, Zhu Q, Peters S, Grisanti S, El Wardani M, Szurman P et al. Intensified monitoring of circadian blood pressure and heart rate before and after intravitreous injection of bevacizumab: preliminary findings of a pilot study. Int Ophthalmol 2009; 29: 213–224.
Risimic D, Milenkovic S, Nikolic D, Simeunovic D, Jaksic V, Stojkovic M et al. Influence of intravitreal injection of bevacizumab on systemic blood pressure changes in patients with exudative form of age-related macular degeneration. Hellenic J Cardiol 2013; 54: 435–440.
Wu L, Martinez-Castellanos MA, Quiroz-Mercado H, Arevalo JF, Berrocal MH et alPan American Collaborative Retina Group (PACORES). Twelve-month safety of intravitreal injections of bevacizumab (Avastin): results of Pan-American Collaborative Retina Study Group (PACORES). Graefes Arch Clin Exp Ophthalmol 2008; 246: 81–87.
Pande A, Lombardo J, Spangenthal E, Javle M . Hypertension secondary to anti-angiogenic therapy: experience with bevacizumab. Anticancer Res 2007; 27 (5B): 3465–3470.
Zeb A, Ali SR, Rohra DK . Mechanism underlying hypertension and proteinuria caused by bevacizumab. J Coll Physicians Surg Pak 2007; 17: 448–449.
Dincer M, Altundag K . Angiotensin-converting enzyme inhibitors for bevacizumab-induced hypertension. Ann Pharmacother 2006; 40: 2278–2279.
Kamba T, McDonald DM . Mechanisms of adverse effects of anti-VEGF therapy for cancer. Br J Cancer 2007; 96: 1788–1795.
Staessen JA, Thijs L, Fagard R, O'Brien ET, Clement D, de Leeuw PW et al. Predicting cardiovascular risk using conventional vs ambulatory blood pressure in older patients with systolic hypertension. systolic hypertension in Europe trial ınvestigators. JAMA 1999; 282: 539–546.
O'Brien E, Sheridan J, O'Malley K . Dippers and nondippers. Lancet 1988; 2: 397.
Shimada K, Kawamoto A, Matsubayashi K, Nishinaga M, Kimura S, Ozawa T . Diurnal blood pressure variations and silent cerebrovascular damage in elderlypatients with hypertension. J Hypertens 1992; 10: 875–878.
Pickering TG . The clinical significance of diurnal blood pressure variation; dippers and nondippers. Circulation 1990; 81: 700–702.
Verdecchia P, Porcellati C, Schillaci G, Borgioni C, Ciucci A, Battistelli M et al. Ambulatory blood pressure: an independent predictor of prognosis in essential hypertension. Hypertension 1994; 24: 793–801.
Mansoor GA . Sleep actigraphy in hypertensive patients with the 'non-dipper' blood pressure profile. J Hum Hypertens 2002; 16: 237–242.
Pickering TG . Ambulatory blood pressure monitoring in clinical practice. Clin Cardiol 1991; 14: 557–562.
Ventola CL . Off-label drug information: regulation, distribution, evaluation, and related controversies. P T 2009; 34: 428–440.
US Food and Drug Administration. 'Off-label' and investigational use of marketed drugs, biologics, and medical devices. Information sheets. Available at: http://www.fda.gov/oc/ohrt/irbs/offlabel.html.
Mancia G, Fagard R, Narkiewicz K, Redon J, Redon J, Zanchetti A et al2013 ESH/ESC practice guidelines for the management of arterial hypertension. Blood Press 2014; 23: 3–16.
Michels S, Rosenfeld PJ, Puliafito CA, Marcus EN, Venkatraman AS . Systemic bevacizumab (avastin) therapy for neovascular age-related macular degeneration twelve-week results of an uncontrolled open-label clinical study. Ophthalmology 2005; 112 (6): 1035–1047.
Rich RM, Rosenfeld PJ, Puliafito CA, Dubovy SR, Davis JL, Flynn HW Jr et al. Short-trem safety and efficacy of intravitreal bevacizumab (avastin) for neovascular age related macular degeneration. Retina 2006; 26 (5): 495–511.
Reimann M, Folprecht G, Haase R, Trautmann K, Ehninger G, Reichmann H et al. Anti-vascular endothelial growth factor therapy impairs endothelial function of retinal microcirculation in colon cancer patients – an observational study. Exp Transl Stroke Med 2013; 5: 7.
Grothey A, Sugrue MM, Purdie DM, Dong W, Sargent D, Hedrick E et al. Bevacizumab beyond first progression is associated with prolonged overall survival in metastatic colorectal cancer: results from a large observational cohort study (BRiTE). J Clin Oncol 2008; 26: 5326–5334.
Rasier R, Artunay O, Yuzbasioglu E, Sengul A, Bahcecioglu H . The effect of intravitreal bevacizumab (avastin) administration on systemic hypertension. Eye 2009; 23: 1714–1718.
Vaklavas C, Lenihan D, Kurzrock R, Tsimberidou AM . Anti-vascular endothelial growth factor therapies and cardiovascular toxicity: what are the important clinical markers to target? Oncologist 2010; 15: 130–141.
Yang JC, Haworth L, Sherry RM, Hwu P, Schwartzentruber DJ, Topalian SL et al. A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med 2003; 349: 427–434.
Palatini P . Masked hypertension: how can the condition be detected? Blood Press Monit 2004; 9: 297–299.
Felmeden DC, Spencer CG, Belgore FM, Blann AD, Beevers DG, Lip GY . Endothelial damage and angiogenesis in hypertensive patients: relationship to cardiovascular risk factors and risk factor management. Am J Hypertens 2003; 16: 11–20.
Sane DC, Anton L, Brosnihan KB . Angiogenic growth factors and hypertension. Angiogenesis 2004; 7: 193–201.
Mourad JJ, des Guetz G, Debbabi H, Levy BI . Blood pressure rise following angiogenesis inhibition by bevacizumab. a crucial role for microcirculation. Ann Oncol 2008; 19: 927–934.
Steeghs N, Gelderblom H, Roodt JO, Christensen O, Rajagopalan P, Hovens M et al. Hypertension and rarefaction during treatment with telatinib, a small molecule angiogenesis inhibitor. Clin Cancer Res 2008; 14: 3470–3476.
Yang R, Thomas GR, Bunting S, Ko A, Ferrara N, Keyt B et al. Effects of vascular endothelial growth factor on hemodynamics and cardiac performance. J Cardiovasc Pharmacol 1996; 27 (6): 838–844.
Yang R, Bunting S, Ko A, Keyt BA, Modi NB, Zioncheck TF et al. Substantially attenuated hemodynamic responses to Escherichia coli-derived vascular endothelial growth factor given by intravenous infusion compared with bolus injection. J Pharmacol Exp Ther 1998; 284: 103–110.
Matsuyama K, Ogata N, Matsuoka M, Wada M, Takahashi K, Nishimura T et al. Plasma levels of vascular endothelial growth factor and pigment epithelium-derived factor before and after intravitreal injection of bevacizumab. Br J Ophthalmol 2010; 94: 1215–1218.
Bakri SJ, Melissa R, Pulido JS, Singh RJ . Pharmacokinetics of intravitreal bevacizumab (avastin). Ophthalmology 2007; 114: 855–859.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Sengul, A., Rasier, R., Ciftci, C. et al. Short-term effects of intravitreal ranibizumab and bevacizumab administration on 24-h ambulatory blood pressure monitoring recordings in normotensive patients with age-related macular degeneration. Eye 31, 677–683 (2017). https://doi.org/10.1038/eye.2016.305
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.305
This article is cited by
-
Emerging therapeutic strategies for unmet need in neovascular age-related macular degeneration
Journal of Translational Medicine (2023)
-
The ideal intravitreal injection setting: office, ambulatory surgery room or operating theatre? A narrative review and international survey
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Intravitreal anti‑VEGF agents and cardiovascular risk: comment
Internal and Emergency Medicine (2021)
-
Ocular microcirculation changes, measured with laser speckle flowgraphy and optical coherence tomography angiography, in branch retinal vein occlusion with macular edema treated by ranibizumab
International Ophthalmology (2021)
-
Immediate changes in blood pressure during intravitreal anti-VEGF agents' applications in exudative age-related macular degeneration patients
International Ophthalmology (2020)