Abstract
Purpose
To quantitatively determine the size and contractility of the superior oblique (SO) muscle in primary SO overaction (PSOOA).
Patients and methods
A prospective, observational study was conducted on 12 patients with PSOOA, and 10 healthy, orthotropic subjects. Sets of contiguous, 2 mm slice thickness, quasi-coronal magnetic resonance imaging were obtained during different gazes, giving pixel resolution of 0.391 mm. Cross-sectional areas of the SO muscles were determined in primary position, supraduction, and infraduction to evaluate size and contractility. The cross-sectional areas of SO muscle were compared with those of controls in the primary position to detect hypertrophy or atrophy and changes in contractility could be detected during the vertical gaze. All statistical calculations were performed using PROC MIXED (SAS 9.4).
Results
There was no difference between the ipsilesional (affected eye), contralesional (unaffected eye), and normal SO muscle cross-sections: 0.176±0.018 cm2, 0.175±0.005 cm2, and 0.173±0.015 cm2, respectively (P=0.82). The maximum contractility of SO muscle on the ipsilesional (affected) side was 0.097±0.024 cm2, and was different than on the contralesional (unaffected) side: 0.067±0.015 cm2 and in control subjects: 0.063±0.018 cm2 (P=0.0002).
Conclusions
In PSOOA, the ipsilesional SO is more contractile than the contralesional SO muscle and different than in controls, with no difference in SO muscle size in primary position, which suggests that excessive innervation rather than muscle hypertrophy underlies PSOOA.
Similar content being viewed by others
Introduction
Superior oblique (SO) overaction is typically diagnosed based on physical examination, which includes an excessive amount of rotation of the eye in infraducted adduction (inward and down gaze), as well as measurements of binocular misalignment. However, the clinical examination poorly distinguishes SO overaction from other scenarios, such as heterotopic rectus extraocular muscles (EOM) pulleys, pulley instability, or other orbital or structural EOM abnormalities.1 SO overaction can be divided into primary SO overaction (PSOOA) and secondary ones. Most patients suffer from PSOOA, commonly associated with an ‘A’ pattern with unclear etiology, but rarely the SO overaction is secondary to inferior oblique palsy. SO overaction interferes with binocular vision and quality of life. For those with a noticeable strabismus, they may feel embarrassed to communicate with others.2 In addition, people with SO overaction often look down for a lengthy time when studying, working, or playing games. The overaction of SO muscles would then continuously induce abduction, leading to instability of orthotropia and difficulty in the development or maintenance of binocular function. The surgical treatment consists of SO tenectomy, tenotomy, horizontal rectus transposition, and various other kinds, with inconsistent postoperative outcomes, including secondary inferior oblique overaction, residual SO overaction, secondary SO palsy and so on. In addition, there is no agreement about the pathophysiology underlying SO overaction.3, 4 The course of disease is generally benign, which precludes invasive diagnostic procedures, and the inaccessibility to direct study makes the understanding of mechanical state of the oblique EOM’s rather complex.5, 6 The current progress in non-invasive imaging methods, such as magnetic resonance imaging (MRI) permits addressing the functional anatomy of the eye, which was exploited in the studies of SO palsy.7, 8, 9 The aim of this study was to quantitatively determine the morphology and contractility of the SO muscle in PSOOA, which could be used to facilitate the pathogenic diagnosis.
Materials and methods
Subjects
This prospective observational study was conducted at West China Hospital, according to a protocol approved by the ethics committee of West China Medical School, Sichuan University (Chengdu, China), conforming to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all study participants. The study consisted of 12 patients with a clinical diagnosis of PSOOA and 10 healthy, orthotropic, and paid volunteers recruited by advertisement. All subjects with PSOOA underwent comprehensive ophthalmologic examinations by an experienced pediatric ophthalmologist, including binocular misalignment measurement by prism and cover testing, as well as Hess screen test. Normal volunteers also underwent complete eye examinations to verify normal corrected vision, ocular versions, orthotropia in all gaze positions, stereoacuity, and no one had undergone any prior ocular surgery.
PSOOA was diagnosed when the following clinical findings were present: an overdepression of the ipsilateral (affected) eye in adduction and was always associated with an ‘A’ pattern; ipsilateral hypotropia increasing in infra-adduction and the difference in the vertical deviation with head tilting was minimal. Generally, if SO overaction is bilateral and symmetric, there will be no hypertropia in the primary position, but an ‘A’ pattern is typically present. If the SO overaction is unilateral, there may be a degree of hypertropia in the primary position.10 Subjects were excluded if they could not cooperate for MRI exam, or if they had a history of prior strabismus surgery.
A total of 20 orbits were imaged in 10 normal subjects of mean (±SD) age 18±4 years old (range, 12–25 years). Both orbits in three subjects with unilateral PSOOA and nine with bilateral PSOOA, with a mean age of 21±11 (range, 10–43) years were imaged.
MRI
A 3.0 T (SIEMENS TRIO) scanner was used for imaging. T1-weighted, orbital MRI was performed with a 256 × 256 matrix over an 8- or 10-cm field of view, giving pixel resolution of 0.391 mm. Sets of 18 contiguous 2-mm-thick images in the quasi-coronal planes were obtained perpendicular to the long axis of the orbit to image the SO and other EOMs (Figure 1). During imaging, subjects’ heads were oriented in the scanner such that the axis of the scanned orbit was vertical. Subjects fixated on custom-made, small, brightly colored crosses, affixed to the inside of the scanner magnet with a width of 1.5 cm diameter.7 The primary position was first performed quasi-coronally, after that, scans were repeated in supraduction and infraduction.
Image processing
MRI image planes were transferred to the WorkStation (syngoMMWP VE40A). From each slice, a cross-sectional area of the SO was outlined manually three times using the ‘freehand range of interest’ function of the workstation tools to compute a mean value. The globe-optic nerve junction was localized as plane zero (Figure 1). For SO contractility, we analyzed only orbits for which there were complete image sets in upward and downward gaze positions. Contractile change was taken to be the cross-section in infraduction minus that in supraduction for each image plane.8 As quasi-coronal image planes are perpendicular to the orbit, but not to the SO muscle, cross-sectional area and contractility were trigonometrically corrected to obtain a true cross-section perpendicular to the long axis of the SO.
Statistical analysis
All statistical calculations were performed using PROC MIXED (SAS 9.4, Cary, NC, USA). The type III test of fixed effects has been used to determine statistical significance, and the least mean square difference test was employed for comparison between means. The level of statistical significance has been set at P<0.05. Due to the exploratory character of the study, it was not possible to perform power analysis a priori. However, we have performed a posteriori evaluation, which has shown that at least 12 eyes per group are sufficient to detect the statistically significant change if it exists. As the study did not have the therapeutic arm, the pre-specification of effect size was not applicable.
Results
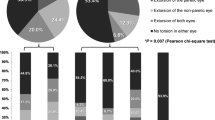
Four patients had bilateral and symmetric overaction, accompanied by an ‘A’ pattern. Five patients had a bilateral SO overaction and asymmetry, with a mean of 7Δ hypotropia in the primary position. In three patients, the SO overaction was unilateral, with a mean of 13Δ hypotropia in the primary position. Clinical characteristics of the subjects with PSOOA are summarized in Table 1.
In the primary position, the greatest SO cross-sections occurred about midorbit, 6 mm posterior to the globe-optic nerve junction. In down gaze, the SO cross-sectional area increased, and the plane in which the maximum cross-sectional area observed was more posterior. In up gaze, the SO cross-sectional area decreased, and the plane in which the maximum cross-sectional area observed was more anterior (Figure 2).
SO muscle size
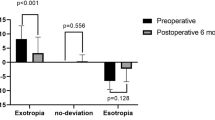
The maximum cross-sectional area of SO muscle on the ipsilesional side was 0.176±0.018 cm2, and was not different than on the contralesional side in patients: 0.175±0.005 cm2 and in control subjects: 0.173±0.015 cm2 (P=0.82, Figure 3).
SO muscle contractility
The maximum contractility of SO muscle in the ipsilesional side was 0.097±0.024 cm2, which was different than on the contralesional side in patients: 0.067±0.015 cm2 and in control subjects: 0.063±0.018 cm2 (P=0.0002, Figure 4).
Discussion
Demer and Miller reported that apparent EOM overaction could be caused by many different factors, including an increase in contractile force of EOM, which is supposed to be responsible for many pathological conditions.7 Also, the cause of EOM overaction includes excessive innervation, an increase in muscle’s cross-sectional area (hypertrophy), and changes in muscle fiber types within the muscle.1, 11 We did not observe differences in the muscle cross-section area, which indicates that muscle hypertrophy is not the likely reason for PSOOA. On the contrary, we found a difference in contractility between eyes with SO overaction and control eyes. The finding that the SO in particular was not hypertrophic in primary position but had significantly more contractile change is similar to the results of an early MRI study of the contralesional inferior rectus muscle in SO palsy, which also found increased contractility but not the change of cross-sectional area.1 This may indicate abnormal innervation resulting in increased muscle stimulation or changes in muscle fiber composition. The abnormal innervation might indeed provide a potential explanation. As the anterior half of the reflected SO tendon and belly near the equator of the globe has the greatest intorsion function, whereas the posterior half primarily has a depression function,10 the excess innervation may primarily act on the posterior half of SO, where the contractile changes mainly occurred, which is in accordance with the anatomy of SO. However, the potential neurological and/or sensory mechanisms that might be responsible for the abnormal innervation are unknown. Alternatively, it could be attributed to the results of pathology of vergence and gaze commands, like the hypothesis of EOM study by Schoeff.12 The neural commands in humans might have a role in causing larger-than-normal changes with eye position, with the normal EOMs. In addition, animal models have indicated that abnormal visual experience in infancy can induce abnormal cross-axis eye movements, and A- or V- pattern in the absence of gross structural abnormalities of EOMs.13 For the change of muscle fiber composition, it is difficult to identify because of a lack of a practical way to obtain tissue samples of the entire muscle in humans with strabismus.
Other theories about oblique muscle dysfunction include rectus pulley heterotopy,4 and pulley instability and ocular torsion.14 A previous study indicated that four subjects with ‘A’ pattern strabismus with marked SO overation was actually due to heterotopic pulleys’ function.4 But, it has also been argued that pulley heterotopia only accounts for some patients who show overdepression in adduction. Like the research into SO palsy, the studies indicated that the expected atrophy or impaired contractility of the SO muscle belly is not present in one third to one half of presumed SO palsies.4 However, it was also demonstrated that SO atrophy, complete absence and segmental posterior atrophy is involved in patients with SO palsy, showing a heterogenity of changes which occur but provide the same muscle phenotype response, meaning there are likely to be multiple mechanisms involved.7 In the current study, the MRI indicated that the contractility of the SO is changed. This study is a preliminary study, with relatively few subjects. Later studies would be recommended to further illustrate SO and other EOMs cross-section, contractility, and pulley locations to get a better understanding of PSOOA. This could then open the way to more targeted treatment.
In Conclusion, the lack of changes in the SO muscle cross-sectional area and the significant difference in contractile function suggest that an innervation abnormality rather than muscle hypertrophy is responsible for PSOOA.

References
Clark RA, Demer JL . Enhanced vertical rectus contractility by magnetic resonance imaging in superior oblique palsy. Arch Ophthalmol 2011; 129: 904–908.
Xu J, Yu X, Huang Y, Chen J, Yu H, Wang Y et al. The psychosocial effects of strabismus before and after surgical correction in Chinese adolescents and adults. J Pediatr Ophthalmol Strabismus 2012; 49: 170–175.
Demer JL . Clarity of words and thoughts about strabismus. Am J Ophthalmol 2001; 132: 757–759.
Clark RA, Miller JM, Rosenbaum AL, Demer JL . Heterotopic muscle pulleys or oblique muscle dysfunction? J AAPOS 1998; 2: 17–25.
Miller JM, Robinson DA . A model of the mechanics of binocular alignment. Comput Biomed Res 1984; 17: 436–470.
Neetens A, Janssens M . The superior oblique: a challenging extraocular muscle. Doc Ophthalmol 1979; 46: 295–303.
Demer JL, Miller JM . Magnetic resonance imaging of the functional anatomy of the superior oblique muscle. Invest Ophthalmol Vis Sci 1995; 36: 906–913.
Jiang L, Demer JL . Magnetic resonance imaging of the functional anatomy of the inferior rectus muscle in superior oblique muscle palsy. Ophthalmology 2008; 115: 2079–2086.
Kono R, Demer JL . Magnetic resonance imaging of the functional anatomy of the inferior oblique muscle in superior oblique palsy. Ophthalmology 2003; 110: 1219–1229.
Kushner BJ . Vertical Strabismus. In: Hoyt GS, Taylor D (eds). Pediatric Ophthalmology and Strabismus, 4th edn. Elsevier: China, 2013, p 804.
Kushner BJ . Multiple mechanisms of extraocular muscle ‘overaction’. Arch Ophthalmol 2006; 124: 680–688.
Schoeff K, Chaudhuri Z, Demer JL . Functional magnetic resonance imaging of horizontal rectus muscles in esotropia. J AAPOS 2013; 17: 16–21.
Narasimhan A, Tychsen L, Poukens V, Demer JL . Horizontal rectus muscle anatomy in naturally and artificially strabismic monkeys. Invest Ophthalmol Vis Sci 2007; 48: 2576–2588.
Oh SY, Clark RA, Velez F, Rosenbaum AL, Demer JL . Incomitant strabismus associated with instability of rectus pulleys. Invest Ophthalmol Vis Sci 2002; 43: 2169–2178.
Acknowledgements
The study was supported by Department of Science and Technology of Sichuan Province, grant number 2012SZ0138.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Gong, Q., Janowski, M., Tang, H. et al. Magnetic resonance imaging of the functional anatomy of the superior oblique muscle in patients with primary superior oblique overaction. Eye 31, 588–592 (2017). https://doi.org/10.1038/eye.2016.274
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.274
This article is cited by
-
MRI evidence of extraocular muscle atrophy and fatty replacement in myasthenia gravis
Neuroradiology (2021)