Abstract
Purpose
To compare focometer and autorefractor in the measurement of refractive errors among students in an underserved community of sub-Saharan Africa.
Methods
The study was a descriptive comparative cross-sectional study conducted in October/November 2014 among secondary school students of Ijaiye-Orile, Oyo State, Nigeria. Students were selected using systematic random sampling method. Ocular examination and measurement of refractive error was carried out on each student using a focometer and an autorefractor.
Results
A total of 230 students were studied. Mean age of the students was 15.1±1.9 years with a range of 13–21 years. Refractive error was detected in 95 (41.3%) of the students using autorefractor and in 81 (35.2%) with focometer. Among those found to have refractive error using autorefractor, 75 (78.9%) students had a difference of ≤±0.75 DS between the autorefractor and focometer readings. The sensitivity and specificity of the focometer relative to the autorefractor was 73.7% and 91.9%, respectively.
Conclusion
The focometer is comparable to the autorefractor in the measurement of refractive error because of its high sensitivity and specificity. The high positive and negative predictive values makes the focometer an effective tool for both screening and diagnosis of refractive error in rural areas among secondary schools students. Its use would make refractive service available and affordable to individuals living in the resource poor rural communities thereby reducing the burden of refractive error in such areas. The focometer should also be a useful tool in school eye health programs.
Similar content being viewed by others
Introduction
The World Health Organization (WHO) in year 20101 estimated the number of people with visual impairment to be about 285 million; made up of 39 million blind individuals and 246 million people with moderate and severe visual impairment.1 Out of the 246 million individuals with low vision, uncorrected refractive errors (URE) accounted for 153 million.2 URE is also the second leading cause of blindness occurring in 8 million individuals.2
Since refractive error manifests at a young age, the number of associated blind-person-years from URE was double the estimate for individuals blind from cataract.3 URE is the single largest contributor to the global burden of eye diseases4 and among children it is the leading and most easily remedied cause of poor vision.5 The prevalence of refractive error among school students in Nigeria varies between 1.97% and 5.8%.6, 7, 8
School children are an important large target group for detection of eye diseases9 and this early detection provides the best opportunity for effective treatment thereby preventing blindness. However, there are various factors responsible for uncorrection of refractive errors, these include lack of awareness and recognition of the problem at personal, family, community and public health level. Other factors responsible include non-availability or inability to afford refractive services, insufficient provision of affordable corrective lenses and cultural disincentives to compliance.10
About 90% of the burden of eye disease occurs in low- and middle-income countries4 where access to refraction services and the availability of spectacles are generally poor.11 One approach to make refractive services readily available and affordable is the introduction of a simple device called a ‘focometer’.12, 13, 14 This is a self-adjustable telescopic refractive device used to subjectively determine the value of an individual’s refractive error. It is portable, lightweight, compact and fairly quick to use. The focometer is less expensive compared with an autorefractor and does not require electricity nor prolonged and intensive training for its use.14
However, there are few published data about the reliability of focometer measurements.15 A study about its validity conducted by the manufacturer reported that focometer measurements are within 0.50 DS of an autorefractor measurement and 0.10 DS of a subjective refraction.13 So, as recommended by WHO, the focometer measurements have offered sufficient visual outcomes that can make it to be considered for use in public health programs. It has been suggested that there is a need to carry out a field testing in a developing country setting to determine whether the focometer has application as a public health tool in such locality.15 However, to the best of the author’s knowledge there has not been any study conducted to fill this gap in knowledge in Nigeria.
The aim of this study was to compare the measurement of refractive error using a focometer and an autorefractor in a rural community where electricity is erratic, coupled with lack of adequate human and infrastructural resources. An autorefractor was used for this comparison because the validity and reliability of various autorefractors have been established in various studies.16, 17, 18
Materials and methods
The study was a descriptive comparative cross-sectional study conducted between October and November 2014.
The study was carried out at Ijaiye High School, Ijaiye-Orile, Akinyele Local Government Area of Oyo state. This is entirely a rural community which lacks basic amenities such as portable water and stable electricity. The major inhabitants are the Yoruba ethnic group.19 The population of the local government based on estimates from the Nigerian 2006 population census using 2.88% growth rate was 270 235 in the year 2013.
Participants were students of Ijaiye High School, Ijaiye-Orile, aged 13 years and above. Students with ocular co-morbidity causing poor vision such as cornea scar, cataract, retinal detachment, macular scar, and so on were excluded from the study.
Sampling technique
Systematic random sampling method with a sampling fraction of 2(two) was used to select the students using the school register. The total number of students in the school was 551. If a selected student in a class was not eligible then the next student on the register was selected and the sampling procedure (every other student) was continued till the calculated sample size of 230 was obtained. The sample size was computed using the comparative formula for paired data. Power was set at 80%, significance level of 0.05 was chosen and an estimated prevalence of 84% was the proportion of students with focometer reading (spherical equivalent) within 0.75 DS of that of the autorefractor.15
Data collection
Interviewer administered semi-structured questionnaires were used to obtain information on the bio-data of the students and their ocular history. Measurement of refractive error with autorefractor and focometer was done respectively by separate examiners. Using the findings of the autorefractor, subjective refraction was then carried out.
Ethical approval
Approval for the conduct of this study was obtained from the Ministry of Education, Oyo state secretariat Ibadan and ethical approval obtained from the Ethical Committee of University of Ibadan/University College Hospital Ibadan. The study was carried out in line with the principles and tenets of the declaration of Helsinki for studies on human subjects. Also, study permission was obtained from the Principal of the school. Signed informed consent forms were obtained from the parent/guardian of selected students and assent of the selected students was obtained individually.
Data analysis
The collected data were entered into a database and was analyzed using Statistical Package for Social Sciences (SPSS) version 21(IBM Corp., NY, USA). The test of analysis between qualitative variables was done using chi-square test and level of statistical significance set at P-value <0.05.
The focometer was assessed for specificity and sensitivity for measuring refractive error with reference to autorefraction.
Paired t-test was done to test for association between quantitative variables. Repeatability was determined by the calculation of the coefficient of repeatability (COR). The COR is 1.96 times the SD of paired differences.20
Definition of terms for the study
-
Refractive error includes myopia, hypermetropia and astigmatism.
-
Myopia was defined as spherical error of higher than −0.5 D (ie, >−0.5 D).2, 21
-
Hypermetropia was defined as spherical error greater than +0.5 D (ie, > +0.5 D).2, 21
-
Astigmatism (minus cylinder format) was defined as a cylindrical error greater than 0.5 D.21
-
True Positives are the number of students that had refractive error using autorefractor and were confirmed by the focometer.
-
False Positives are the number of students that did not have refractive error using the autorefractor but were found to have refractive error using focometer.
-
True Negatives are the number of students that did not have refractive error using autorefractor and were found to be negative by the focometer.
-
False Negatives are the number of students that had refractive error using autorefractor but were found to be negative by the focometer.
Results
Two hundred and thirty secondary school students had refraction done with both autorefractor and focometer. The mean age of the students studied was 15.1±1.9 years. The range was 13–21 years. They comprised of 123 (53.4%) males and 107 (46.6%) females.
Autorefractor revealed that 95 (41.3%) students had refractive error. Forty nine (39.8%) males had refractive error compared with 46 (43%) females. The difference between the genders was not statistically significant (P-value 0.628).
Comparing refractive status between autorefraction and focometer
About three quarters of students with refractive error using autorefractor were also detected to have refractive error using focometer. Focometer was observed to have a high sensitivity (73.7%) for diagnosing refractive errors in comparison with autorefraction, a high specificity (91.9%) in comparison to autorefraction as well as a nine fold chance of accurately diagnosing refractive error with a possibility of 29% margin of error. Similarly, focometer has high positive and negative predictive values for refractive errors when compared to autorefraction (86.4% and 83.2%, respectively) as shown in Table 1.
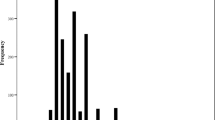
Distribution of different types of refractive error in study subjects
The distribution of the types of refractive errors among the study subjects is shown in Figure 1. Most of the patients with refractive error had myopia with either of the test instruments (autorefractor; 48.5%, focometer; 76.5%). There was no statistically significant difference between the proportion of myopia and hypermetropia using the test instruments (P-value >0.05). However, the proportion of students noted to have astigmatism with autorefraction was significantly higher than those diagnosed with focometer (P-value=0.005).
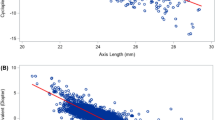
Comparison of the degrees of refractive error between the two test instruments
The mean of the spherical errors was −0.37±1.42 DS, mean of Cylindrical errors was −0.62±0.75 Dcyl, and mean of Spherical equivalents was −0.58±1.34 DS with the autorefractor while the mean spherical error, Cylindrical error and Spherical equivalents using the focometer were −0.31±1.04 DS, −0.09±0.35 Dcyl and −0.34±0.98 DS respectively. There was no significant difference in the degree of spherical errors detected by the two tests instruments (P-value >0.05). However, focometer was observed to be less effective in detecting cylindrical errors with a statistically significant mean difference when compared with autorefractor (P-value 0.001).
There was also a statistically significant difference between the spherical equivalents obtained between autorefractor and focometer (P-value 0.006).
Difference in the value of refractive error using the test instruments
The mean difference in the value of spherical equivalents of the refractive error measurements in each student using autorefractor and focometer was −0.25±0.86 DS. Further analysis indicated that 75 students (78.9%) had a difference of ≤±0.75 DS and 20 students (21.1%) had a difference > ±0.75 DS between the two test instruments, whereas 80 students (84.2%) were within 0.75 DS difference and 15 (14.8%) had >0.75 DS difference between subjective refraction and focometer, as shown in Table 2.
Repeatability of study instruments
The repeatability of the study instruments was determined to evaluate level of agreement between focometer and autorefractor. The COR between the focometer and the autorefractor measurement of refractive error was found to be close to each other indicating a high level of agreement between the two test instruments (Table 3).
Level of agreement between the two test instruments
The level of agreement between the test instruments was further corroborated as shown in Figure 2. The difference in the spherical equivalent of autorefractor and focometer shows a 95% limit between −4.00 DS to +2.00 DS. Majority of the measurements were interspersed within the 95% limits of agreement with a few outliers.
Discussion
A cost effective means of making refractive services available and affordable to individuals in the rural areas of low income countries is paramount in reducing the huge burden of URE in such regions. The focometer is designed to overcome majority of the obstacles to refractive services in a rural setting. So this study was designed to compare focometer with autorefractor with the intention of making recommendations for an efficient refractive error test instrument which may be adopted as a screening tool in a resource poor rural community.
The proportion of students with refractive error in the study population using the study definition as determined by using the autorefractor was 41.3% while with the focometer it was 35.2%. This was low compared to the findings by Du Toit et al15 where 99% of the population studied had refractive error using the autorefractor. This may be due to the differences in definitions of the refractive errors used in their study compared with this study. In addition most studies,2, 11 on refractive error usually document subjectively refined refraction of retinoscopy rather than the objective autorefraction, hence there are limited studies to compare the findings of this study with.
The distribution of the types of refractive error with autorefractor was 46 (48.5%), 11 (11.5%), and 38 (40%) for myopia, hypermetropia and astigmatism respectively while focometer readings showed 62 (76.5%), 11 (13.5%), and 8 (10%) for myopia, hypermetropia and astigmatism, respectively. These findings are different from the findings of Du Toit et al15 in Australia where autorefractor showed that 63% of the study population were myopic, 36% were hypermetropic and 91% had astigmatism while only 32% had astigmatism with the focometer. This variation may be related to differences in the definitions of refractive error used, differences in age group and ethnicity of the study population. All these factors have been shown to affect the prevalence and pattern of refractive error globally.
Comparing the two test instruments; the sensitivity and specificity of the focometer are good; 73.6% and 91.9%, respectively. These indicate that the focometer has the capacity to identify refractive error easily when present in an individual and can also identify an individual without refractive error quite accurately. Likewise, the high positive and negative predictive values for refractive error measurement of the focometer compared with an autorefractor indicate that it can be used effectively as both diagnosing and screening test tool for refractive error in a student population.
The COR indicates that the measurements of refractive error with the two test instruments are reliable and similar to each other. This is also similar to the findings of Du Toit et al15 in which the difference of COR between the focometer and autorefractor was 0.05 for one of the groups.
The mean difference of the spherical and cylindrical errors obtained between the autorefractor and focometer were −0.05 DS±0.89 (P=0.582) and −0.52DC ±0.65 (P=0.001) respectively demonstrating that the cylindrical error mean difference was statistically significant. This is similar to the findings of Du Toit et al15 indicating that the focometer is not very accurate in the determination of cylinder power and axis in astigmatic prescriptions. This may be because the clock target (recommended by the manufacturer) has radials at 30° intervals and the cylinder axis determination with the focometer can only be measured to the nearest 15° resulting in approximation of the cylindrical axis degree. Another reason may be because some participants unintentionally tend to prefer the spherical equivalent of the refractive error they have rather than going through the procedure of identifying the cylindrical power and axis of their error.
The spherical equivalent measurements of refractive error between the two test instruments showed that 56.8% of the participants with refractive error had a difference of ≤±0.50 DS and 78.9% had a difference of ≤±0.75 DS. This difference in refractive error measurements is comparable to the findings of Du Toit et al15 where 62% of the focometer spherical equivalent measurements were within 0.50 DS of the autorefractor, and 84% were within 0.75 DS. However, the slightly lower values in this study might be because the study population used by Du Toit et al15 were students of optometry who were older and better informed about the test instruments and were likely to follow instructions better than secondary students. This agreement rate was higher when comparing the focometer with subjective refraction in which the focometer readings of 84.2% participants with refractive error fell within 0.75 difference of an autorefractor. This indicates that there is better agreement between the focometer and the subjective than the autorefractor probably because focometer is also a subjective method of measuring refractive error.
The focometer was able to improve the vision of those (12.6%) with visual acuity worse than 6/6 to 6/6 or better. According to WHO,15 the goal of a public health program is to offer the greatest number of people the best possible visual acuity through refractive error correction which should be at least 6/18, beyond which there is visual impairment. In this study, 100% of the participants achieved at least 6/6 with their focometer prescription. This suggests that the focometer measurements offered sufficient visual outcomes to consider its use in public health programs especially in a resource poor rural community and hence can be useful in a school eye health program.
This study has some limitations. First, the calibration (1D apart) of the focometer and the clock target radials at 30° intervals both might have lead to the approximations of spherical and cylindrical corrections respectively hence affecting the accuracy of the focometer astigmatic correction. Second, accuracy of the result obtained from the focometer is largely dependent on the patient’s input. Third, the unavailability of cycloplegic refraction as the gold standard for comparison with the focometer is also a limitation.
In conclusion, this study showed that the result of measuring refractive error with focometer is comparable to the results from an autorefractor especially for spherical corrections. However, it is less accurate for cylindrical corrections. The high sensitivity and specificity of a focometer relative to an autorefractor and the high positive and negative predictive values indicate that it is an effective tool for both screening and diagnosing refractive error in rural areas among secondary schools students. Hence the focometer is a cheaper alternative to autorefractor in a resource poor rural community.
We recommend that the focometer should be made available in the primary eye care centers so that basic screening for refractive errors can be done at this level of eye care with prompt referral of appropriate cases when indicated. In addition, school eye health programs may make use of the focometer for screening purposes to detect refractive errors among students.
Similar studies comparing focometer and autorefractor in the adult population of the community should also be conducted with respect to near vision and reading.

References
Pascolini D, Mariotti SP . Global estimates of visual impairment: 2010. Br J Ophthalmol 2012; 96 (5): 614–618.
Ezelum C, Razavi H, Sivasubramaniam S, Gilbert CE, Murthy GV, Entekume G et al. Refractive error in Nigerian adults: prevalence, type, and spectacle coverage. Invest Ophthalmol Vis Sci 2011; 52 (8): 5449–5456.
Dandona L, Dandona R, Srinivas M, Giridhar P, Vilas K, Prasad MN et al. Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci 2001; 42 (5): 908–916.
Ono K, Hiratsuka Y, Murakami A . Global inequality in eye health: Country-level analysis from the Global Burden of Disease Study. Am J Public Health 2010; 100 (9): 1784–1788.
Zhang M, Zhang R, He M, Liang W, Li X, She L et al. Self correction of refractive error among young people in rural China: results of cross sectional investigation. Br Med J (Clinical research ed) 2011; 343: d4767.
Chuka-Okosa CM . Refractive errors among students of a postprimary institution in a rural community in south-eastern Nigeria. West Afr J Med 2005; 24: 62–65.
Opubiri I, Pedro-Egbe C . Screening for refractive error among primary school children in Bayelsa State, Nigeria. Pan Afr Med J 2013; 14: 74.
Ajaiyeoba AI, Isawumi MA, Adeoye AO, Oluleye TS . Pattern of eye diseases and visual impairment among students in southwestern Nigeria. Int Ophthalmol 2007; 27 (5): 287–292.
Desai S, Desai R, Desai NC, Lohiya S, Bhargava G, Kumar K . School eye health appraisal. Indian J Ophthalmol 1989; 37 (4): 173–175.
Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP . Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ 2008; 86 (1): 63–70.
Naidoo KS, Jaggernath J . Uncorrected refractive errors. Indian J ophthalmol 2012; 60 (5): 432–437.
Smith K, Weissberg E, Travison TG . Alternative Methods of Refraction: A Comparison of Three Techniques. Optom Vis Sci 2010; 87 (3): E176–E182.
Berger IB, Spitzberg LA, Nnadozie J, Bailey N, Feaster J, Kuether C et al. Testing the FOCOMETER—A new refractometer. Optom Vis Sci 1993; 70 (4): 332–338.
Murthy G, Johnson GJ . The focometer: use in aphakic correction. Community Eye Health 1999; 12 (31): 43.
du Toit R, Soong K, Brian G, Ramke J . Quantification of refractive error: comparison of autorefractor and focometer. Optom Vis Sci 2006; 83: 582–588.
Paff T, Oudesluys-Murphy AM, Wolterbeek R, Swart-van den Berg M, de Nie JM, Tijssen E et al. Screening for refractive errors in children: the plusoptiX S08 and the Retinomax K-plus2 performed by a lay screener compared to cycloplegic retinoscopy. J AAPOS 2010; 14 (6): 478–483.
Chat SW, Edwards MH . Clinical evaluation of the Shin-Nippon SRW-5000 autorefractor in children. Ophthalmic Physiol Opt 2001; 21 (2): 87–100.
Allen PM, Radhakrishnan H, O'Leary DJ . Repeatability and validity of the PowerRefractor and the Nidek AR600-A in an adult population with healthy eyes. Optom Vis Sci 2003; 80 (3): 245–251.
The Official website of Oyo State Government. Available at http://www.oyostate.gov.ng/about-oyo-state/the-people/. Accessed on 22 December 2014.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Refractive errors and Refractive surgery; Preferred Practice Pattern Guildlines. American Academy of Ophthalmology; 2013. Available at www.aao.org/ppp. Accessed on 22 November 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Aina, A., Oluleye, T. & Olusanya, B. Comparison between focometer and autorefractor in the measurement of refractive error among students in underserved community of sub-Saharan Africa. Eye 30, 1496–1501 (2016). https://doi.org/10.1038/eye.2016.181
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.181